Understanding Buprenorphine: A Life-Saving Medication for Opioid Addiction
Buprenorphine is a prescription medication used to treat opioid use disorder (OUD) and manage chronic pain. Here’s a quick overview:
What it is:
- A partial opioid agonist, different from full opioids like heroin or fentanyl.
- Available as tablets, films, injections, and patches.
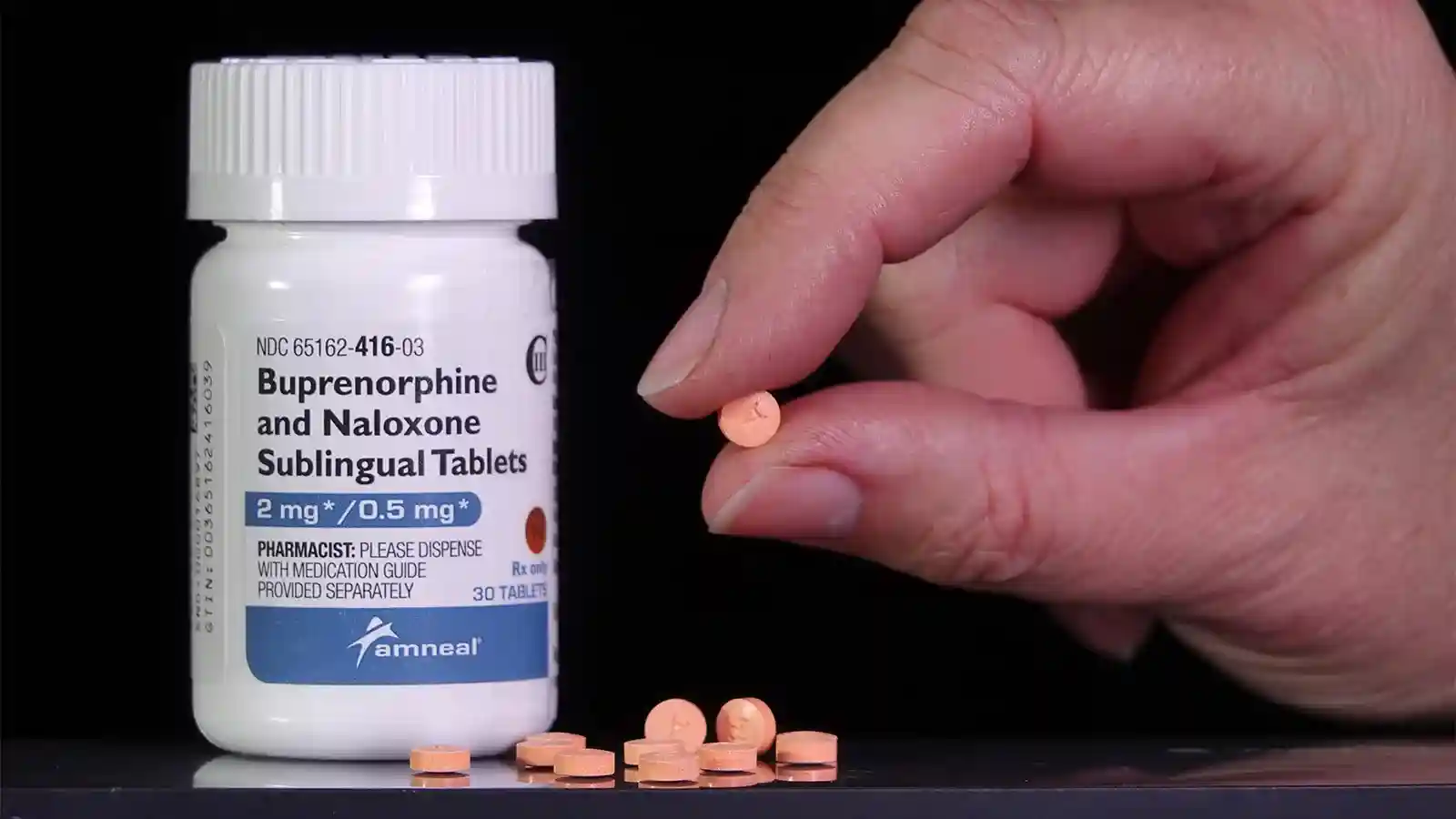
- Often combined with naloxone (e.g., Suboxone).
What it does:
- Reduces opioid cravings.
- Prevents withdrawal symptoms.
- Blocks the effects of other opioids.
- Has a “ceiling effect” that lowers overdose risk.
Common uses:
- Opioid addiction treatment (higher doses).
- Chronic pain management (lower doses).
- A key part of medication-assisted treatment (MAT).
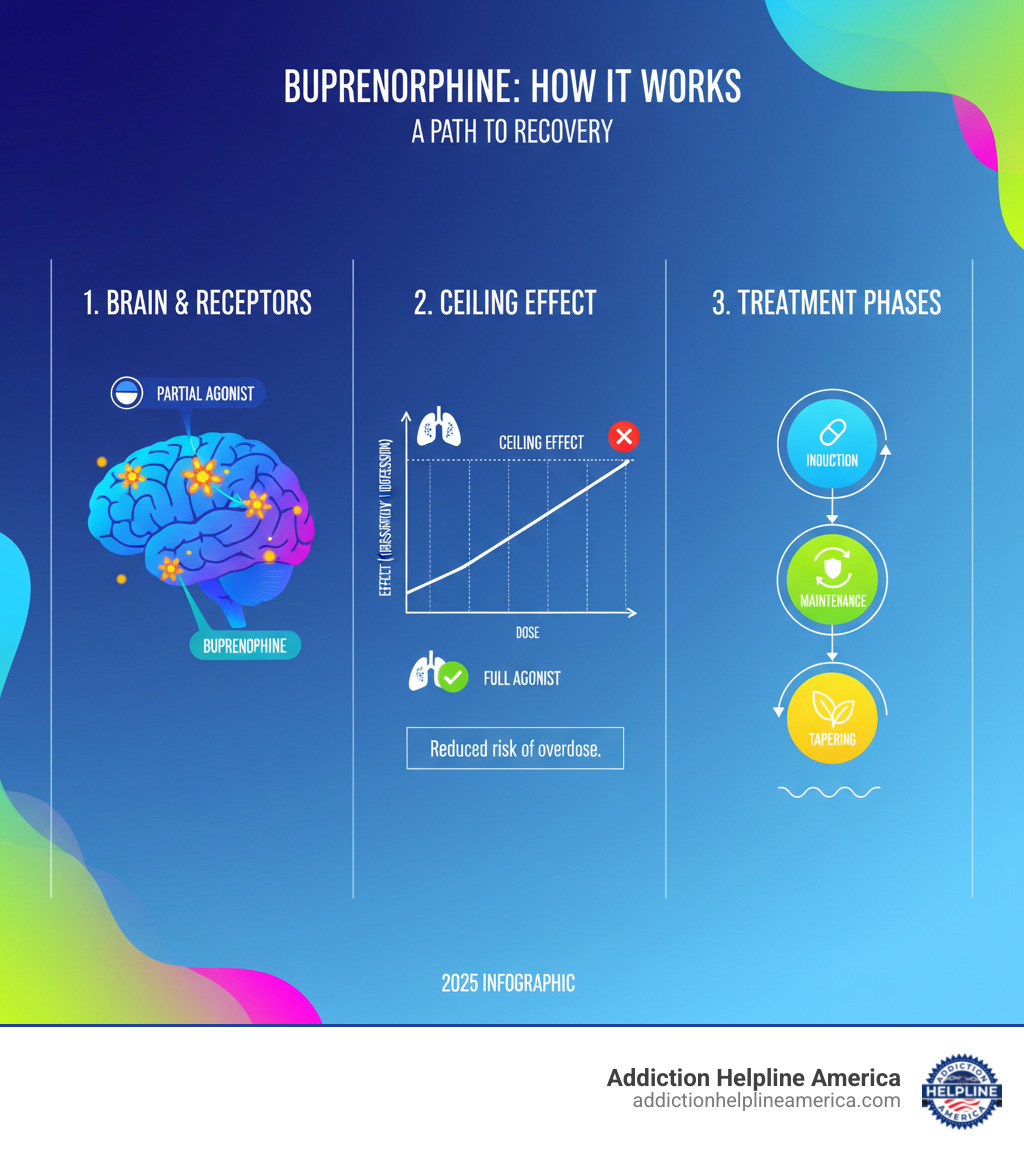
Unlike full opioids, buprenorphine only partially activates opioid receptors in the brain. This relieves cravings and withdrawal without producing an intense high, allowing people to stabilize and focus on recovery. Its “ceiling effect” means that after a certain dose, taking more does not increase the opioid effects, which dramatically lowers the risk of overdose compared to other opioids.
Treatment is personalized and typically moves through induction, maintenance, and sometimes tapering phases. At Addiction Helpline America, our 24/7 helpline can connect you with certified providers who prescribe this life-saving medication and guide you toward recovery.
What Is Buprenorphine and How Does It Work?
Buprenorphine is a key component of Medication-Assisted Treatment (MAT), which combines medication with counseling to effectively treat opioid use disorder. It works by stabilizing the brain chemistry that has been disrupted by addiction, giving you the clarity to focus on recovery.
Here’s how it works:
- Partial Agonist Action: It attaches to the same brain receptors as other opioids but only activates them partially. This relieves cravings and withdrawal symptoms without producing the intense high of full agonists like heroin or fentanyl.
- High Affinity: Buprenorphine binds very tightly to opioid receptors, pushing other opioids out and blocking their effects. This helps prevent relapse but also means the first dose must be timed carefully by a doctor to avoid “precipitated withdrawal” (a sudden onset of severe withdrawal symptoms).
- Ceiling Effect: After a certain dose, the medication’s effects plateau. This built-in safety feature makes the risk of fatal respiratory depression (slowed breathing) much lower than with methadone or illicit opioids.
- Long Half-Life: It remains effective for 24 hours or more, allowing for stable, once-daily dosing that helps you avoid the highs and lows that trigger cravings.
This unique combination of properties makes buprenorphine a safer, more stable option that allows people to live normal lives while in treatment. For more details on MAT, you can explore scientific research on Medication-Assisted Treatment from SAMHSA.
At Addiction Helpline America, our team is available 24/7 to help you understand your options and connect you with providers who can prescribe buprenorphine as part of a comprehensive recovery plan.
A Closer Look at Buprenorphine Treatment
Starting buprenorphine is a structured medical journey that requires a doctor’s prescription and supervision. Treatment typically involves three phases.

- Induction Phase: This is the transition from full opioids to buprenorphine. To avoid precipitated withdrawal, you must wait until you are in mild to moderate withdrawal before taking the first dose. A doctor will start you on a low dose and gradually increase it until symptoms are controlled.
- Maintenance Phase: Once on a stable dose, your cravings and withdrawal are managed. This allows you to focus on counseling and rebuilding your life. This phase can last for months or years, depending on your needs.
- Tapering Phase: If and when you and your doctor decide the time is right, you may slowly reduce your dose to eventually stop the medication. This is not a required step for everyone and should never be rushed.
Forms and Brand Names
Buprenorphine comes in several forms to suit different needs:
- Sublingual Tablets/Films (e.g., Suboxone, Subutex, Zubsolv): Placed under the tongue, this is the most common form for OUD treatment.
- Buccal Films (e.g., Belbuca): Placed inside the cheek, often used for chronic pain.
- Extended-Release Injections (e.g., Sublocade, Brixadi): A monthly or weekly injection given by a healthcare provider, eliminating the need for daily dosing.
- Transdermal Patches (e.g., Butrans): A skin patch that releases medication over several days for pain relief.
- Intravenous/Intramuscular Injections (e.g., Buprenex): Typically used in hospitals for acute pain.
More details on these forms are available through the FDA’s comprehensive resources.
Using buprenorphine for Pain vs. Addiction
The dose and form of buprenorphine differ depending on its use. For chronic pain, lower doses are used (often patches or buccal films) to provide steady pain relief. For opioid use disorder, higher doses are prescribed (usually sublingual films or injections) to block cravings and prevent withdrawal.
The Buprenorphine and Naloxone Combination
Many formulations, like Suboxone, combine buprenorphine with naloxone. Naloxone is an opioid blocker that is poorly absorbed when the medication is taken as directed (under the tongue). However, if someone tries to misuse the medication by injecting it, the naloxone becomes active and triggers immediate, unpleasant withdrawal symptoms. This clever combination serves as a built-in deterrent to misuse.
Buprenorphine vs. Methadone for Opioid Use Disorder
When considering Medication-Assisted Treatment (MAT), buprenorphine and methadone are the two primary options. Both are effective, but they have key differences in safety, side effects, and accessibility that may make one a better choice for your situation.

Key Differences in Safety and Side Effects
Buprenorphine‘s “ceiling effect” makes its overdose risk significantly lower than methadone, which is a full opioid agonist without this safety feature. While both can cause side effects like constipation and nausea, those associated with buprenorphine are generally milder. A crucial difference is that methadone can affect heart rhythm (QTc interval), a risk not associated with buprenorphine. Buprenorphine also has fewer drug interactions and allows for faster dose stabilization, often within days compared to weeks for methadone.
Prescribing and Accessibility
The biggest difference is how you get the medication. Methadone is highly restricted and typically requires daily visits to a specialized clinic. Buprenorphine offers far more flexibility.
In a transformative change, the federal “X-waiver” requirement for prescribing buprenorphine was eliminated in 2022. Now, any provider with a standard DEA license can prescribe it. This means you can get treatment from your primary care doctor, a local clinic, or via telehealth, making care more private and accessible.
Here’s a quick comparison:
| Feature | Buprenorphine | Methadone |
|---|---|---|
| How it works | Partial opioid agonist | Full opioid agonist |
| Overdose risk | Lower (ceiling effect) | Higher (no ceiling effect) |
| Side effects | Generally milder | Can be more intense |
| Heart effects | Minimal to none | Can affect heart rhythm |
| Drug interactions | Fewer interactions | More interactions |
| Time to stable dose | Days | Weeks |
| Who can prescribe | Any DEA-licensed doctor | Only certified OTP clinics |
| Where you get it | Doctor’s office, telehealth | Daily clinic visits |
| Take-home doses | Common, often weeks’ supply | Restricted, earned over time |
This increased accessibility for buprenorphine has opened doors to recovery for people across the country. Addiction Helpline America can help you find a local provider who can prescribe buprenorphine and support your recovery.
Risks, Interactions, and Important Warnings
While buprenorphine has a strong safety profile, it’s a powerful medication that requires careful management. Understanding the risks is key to using it safely.
- Central Nervous System (CNS) Depression: The main risk comes from mixing buprenorphine with other substances that slow brain function, such as alcohol, benzodiazepines (e.g., Xanax, Valium), or other sedatives. This combination can lead to severe respiratory depression, coma, or death.
- Liver Health: Your doctor will monitor your liver function, as buprenorphine is processed by the liver. It should be used with caution in people with liver problems and is generally avoided in cases of severe liver impairment.
- Precipitated Withdrawal: Taking buprenorphine too soon after using other opioids can trigger sudden, severe withdrawal. This is preventable by following your doctor’s instructions on when to start the medication.
- Pregnancy: Continuing buprenorphine during pregnancy is safer than returning to illicit opioid use. However, babies may be born with Neonatal Abstinence Syndrome (NAS), a treatable condition where the newborn experiences withdrawal.
Critical Drug Interactions
Be honest with your doctor about all medications and substances you use. The most dangerous interactions are with:
- Benzodiazepines and Alcohol: Combining these with buprenorphine is extremely dangerous and significantly increases the risk of fatal overdose.
- Other Sedatives: Sleep aids, muscle relaxants, and some antihistamines can amplify sedative effects.
- CYP3A4 Inhibitors/Inducers: Certain antibiotics, antifungals, and anti-seizure medications can affect how your body processes buprenorphine, requiring a dose adjustment by your doctor.
Common Side Effects
Most side effects are manageable and often improve over time. They include:
- Constipation
- Headache
- Nausea
- Drowsiness
- Dizziness
- Sweating
- Insomnia
- Pain at the injection site (for injectable forms)
Who Should Avoid buprenorphine?
Buprenorphine is not suitable for everyone. You should avoid it if you have:
- A known hypersensitivity or allergy to buprenorphine.
- Severe liver disease.
- Acute respiratory depression (severely slowed breathing).
Use with caution is required for individuals with severe lung disease (like COPD), head injuries, or acute alcoholism. A thorough medical evaluation is essential to ensure buprenorphine is a safe choice for you.
Frequently Asked Questions about Buprenorphine
Here are answers to some common questions about buprenorphine treatment.
Is buprenorphine just replacing one addiction with another?
No. Addiction is defined by compulsive, harmful drug use despite negative consequences. Buprenorphine treatment is therapeutic medical care. While it can cause physical dependence (meaning you would have withdrawal if you stopped suddenly), it does not cause the destructive behaviors of addiction. Instead, it normalizes brain chemistry, reduces cravings, and allows a person to regain control of their life and focus on recovery.
Can you overdose on buprenorphine?
It is very difficult to overdose on buprenorphine alone due to its “ceiling effect” on respiratory depression. However, the risk of a fatal overdose becomes extremely high when buprenorphine is mixed with other central nervous system depressants like alcohol or benzodiazepines (e.g., Xanax, Valium). Most buprenorphine-related deaths involve this kind of combination. Naloxone can reverse a buprenorphine overdose, but higher or repeated doses may be needed.
How long does buprenorphine withdrawal last?
Withdrawal from buprenorphine is generally milder than from heroin or fentanyl, but it lasts longer due to the medication’s long half-life. Symptoms may not start for 1-3 days and can last for several weeks, though the acute phase is shorter. The best way to avoid discomfort is to work with a doctor on a slow, medically supervised tapering plan. Never stop taking buprenorphine abruptly.
Conclusion
Buprenorphine is a transformative medication for treating opioid use disorder and managing chronic pain. Its unique properties as a partial opioid agonist with a “ceiling effect” make it a safer, highly effective option that stabilizes individuals, reduces cravings, and prevents withdrawal without the same risks as full opioids.
The recent elimination of the X-waiver has made this life-saving treatment more accessible than ever, allowing more doctors to prescribe it and more people to receive care in a familiar setting. It reduces stigma and treats addiction as the medical condition it is.
While buprenorphine requires medical supervision, it provides a foundation for lasting recovery. It allows people to be present for their families, return to work, and rebuild their lives. It doesn’t just save lives—it restores them.
At Addiction Helpline America, we have seen the profound impact of this treatment. Our team is available 24/7 to offer free, confidential support and connect you with certified providers in your area. Recovery is possible, and you don’t have to find the path alone.
Find confidential help for opioid addiction today. We’re here to help you take the first step.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.












