
Understanding Bipolar Disorder 2 Treatment: Your Path Forward
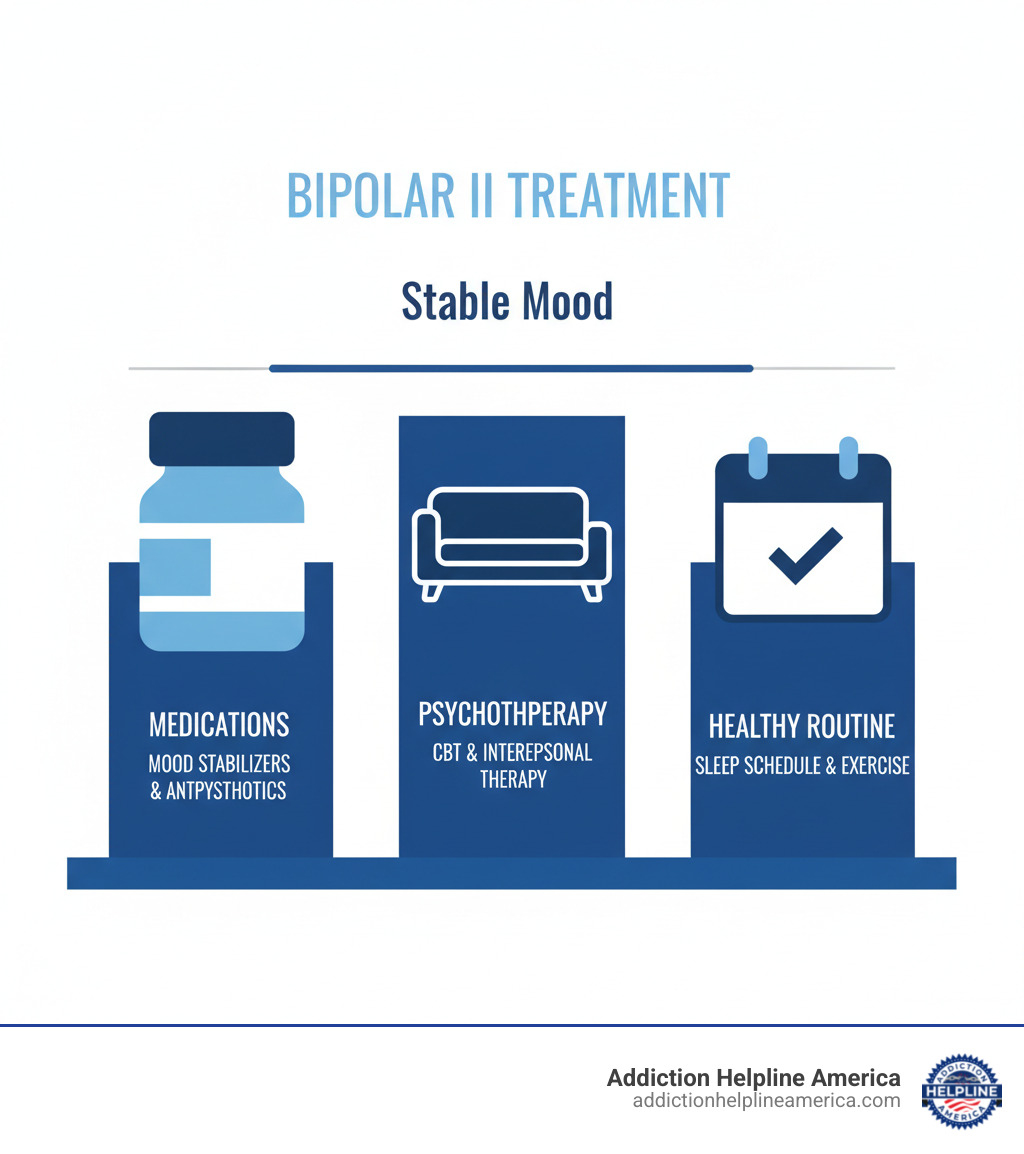
Bipolar disorder 2 treatment involves a combination of medication, psychotherapy, and lifestyle management. This lifelong approach is essential for stability, but with consistent care, most people with Bipolar II live fulfilling lives.
Quick Overview of Bipolar II Treatment Options:
| Treatment Category | First-Line Options | Purpose |
|---|---|---|
| Medications | Quetiapine, Lithium, Lamotrigine | Stabilize mood, prevent episodes |
| Psychotherapy | CBT, Interpersonal Therapy, Family Therapy | Build coping skills, manage triggers |
| Lifestyle Changes | Regular sleep schedule, stress management, exercise | Support mood stability, reduce relapse risk |
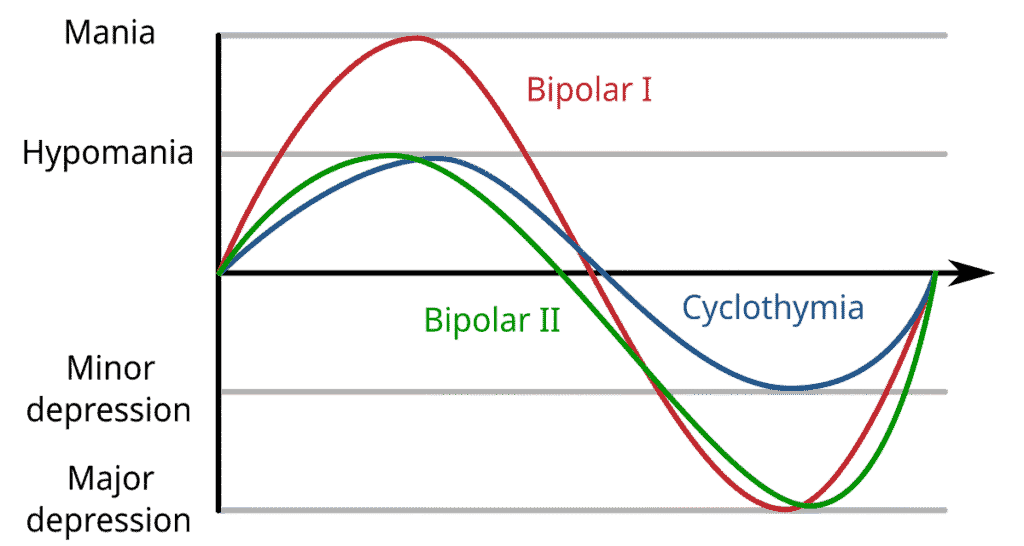
Bipolar II disorder is defined by hypomanic episodes (liftd moods lasting at least four days) and major depressive episodes. Unlike Bipolar I’s full manic episodes, the primary challenge in Bipolar II is often the more frequent and longer-lasting depressive episodes.
This makes treatment difficult. Hypomania can feel productive or enjoyable, so many people don’t see it as a problem. This contributes to an average 12-year delay in accurate diagnosis and care. Without proper treatment, the depressive episodes can be debilitating, and the relapse rate is over 70% within five years.
With personalized, consistent treatment, you can achieve euthymia—a stable, balanced mood. The right plan depends on your symptoms, medication response, lifestyle, and any co-occurring conditions like anxiety or substance use disorders.
Addiction Helpline America connects individuals with comprehensive mental health resources, including specialized programs for bipolar disorder 2 treatment. Our team can guide you through every available option, especially when co-occurring substance use is a concern.
Bipolar disorder 2 treatment terms you need:
Differentiating Treatment: Bipolar I vs. Bipolar II
While both Bipolar I and II involve mood swings, their differences are critical for treatment. The main distinction is that Bipolar I involves full-blown manic episodes, while Bipolar II features less severe hypomanic episodes. However, Bipolar II is not a “milder” version; people with Bipolar II often spend three times more days depressed than those with Bipolar I, and these depressive episodes can be just as debilitating.
For both conditions, the goal is euthymia—a balanced, stable mood. Achieving this requires an accurate diagnosis and a treatment plan customized to your specific type of bipolar disorder.
Key Differences in Treatment Approaches
For bipolar disorder 2 treatment, the focus shifts compared to Bipolar I. With Bipolar I, controlling severe mania is the priority, often requiring aggressive medication strategies and sometimes hospitalization. For Bipolar II, the primary challenge is usually managing the frequent and long-lasting depressive episodes.
This is where treatment gets tricky, especially concerning antidepressants. In Bipolar I, antidepressants are used with extreme caution as they can trigger dangerous manic episodes or rapid cycling. They are almost never prescribed without a mood stabilizer.
For bipolar disorder 2 treatment, the risk of an antidepressant inducing hypomania is lower but still significant. While some doctors may prescribe them alone with close monitoring, most experts recommend using them only in combination with a mood stabilizer or atypical antipsychotic. As this scientific research on Bipolar I and II treatment differences notes, medication choices and doses are adjusted based on whether the primary target is severe mania or persistent depression.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Targeting Specific Mood Episodes
Effective bipolar disorder 2 treatment addresses each type of mood episode.
Managing Acute Hypomania: Though you may feel good, hypomania can lead to impulsive decisions. Your doctor might use mood stabilizers like lithium or divalproex, or an atypical antipsychotic to prevent escalation. If you’re on an antidepressant, it may be stopped.
Treating Bipolar Depression: This is often the toughest part of Bipolar II. Quetiapine is a common first-line medication. Other options include lurasidone, cariprazine, or lamotrigine. The goal is to lift depression without triggering hypomania.
Preventing Antidepressant-Induced Switching: If antidepressants are used, your team will monitor you closely for signs of mood elevation. Combining them with a mood stabilizer helps reduce this risk.
Mood Stabilization: This is the primary long-term goal. Stability prevents future episodes and disruptions to your work, relationships, and well-being.
Rapid Cycling: If you have four or more mood episodes in a year, your plan may need adjustment. Lamotrigine has shown benefits for rapid cycling, and strict medication adherence is critical.
Addiction Helpline America helps you find specialized treatment programs that understand the specific needs of Bipolar II and can provide the personalized care you deserve.
Medication: The Cornerstone of Bipolar Disorder 2 Treatment
Medication is essential for bipolar disorder 2 treatment. As a biological condition affecting brain chemistry, bipolar disorder requires medications to help balance the neurotransmitters that regulate mood. For most, this means lifelong medication to prevent depressive episodes and manage hypomania, allowing for a stable, fulfilling life.

Finding the right medication regimen takes patience and personalization. Your doctor may need to adjust doses or try different options, as what works for one person may not work for another. Combination therapy—using a mood stabilizer with an antipsychotic, for example—is common. Regular monitoring, including blood work for certain medications, is a crucial safety measure. Most importantly, medication adherence is key; stopping your medication when you feel better is a common cause of relapse.
Key Medication Classes Used in Treatment
Your doctor might prescribe medications from the following classes for bipolar disorder 2 treatment.
Mood Stabilizers: These are the foundation of treatment, preventing both depressive and hypomanic episodes. Lithium is the oldest and most proven option, known for reducing suicide risk. Lamotrigine (Lamictal) is a go-to for Bipolar II as it’s effective at preventing depression. Other options include anticonvulsants like valproic acid/divalproex sodium (Depakote) and carbamazepine (Tegretol).
Atypical Antipsychotics: These have powerful mood-stabilizing properties. Quetiapine (Seroquel) and lurasidone (Latuda) are highly effective for bipolar depression. Other common options include cariprazine (Vraylar), olanzapine (Zyprexa), aripiprazole (Abilify), and the olanzapine-fluoxetine combination (Symbyax).
Antidepressants: These are used cautiously due to the risk of triggering hypomania. They are almost always prescribed alongside a mood stabilizer or antipsychotic. You can learn more in our article on bipolar disorder and antidepressants.
For a comprehensive look at options, see our guide on a drug for bipolar disorder.
Understanding and Managing Medication Side Effects
Side effects are a frustrating but often manageable part of treatment. Honest communication with your doctor is key.
Weight Gain and Metabolic Changes: Common with many antipsychotics. Your doctor should monitor your weight, blood sugar, and cholesterol. Lifestyle changes and medication adjustments can help.
Drowsiness or Sedation: Often improves over time. Taking medication at bedtime can minimize daytime sleepiness.
Gastrointestinal Issues: Nausea or upset stomach can often be managed by taking medication with food.
Tremors: Fine hand tremors are common with lithium. Your doctor can adjust the dose if they become bothersome.
Akathisia: An intense feeling of inner restlessness. Report this to your doctor immediately, as it is highly distressing but treatable.
Tardive Dyskinesia: A serious risk of long-term antipsychotic use involving involuntary movements. Regular screening is essential for early detection.
Certain medications require special considerations. Lithium requires blood tests to monitor levels and careful management of salt and fluid intake, as explained in resources like this one on managing diet with certain medications. Medications like valproate and carbamazepine carry risks during pregnancy. Lamotrigine requires a slow dose increase (titration) to reduce the risk of a serious rash.
The goal is to find an effective bipolar disorder 2 treatment with tolerable side effects. At Addiction Helpline America, we connect people with programs that take the time to get this balance right.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Beyond Medication: Psychotherapy and Lifestyle Strategies
Medication alone is not enough for effective bipolar disorder 2 treatment. Psychotherapy is an essential partner to medication, teaching you the skills to live with the condition. It helps you develop coping mechanisms, understand your triggers, improve relationships, and manage daily stressors. Combining therapy with medication significantly lowers relapse rates and gives you a greater sense of control.
Effective Talk Therapies for your Bipolar Disorder 2 Treatment Plan
Several types of therapy are proven to be effective for bipolar disorder:
Cognitive Behavioral Therapy (CBT): Helps you identify and change negative thought patterns and behaviors that can worsen mood episodes.
Interpersonal and Social Rhythm Therapy (IPSRT): Focuses on stabilizing daily routines—especially sleep, meals, and social activity—to help regulate your biological rhythms and mood.
Family-Focused Therapy (FFT): Involves family members in treatment to improve communication, education, and support, creating a team approach to managing the condition.
Dialectical Behavior Therapy (DBT): Teaches skills in mindfulness, emotional regulation, and distress tolerance, which is especially helpful for managing intense emotions.
Psychoeducation: Woven into all effective therapy, this involves learning about your condition, its symptoms, and treatment strategies to empower you to make informed decisions.
Building a Supportive Daily Routine and Lifestyle

Your daily habits are fundamental tools in your bipolar disorder 2 treatment plan. These strategies can make the difference between stability and relapse.
Sleep Hygiene: This is non-negotiable. Go to bed and wake up at the same time every day, even on weekends, to prevent triggering mood episodes.
Consistent Daily Routines: Regular meal times and activity schedules help regulate your biological clock and support mood stability.
Stress Management: Learn techniques like deep breathing, yoga, or meditation to cope with stress, a major trigger for mood episodes.
Regular Exercise: Acts as a natural mood stabilizer. Even a 30-minute walk most days can improve symptoms of depression and anxiety.
Balanced Nutrition: Eating regular, nutritious meals helps stabilize your energy and mood. If taking lithium, discuss fluid and salt intake with your doctor.
Avoiding Alcohol and Recreational Drugs: Substance use worsens bipolar symptoms, interferes with medication, and increases relapse risk. An estimated 60% of people with bipolar disorder also have a substance use disorder, making integrated treatment essential.
Mood Tracking: Using an app or journal to record moods, sleep, and energy levels helps you and your doctor identify patterns and potential triggers.
Healthy Relationships: A strong support system of understanding family and friends can provide encouragement and help you spot early warning signs.
At Addiction Helpline America, we connect you with holistic treatment programs that help you build the daily habits and support systems needed for long-term recovery.
Navigating Crises and Co-Occurring Conditions
Managing bipolar disorder often involves navigating other mental health challenges and substance use issues. When these conditions overlap (a dual diagnosis), bipolar disorder 2 treatment becomes more complex but also more critical. Integrated care that addresses all interconnected challenges is the most effective approach.
Integrating Substance Abuse Care with Bipolar Disorder 2 Treatment
Approximately 60% of people with bipolar disorder also struggle with a substance use disorder. Many turn to drugs or alcohol to self-medicate the pain of depression or the restlessness of hypomania. However, this provides only temporary relief and ultimately worsens mood instability, interferes with medication, and increases relapse risk. Substances can also trigger mood episodes and have dangerous interactions with psychiatric medications.
Integrated treatment programs are vital because they treat both conditions simultaneously. Sobriety is fundamental to mood stability; when the brain isn’t dealing with the chaos of substance use, medications and therapy are far more effective.
At Addiction Helpline America, our mission is to connect people to comprehensive dual diagnosis care. We can guide you to specialized programs that address both mental health and substance use. If you’re navigating this challenge, exploring Substance Abuse Treatment is a crucial step.
Intensive Treatment Options for Severe Symptoms
While most bipolar disorder 2 treatment is outpatient, severe symptoms may require more support. Severe depression is a primary concern in Bipolar II, as as many as 1 in 5 people with bipolar disorder die by suicide. When safety is at risk due to suicidal thoughts or psychotic features, intensive treatment is necessary.
Partial Hospitalization Programs (PHP): Offer structured, all-day treatment 5-7 days a week while you return home at night. This is a step-down from inpatient care or a step-up from standard outpatient.
Intensive Outpatient Programs (IOP): Provide structured group and individual therapy for several hours, 3-4 days a week, allowing you to maintain some daily responsibilities.
Inpatient Hospitalization: Necessary for acute crises, providing 24/7 supervision in a safe environment to stabilize symptoms and adjust medication. You can learn more about In Patient Rehab For Depression.
For treatment-resistant depression, other options like Electroconvulsive Therapy (ECT), Repetitive Transcranial Magnetic Stimulation (rTMS), and ketamine treatment may be considered.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Treating Bipolar Disorder in Children and Teens
When bipolar disorder appears in adolescence or childhood, it requires a specialized approach. Distinguishing symptoms from normal moodiness is a major diagnostic challenge. Co-occurring conditions like ADHD and anxiety can further complicate the picture.
Medication safety is a top concern, as there is less research on its effects on developing brains. Family therapy is crucial, as it helps the entire family unit understand the illness, improve communication, and support the young person. School accommodations through IEP or 504 plans are also vital to ensure academic success. The goal is to manage current symptoms while building the emotional regulation and coping skills needed for adulthood. If substance use is also a factor, specialized Adolescent Substance Abuse programs are essential.
The Long-Term Outlook and Finding Consistent Care
Bipolar disorder is a chronic condition that requires lifelong management, similar to diabetes or heart disease. While this may sound daunting, the hopeful reality is that with consistent, appropriate bipolar disorder 2 treatment, you can live a full and meaningful life.
Statistics highlight the importance of treatment. Without it, over 70% of people with bipolar disorder relapse within five years. Untreated bipolar disorder is also linked to a nine-year reduction in expected life span and a high suicide risk, with 1 in 5 people dying by suicide. These outcomes are not inevitable; they represent the risks of an unmanaged condition.
With a personalized plan combining medication, therapy, and lifestyle adjustments, the outlook changes dramatically. The goal of bipolar disorder 2 treatment is not just to prevent episodes but to thrive—engaging in fulfilling work, nurturing relationships, and caring for your overall health. Consistency is key, including regular check-ins with your psychiatrist and therapist to ensure your treatment remains safe and effective.
At Addiction Helpline America, we have helped thousands of people steer the complexities of mental health and substance use disorders. We know finding the right care is overwhelming, and we are here to provide free, confidential guidance. Our team can connect you with specialized bipolar disorder 2 treatment programs across the country, from Alabama to Wyoming.
We believe in the power of recovery. Bipolar disorder is manageable, and stability is possible. Let us help you take the next step. Find a personalized mental health treatment program that meets you where you are and supports you in building the stable, fulfilling life you deserve. You don’t have to steer this journey alone.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.





