Finding Your Way: The Best Solutions for Depression
Finding the best solution for depression can feel overwhelming, but you’re not alone. Nearly 7% of U.S. adults experience depression annually, and about 1 in 6 will in their lifetime. The good news is that treatment is highly effective, with 80% to 90% of people responding well to it.
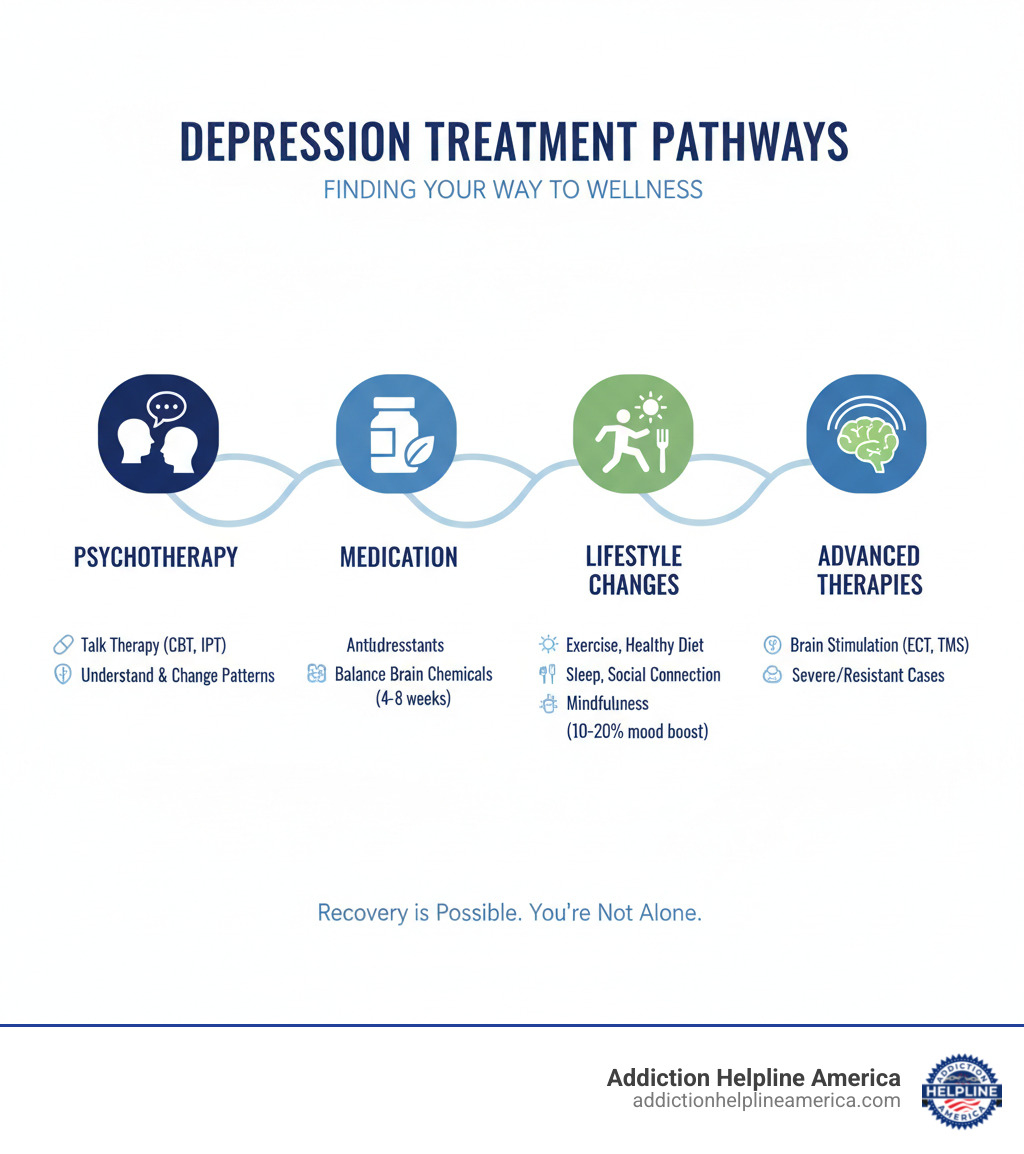
While there’s no single path for everyone, effective strategies often include:
- Psychotherapy (Talk Therapy): Therapies like Cognitive Behavioral Therapy (CBT) or Interpersonal Therapy (IPT) help change negative thought patterns.
- Antidepressant Medications: These help balance brain chemicals and typically take 4-8 weeks to work.
- Lifestyle Changes: Regular exercise, a healthy diet, good sleep, and social connection can significantly improve mood.
- Mindfulness Meditation: Focusing on the present can reduce symptoms by 10-20%.
- Brain Stimulation Therapies: ECT and TMS are options for severe or treatment-resistant cases.
Depression is a medical condition that affects how you think, feel, and act, but it doesn’t have to define your future. This guide will help you understand the condition and explore proven ways to find relief.
At Addiction Helpline America, we know how crucial finding the best solution for depression is for well-being. Our team guides individuals toward effective treatment options, empowering them to reclaim their lives.
Easy best solution for depression glossary:
Understanding Depression: Signs, Types, and Causes
Depression is a complex mood disorder, not just a feeling of sadness. It involves a persistent low mood and loss of interest in activities, affecting your thoughts, feelings, and daily life. It can affect anyone, with women diagnosed more often than men and about 4.4% of U.S. children experiencing it.
This condition appears in many forms, from Major Depressive Disorder (MDD) to Persistent Depressive Disorder (dysthymia), Seasonal Affective Disorder (SAD), and Perinatal Depression. The causes are varied, often involving a mix of brain chemistry, genetics, and life events. Understanding depression as a Behavioral Disorder is a helpful step toward finding solutions.
Recognizing the Telltale Signs and Symptoms
Spotting the signs of depression early can make a huge difference. If you notice five or more of these symptoms daily for at least two weeks, it may indicate depression, especially if one symptom is a depressed mood or loss of interest.
Common clues include:
- A persistent sad, anxious, or empty mood.
- A noticeable loss of interest or pleasure (anhedonia) in most activities.
- Sleep changes, such as insomnia (trouble sleeping) or hypersomnia (sleeping too much).
- Appetite or weight changes, like significant weight loss or gain without trying.
- Profound fatigue or feeling drained, even after rest.
- Powerful feelings of worthlessness or guilt without a clear reason.
- Difficulty concentrating, remembering things, or making decisions.
- Thoughts of death or suicide. This is a serious symptom. Depression contributes to nearly 40,000 suicides each year in the U.S. If you or someone you know has these thoughts, please seek help immediately.
The Many Faces of Depression: Understanding the Types
Depression isn’t one-size-fits-all. Understanding the specific type helps tailor the most effective treatment plan—the true best solution for depression for an individual.
Common forms include:
- Clinical Depression (Major Depressive Disorder – MDD): Severe symptoms that interfere with daily life, lasting at least two weeks.
- Persistent Depressive Disorder (Dysthymia): A milder but chronic form of depression, with symptoms lasting at least two years.
- Bipolar Disorder Depression: Periods of deep lows (depression) alternating with periods of liftd mood (mania or hypomania).
- Premenstrual Dysphoric Disorder (PMDD): A severe form of PMS with significant mood swings and irritability before menstruation.
- Atypical Depression: Mood may improve with positive events, but other symptoms include increased appetite, excessive sleep, and high sensitivity to rejection.
- Depressive Disorder Due to Another Medical Condition: Conditions like an underactive thyroid, Parkinson’s disease, or heart disease can trigger depressive symptoms.
- Seasonal Affective Disorder (SAD): Depression that follows a seasonal pattern, typically starting in the fall or winter.
Uncovering the Causes and Path to Diagnosis
The exact causes of depression are complex, but it’s usually a combination of biological, psychological, and environmental factors.
Key factors include:
- Neurotransmitters: Imbalances in brain chemicals like serotonin and dopamine are linked to mood regulation.
- Genetics: A family history of depression can increase your risk.
- Stressful Life Events: Trauma, loss, chronic stress, or major life changes can trigger depression.
- Medical Conditions: Health issues like hypothyroidism, heart disease, and cancer can cause or worsen symptoms.
A diagnosis is made by a mental health professional or doctor and typically includes:
- A Psychiatric Evaluation: A detailed discussion of your symptoms, thoughts, feelings, and behaviors.
- A Physical Exam: To rule out other medical problems causing your symptoms.
- Lab Tests: Blood tests, like a thyroid panel, can rule out physical health issues.
The official diagnosis requires five or more specific symptoms lasting at least two weeks, including a depressed mood or loss of interest. An accurate diagnosis is the first step to finding the best solution for depression for you.
The Pillars of Treatment: Finding the Best Solution for Depression
Once diagnosed, a wide range of effective treatments are available. Finding the best solution for depression often means combining approaches based on your unique needs and the severity of your condition. The main pillars of treatment include psychotherapy, medication, and, for some, advanced brain stimulation therapies.
For those with treatment-resistant depression, a personalized treatment plan is even more crucial for finding a sustainable path toward well-being.
Psychotherapy: Is Talk Therapy the Best Solution for Depression?
Psychotherapy, or “talk therapy,” is a cornerstone of depression treatment. It provides a safe space to explore thoughts and behaviors contributing to depression and develop healthier coping skills. For many with mild to moderate depression, psychotherapy can be a highly effective primary treatment.
Helpful types of talk therapy include:
- Cognitive Behavioral Therapy (CBT): Helps you identify and challenge negative thought patterns and behaviors, replacing them with more realistic ones. A key component, behavioral activation, encourages engaging in positive activities.
- Interpersonal Therapy (IPT): Focuses on current relationship problems, helping improve communication skills and resolve conflicts to strengthen social support.
- Behavioral Activation: A targeted therapy focused on increasing engagement in rewarding activities to combat the withdrawal and apathy common in depression.
These therapies are highly beneficial, as shown in studies like this meta-analysis of Cognitive-Behavioral Therapy for adult depression. For those with bipolar disorder, understanding Bipolar Disorder Psychotherapy is also key. Success often depends on consistency and a good connection with your therapist.
Here’s a quick comparison:
| Therapy Type | Primary Focus |
|---|---|
| Cognitive Behavioral Therapy (CBT) | Changing distorted thoughts and problematic behaviors. It involves recognizing and challenging negative thinking patterns and using behavioral activation to engage in positive activities. |
| Interpersonal Therapy (IPT) | Addressing current interpersonal problems and relationship issues that contribute to depression. It aims to improve communication skills and social support. |
| Behavioral Activation | Directly increasing engagement in positive, rewarding activities to counteract withdrawal and apathy. It emphasizes “doing” to change mood, rather than waiting for mood to change. |
Medication and Advanced Therapies: Finding the Best Solution for Depression for Severe Cases
For moderate to severe depression, medication is often a crucial part of treatment, especially when combined with psychotherapy. Antidepressants work by adjusting neurotransmitters in the brain to restore a healthier chemical balance.
Common types of antidepressants include:
- Selective Serotonin Reuptake Inhibitors (SSRIs): Often the first-line treatment. Medications like fluoxetine (Prozac) and sertraline (Zoloft) increase serotonin levels and typically have fewer side effects.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Drugs such as venlafaxine (Effexor) and duloxetine (Cymbalta) boost both serotonin and norepinephrine.
- Atypical Antidepressants: This group works in various ways and includes medications like bupropion (Wellbutrin) and mirtazapine (Remeron).
Antidepressants usually take 4 to 8 weeks to become fully effective. While generally safe, they can have side effects. Close monitoring by a healthcare provider is essential, especially for young adults under 25, due to a small risk of increased suicidal thoughts. You can find detailed Information on medications from the FDA.
For severe or treatment-resistant cases, advanced therapies can be life-changing:
- Electroconvulsive Therapy (ECT): Involves brief electrical stimulation of the brain under general anesthesia. It is highly effective for severe depression.
- Transcranial Magnetic Stimulation (TMS): A non-invasive procedure using magnetic fields to stimulate nerve cells in the brain involved in mood control.
- Esketamine: An FDA-approved nasal spray for treatment-resistant depression that can offer rapid relief under medical supervision.
Holistic Healing: Lifestyle Changes and Complementary Therapies
Beyond professional treatments, a holistic approach supports recovery by addressing the whole self—mind, body, and spirit. When combined with other treatments, these lifestyle changes and complementary therapies can be a key part of finding your best solution for depression, building a strong mind-body connection and offering natural relief.
The Power of Lifestyle Adjustments
Simple, consistent lifestyle changes can have a profound impact on managing depression symptoms and boosting brain health.
- Exercise: Aim for 30 minutes of moderate activity, like brisk walking, five times a week. Exercise releases endorphins, which act as natural mood boosters. Research consistently shows how much exercise helps with depression.
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can positively influence your mood. Limit processed foods, sugar, and unhealthy fats.
- Sleep Hygiene: Getting 7-9 hours of quality sleep is vital. A regular sleep schedule can ease many depression symptoms.
- Avoiding Alcohol and Drugs: These substances are depressants and can worsen symptoms in the long run, making recovery harder.
- Social Connection: Spending time with loved ones and nurturing relationships helps combat the isolation that often accompanies depression.
- Stress Management: Chronic stress worsens depression. Simple practices like deep breathing or short breaks can help manage stress levels.
Mindfulness and Meditation: Training Your Brain for Wellness
Mindfulness meditation is a powerful tool for managing depression. It involves focusing on the present moment and observing your thoughts and feelings without judgment.
This practice helps you pause worries, creating a space between you and your thoughts so you can react to them less. Learning non-judgmental awareness builds self-compassion, which is essential for healing. You can find helpful self-compassion exercises on Kristin D. Neff’s website here. Studies show that an eight-week meditation course can lead to a 10% to 20% improvement in depression symptoms. Group mindfulness is even recommended by health bodies like NICE for less severe depression.
Exploring Complementary Therapies
Certain complementary therapies can offer extra support alongside traditional treatments. Always talk with your healthcare provider before trying something new.
- Acupuncture: This traditional Chinese practice uses thin needles at specific body points and may help reduce depression symptoms for some.
- Yoga: Combining physical poses, breathing exercises, and meditation, yoga is a great way to reduce stress and improve mood.
- St. John’s Wort: An herbal supplement for mild depression, but it can have serious interactions with prescription drugs like antidepressants and birth control. Its effectiveness varies, so consult a doctor before use.
- Omega-3 Fatty Acids: Found in fish oil, these are important for brain health. However, a review found that Omega-3 fatty acids were not conclusively effective for depression in adults.
- Art and Music Therapy: Creative expression provides an outlet for emotions, reduces stress, and improves mood. Research on music therapy for depression shows it can be a helpful aid.
These therapies are best used to “complement” established medical and psychological treatments as part of a complete care plan.
Navigating the Journey: Support, Outlook, and Prevention
The path through depression can be winding, but recovery is a common outcome for most who seek help. With the right support and treatment, a brighter future is possible. Understanding the journey, preventing setbacks, and supporting loved ones are all crucial steps.
Knowing When to Reach Out for Professional Help
It’s normal to feel sad sometimes, but it’s important to know when to seek professional attention. Reach out if:
- Your symptoms are impacting your daily life, making it hard to work, enjoy relationships, or handle everyday tasks.
- You’ve experienced five or more depression symptoms nearly every day for two weeks or longer.
- You are having thoughts of self-harm, death, or suicide. This is an emergency. Call or text the 988 Suicide and Crisis Lifeline at 988, or call 911 if the situation is life-threatening. Your safety is the priority.
Seeking help is an act of courage. Early diagnosis and treatment improve the prognosis and reduce the long-term impact of depression.
How to Be a Supportive Ally to Someone with Depression
Watching a loved one struggle with depression is difficult, but your support can make a huge difference. Here’s how to help:
- Offer support and patience. Let them know you’re there for them without judgment. Understand that depression is an illness, not a choice.
- Encourage professional help. Offer to help them find a therapist or go with them to an appointment.
- Listen without judgment. Often, simply being heard is the best solution for depression you can offer in the moment. You don’t need to “fix” everything.
- Help with daily tasks. Practical support like helping with chores or errands can lighten their load significantly.
- Invite them to activities. They may decline, but continue to extend gentle invitations. A short walk could make a positive difference.
- Remind them that recovery is possible. Celebrate small victories and reassure them that with time and treatment, things can get better.
Outlook, Recovery, and Prevention Strategies
The outlook for depression is very positive, with 80% to 90% of people responding well to treatment. Recovery is a process, not always a straight line, and often involves ongoing management.
While depression can be a chronic condition for some, many achieve full remission. For others, long-term management with continued therapy or medication allows them to lead fulfilling lives.
A key part of wellness is practicing healthy coping mechanisms, such as stress management and emotional regulation, to build resilience and help prevent relapse.
Regular self-care is also essential. Prioritizing good sleep, nutrition, exercise, and mindfulness strengthens your defense against future depressive episodes.
Finally, building a strong support network of family, friends, and support groups provides a vital buffer against isolation and a reliable resource during challenging times. While we can’t always prevent depression, these strategies can significantly reduce the risk and are among the best solution for depression for achieving a good outcome.
Frequently Asked Questions about Depression Treatment
It’s natural to have questions when facing depression. At Addiction Helpline America, we want to provide clear answers to some of the most common questions to help you feel more informed and hopeful.
What is considered the most effective treatment for depression?
There is no single “most effective” treatment, as the best solution for depression is highly personal. For moderate to severe depression, a combination of psychotherapy (talk therapy) and antidepressant medication is often the most powerful approach. This duo tackles both the psychological and biological aspects of the condition. For milder cases, psychotherapy or lifestyle changes alone may be sufficient. A personalized plan crafted with a healthcare professional is key.
Can depression be cured completely?
While we often speak of remission rather than a “cure,” many people do experience a complete disappearance of their symptoms and live full, thriving lives. For some, depression can be a chronic or recurrent condition. In these cases, the goal is effective management—learning to spot early warning signs and using strategies to address them quickly. With the right tools and support, long-term wellness is a very realistic and achievable goal.
How long does it take to recover from depression?
The recovery timeline is unique to each person and depends on the severity of the depression, the treatments used, and individual response. If you start antidepressants, you may notice improvements in sleep or appetite within 4-8 weeks, with mood benefits taking longer. Psychotherapy can range from a few months to several years, depending on the issues being addressed. The process requires patience and persistence with your treatment plan. Every step forward is a victory on your path to well-being.
Conclusion: Your Path to a Brighter Tomorrow
Living with depression is a tough journey, but we hope this guide has illuminated the many paths to healing. There is no single best solution for depression; instead, recovery lies in finding the right combination of treatments and strategies custom to you.
We’ve covered key tools like psychotherapy, medication, and advanced therapies, as well as the transformative power of lifestyle adjustments and mindfulness. Each of these can be part of your personalized plan for recovery.
You don’t have to go through this alone. Recovery is a real possibility, and countless people have found their way to a more hopeful tomorrow. Reaching out is a brave first step. At Addiction Helpline America, we are passionate about connecting people nationwide with the right support and treatment programs. Let us be your guide as you find your unique path forward.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.