Understanding Bipolar Disorder and the Essential Role of Psychotherapy
Bipolar disorder psychotherapy is a vital component of treatment that works alongside medication to help individuals manage extreme mood swings and improve daily functioning. This lifelong condition affects approximately 5.7 million adult Americans (about 2.6% of the U.S. population), causing intense shifts in mood, energy, and behavior. While medication is essential for managing the biological aspects of the illness, it often provides only partial symptom relief. This is where psychotherapy becomes crucial, offering practical skills for the day-to-day challenges of living with bipolar disorder.
Key Benefits of Psychotherapy for Bipolar Disorder:
- Faster Recovery: Individuals in intensive psychotherapy with medication were 1.58 times more likely to be clinically stable than those receiving only medication and brief education.
- Reduced Depression: People in structured group psychoeducation spent 75% less time depressed at a 5-year follow-up compared to those in unstructured groups.
- Better Medication Adherence: Therapy helps address the 25-68% nonadherence rates common in bipolar disorder.
- Improved Functioning: Evidence-based therapies help manage the persistent psychosocial and interpersonal challenges of the condition.
- Relapse Prevention: Regular therapy helps identify early warning signs and prevent episodes from worsening.
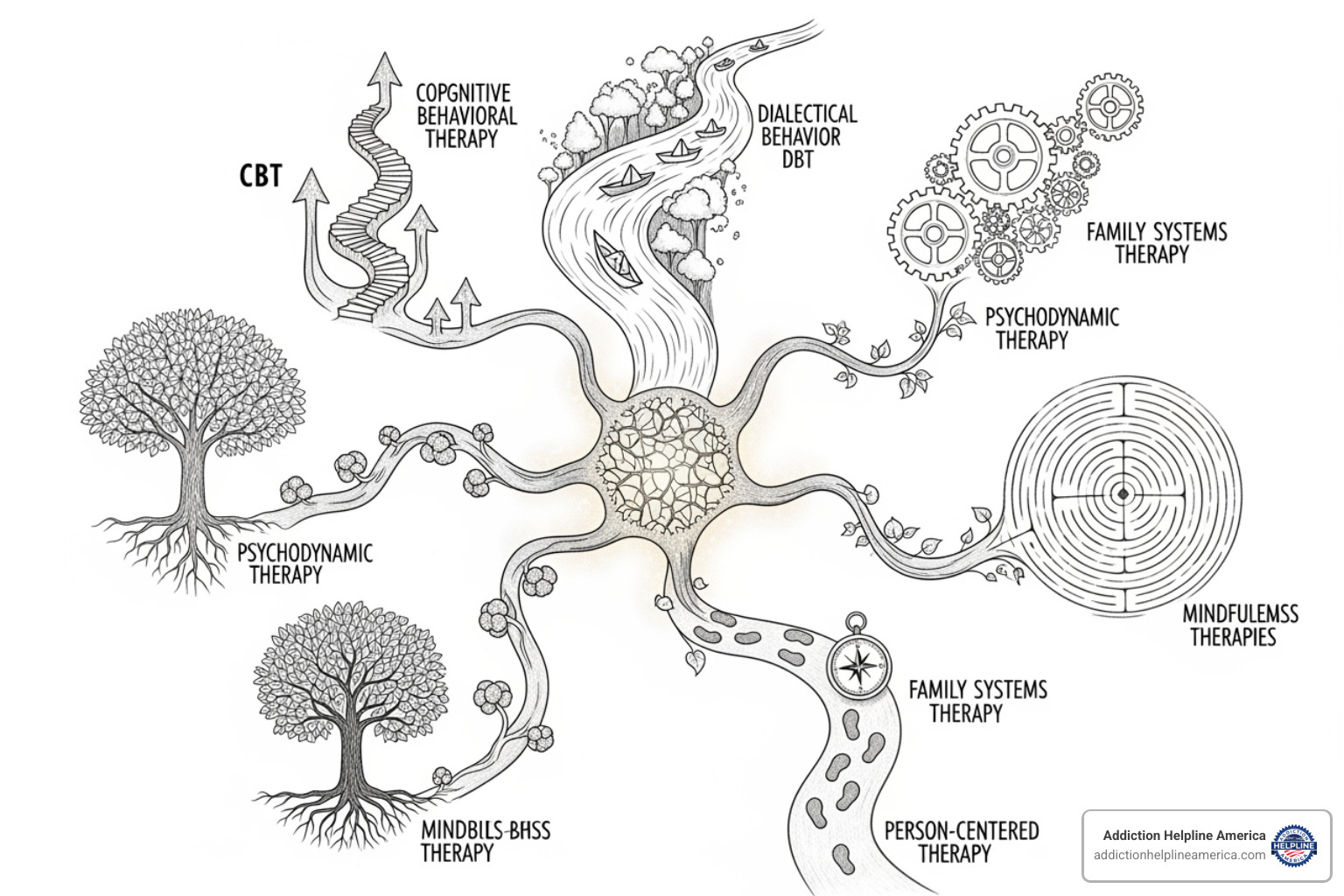
Several evidence-based approaches have proven effective, including Cognitive Behavioral Therapy (CBT), Family-Focused Therapy (FFT), and Interpersonal and Social Rhythm Therapy (IPSRT). Each addresses different aspects of the condition, from challenging negative thought patterns to stabilizing daily routines.
The challenge is often compounded by co-occurring conditions. The lifetime prevalence of PTSD among individuals with bipolar disorder is as high as 40%, and an estimated 60% have a history of drug or alcohol dependence. These complexities demand comprehensive treatment that addresses the whole person.
At Addiction Helpline America, we understand the critical intersection between mental health and substance use. We recognize that effective bipolar disorder psychotherapy is essential for lasting recovery and connect people with the specialized resources they need.
This guide will walk you through how psychotherapy works, which approaches are most effective, and how to access care. Understanding your options is a crucial step toward stability and an improved quality of life.
Important bipolar disorder psychotherapy terms:
The Cornerstone of Treatment: How Psychotherapy Stabilizes Bipolar Disorder
While mood stabilizers and other medications are essential for treating bipolar disorder, especially during acute episodes, medication alone rarely provides a complete solution. The most effective treatment combines medication with bipolar disorder psychotherapy. This adjunctive approach addresses both the biological aspects of the illness and the practical skills needed to steer relationship struggles, work difficulties, and social complications.
Research consistently shows that combining psychotherapy with medication leads to faster recovery and better long-term outcomes. The landmark STEP-BD study found that people receiving intensive psychotherapy were 1.58 times more likely to achieve clinical stability compared to those who only took medication with brief education. This is particularly important for depression, which is the most common and disabling aspect of bipolar disorder. For those with Bipolar I, depressive episodes can be three times more frequent than manic ones; for Bipolar II, that number jumps to 39 times more frequent.
What is Psychotherapy and How Does It Help?
Often called “talk therapy,” psychotherapy is a structured process where a mental health professional helps you identify and work through problems related to your condition. You’ll gain a deeper understanding of your illness, learn to recognize episode triggers, and see how your thoughts, feelings, and behaviors are connected. The relationship you build with your therapist—the “therapeutic alliance”—is a powerful healing force, creating a safe space for honesty and growth.
Therapy helps you manage symptoms, prevent relapse by catching warning signs early, and build a personal toolbox of coping strategies for stress and emotional regulation. These are practical skills that make a real difference in your daily life.
Improving Medication Adherence and Quality of Life
Taking medication consistently is a major challenge, with nonadherence rates between 25% and 68%. Therapy provides a space to have honest conversations about medication challenges and side effects. Through psychoeducation, your therapist explains why medications are necessary, which helps you stay committed to your treatment plan. Techniques like motivational interviewing can also help you find your own reasons for wanting to stay well.
Beyond medication, therapy improves your overall quality of life by helping you manage psychosocial challenges. By learning better interpersonal and communication skills, you can reduce conflict, build a stronger support network, and regain stability in your career and personal relationships.
At Addiction Helpline America, we connect people with treatment programs that specialize in evidence-based approaches for bipolar disorder, ensuring that both the medication and therapy components work together for lasting recovery.
Evidence-Based Approaches in Bipolar Disorder Psychotherapy
Several evidence-based therapies have proven effective for bipolar disorder, but there is no single “best” approach for everyone. The most effective treatment is one that fits your specific needs and preferences. Think of these therapies as different tools designed to address different aspects of the condition, from thought patterns to daily routines to family relationships.
Cognitive and Behavioral Approaches
Cognitive Behavioral Therapy (CBT) is one of the most well-researched forms of bipolar disorder psychotherapy. It operates on the principle that our thoughts, feelings, and behaviors are interconnected. During a depressive episode, CBT helps you identify and challenge distorted thoughts like “I’m worthless,” which fuel feelings of hopelessness. For manic episodes, it teaches you to recognize inflated thoughts as symptoms, not reality, leading to better judgment. A key component is behavioral activation, which involves gradually re-engaging with meaningful activities to counteract the withdrawal of depression. Research shows CBT is highly effective for managing depressive symptoms and lowering relapse rates.
Interpersonal and Routine-Focused Strategies
Interpersonal and Social Rhythm Therapy (IPSRT) is designed specifically for bipolar disorder and is based on the insight that disruptions in daily routines can trigger mood episodes. The therapy focuses on stabilizing your daily schedules for sleeping, eating, and other activities to regulate your body’s internal clock, or circadian rhythms. A key concept is “social zeitgebers”—the regular social cues like meals and work schedules that anchor your internal clock. The “interpersonal” component of IPSRT helps you identify and resolve relationship problems that cause stress and trigger mood shifts, teaching better communication and problem-solving skills.
Family Involvement and Support
Family-Focused Therapy (FFT) acknowledges that bipolar disorder affects the entire family and brings loved ones directly into the treatment process. It typically begins with psychoeducation, where the family learns about the illness, its symptoms, and its causes. This understanding helps reduce conflict and allows family members to recognize early warning signs. A major part of FFT is communication training, which teaches families to express emotions constructively and avoid destructive patterns like criticism or avoidance. The therapy also equips the family with problem-solving skills to work as a team in managing the practical challenges of the illness. Research shows FFT significantly improves outcomes by reducing family stress.
Skills for Emotional Regulation
For those who struggle with intense emotional swings and impulsivity, Dialectical Behavior Therapy (DBT) can be particularly helpful. DBT teaches concrete skills in four main areas: mindfulness (observing thoughts and feelings without judgment), distress tolerance (surviving crises without making them worse), emotion regulation (understanding and reducing the intensity of difficult emotions), and interpersonal effectiveness (asking for what you need and setting healthy boundaries). Another approach, Mindfulness-Based Cognitive Therapy (MBCT), combines mindfulness with CBT to help you gain a more detached perspective on your thoughts, reducing the rumination that often accompanies depression.
Key Skills for Managing Bipolar Disorder in Daily Life
Effective bipolar disorder psychotherapy equips you with practical tools to become an active participant in your own stability. These skills help you build resilience and proactively manage challenges before they escalate into full-blown episodes.
The Power of Psychoeducation: Individual vs. Group Settings
Understanding your illness is the first step toward managing it. Psychoeducation teaches you about the biological basis of bipolar disorder, what triggers episodes, and how treatments work. This can happen in individual therapy, but group psychoeducation offers the unique power of shared experience, reducing the isolation and stigma that often accompany the condition. The research is compelling: one 5-year study found that individuals who participated in structured group psychoeducation spent 75% less time depressed compared to those in unstructured support groups.
Recognizing Early Warning Signs and Managing Episodes
Most mood episodes are preceded by subtle early warning signs, or prodromal symptoms. Therapy helps you identify your personal signs, such as changes in sleep, energy, or thought patterns. You’ll then create a personalized wellness plan—a clear roadmap for what to do when these signs appear, such as contacting your therapist or adjusting your routine. Mood monitoring, using a journal or app to track your sleep, mood, and energy, helps you and your therapist identify patterns and triggers. This proactive approach, combined with a crisis plan for severe episodes, empowers you to manage your condition effectively.
Coping with Stress, Trauma, and Co-Occurring Conditions
Stress is a major trigger for mood episodes, making stress management techniques an essential part of therapy. You’ll learn practical relaxation, problem-solving, and cognitive strategies to handle life’s pressures. However, bipolar disorder rarely travels alone. Up to 40% of people with bipolar disorder also have PTSD, and an estimated 60% struggle with substance use. If you have Bipolar I, you are 5.8 times more likely to develop a substance use disorder.
These co-occurring conditions require integrated treatment. Trauma-informed therapy can help you process past experiences safely, while dual diagnosis programs address substance use and bipolar disorder simultaneously. At Addiction Helpline America, we specialize in connecting people to these integrated programs, understanding that you cannot successfully treat one condition without addressing the other.
Access, Support, and the Future of Treatment
While we know that bipolar disorder psychotherapy is effective, accessing quality care can be challenging. The good news is that the landscape of mental health treatment is evolving, with new ways to overcome traditional barriers.
Overcoming Barriers to Accessing Bipolar Disorder Psychotherapy
Many people face significant problems when seeking help. These often include:
- Cost: Therapy can be expensive, even with insurance.
- Stigma: Fear of judgment from family, friends, or employers prevents many from seeking treatment.
- Finding a Specialist: Therapists trained in evidence-based approaches for bipolar disorder can be difficult to find, especially outside of major cities.
- Geographic and Insurance Problems: Living in a rural area or navigating complex insurance plans can make accessing care feel overwhelming.
At Addiction Helpline America, we help people steer these challenges every day, connecting them with treatment options across states like Alabama, Arizona, California, Florida, and more.
The Rise of Telehealth and Digital Support
Telehealth has revolutionized access to mental health care. Video therapy sessions allow you to connect with a specialized therapist regardless of your location. In addition, digital tools can supplement your treatment:
- Smartphone apps provide psychoeducational content and guided exercises for coping skills.
- Mood tracking technology helps you and your therapist monitor patterns and triggers with greater accuracy.
- Web-based programs offer structured self-management resources.
While these tools are powerful additions, they work best alongside the guidance and human connection of a skilled therapist.
The Role of Support Groups and Community in Bipolar Disorder Psychotherapy
Support groups offer a unique form of healing: connection with peers who truly understand your experience. In these groups, led by professionals or trained peers, you can share struggles and victories without fear of judgment. This shared experience reduces isolation and provides practical wisdom. Organizations like the Depression and Bipolar Support Alliance (DBSA) offer peer-led groups that can be an invaluable part of a comprehensive treatment plan.
Family support groups are also crucial, giving loved ones a space to learn, share concerns, and develop coping strategies. This reduces household stress and creates a more supportive environment for the person with bipolar disorder. When professional therapy isn’t immediately available, peer support can provide meaningful help and a connection to vital community resources.
Conclusion
Bipolar disorder psychotherapy is not just a helpful add-on; it is an essential partner to medication that can transform your life. While medication addresses the biological roots of the illness, psychotherapy provides the skills and resilience needed to steer its daily challenges.
We’ve seen how different therapies—like CBT, IPSRT, FFT, and DBT—offer unique tools for managing thoughts, routines, relationships, and emotions. The research is clear: combining therapy with medication leads to higher rates of clinical stability and significantly less time spent in depressive episodes. Therapy is also critical for improving medication adherence, which is a common struggle for 25-68% of individuals.
Furthermore, with high rates of co-occurring conditions like PTSD (up to 40%) and substance use disorders (around 60%), integrated treatment that addresses the whole person is paramount. At Addiction Helpline America, we specialize in connecting people to care that treats both mental health and substance use issues simultaneously.
While barriers like cost, stigma, and access are real, the rise of telehealth and the power of support groups are creating more pathways to care than ever before. The most important step is finding an approach and a therapist that you trust.
Living with bipolar disorder is challenging, but stability, recovery, and an improved quality of life are absolutely within reach. You don’t have to steer this journey alone.
At Addiction Helpline America, we are committed to providing free, confidential guidance to help you find specialized mental health and addiction treatment resources across the nation. Reach out today to take the next step toward stability and hope.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.