The Hidden Struggle of Benzodiazepine Withdrawal
Benzo withdrawal symptoms can be far more complex and distressing than most people realize. Stopping benzodiazepines like Xanax, Valium, Ativan, or Klonopin after regular use forces your body and brain to readjust, a process that can bring unexpected challenges.
Common benzo withdrawal symptoms include:
- Anxiety and panic attacks (often worse than before)
- Insomnia and sleep disturbances
- Tremors and muscle pain
- Sweating and heart palpitations
- Nausea and headaches
- Difficulty concentrating
- Mood swings and irritability
More severe symptoms can include:
- Seizures
- Hallucinations
- Psychosis
- Suicidal thoughts
Benzodiazepines are prescribed medications meant to calm the nervous system. They’re often given for anxiety, panic disorders, insomnia, or seizures. Common brand names include Xanax (alprazolam), Valium (diazepam), Klonopin (clonazepam), and Ativan (lorazepam).
While helpful for short-term use, taking benzos for longer than a few weeks can lead to physical dependence. As your brain adapts to the drug, stopping suddenly or reducing the dose too quickly can trigger withdrawal symptoms ranging from uncomfortable to life-threatening.
Here’s what many people don’t know: Some withdrawal symptoms are rarely discussed, even by healthcare providers. Beyond the common experiences of anxiety and insomnia, there are lesser-known symptoms that can be confusing, frightening, and isolating. You might feel sensations that seem impossible to explain or experience symptoms that make you question your sanity.
This guide covers seven benzo withdrawal symptoms you won’t often hear about. We’ll explain what’s happening in your body and how you can safely steer the path to recovery.
You do not have to face this alone. Recovery is possible, and professional support can make a meaningful difference. If you’re struggling with benzodiazepine dependence or withdrawal, Addiction Helpline America offers free, confidential guidance to help you explore treatment options custom to your needs.
Understanding Why Benzo Withdrawal Happens
Benzodiazepines, often called “benzos,” are a class of psychoactive drugs that act as central nervous system (CNS) depressants. They are prescribed to treat a variety of conditions, including anxiety, panic disorders, insomnia, muscle spasms, and seizure disorders. Common examples include alprazolam (Xanax), diazepam (Valium), lorazepam (Ativan), and clonazepam (Klonopin). The DEA classifies them as Schedule IV controlled substances, indicating their potential for abuse and dependence.
Neurologically, benzodiazepines improve the effects of gamma-aminobutyric acid (GABA), the brain’s primary inhibitory neurotransmitter, or “brake.” This action calms the nervous system, reducing anxiety, inducing sleep, and relaxing muscles.
With prolonged use (more than a few weeks), the brain adapts to the drug’s constant presence. This leads to tolerance and physical dependence.
Tolerance means that your body needs increasingly higher doses of the drug to achieve the same therapeutic effect. The brain’s GABA receptors become less sensitive to the drug, or their numbers may even decrease.
Dependence occurs when your body physically adapts to the drug’s presence and requires it to function “normally.” When the drug is suddenly reduced or stopped, your brain, which has become accustomed to the improved inhibitory effects of GABA, goes into overdrive. This sudden imbalance—a rebound of excitatory activity—is what triggers benzo withdrawal symptoms.
Physical dependence is a physiological response, not a moral failing, and can develop even when taking benzos as prescribed. The risk of dependence and severe withdrawal increases with higher doses and longer duration of use. For instance, patients taking 4 mg/day or higher of Xanax for longer than three months were more likely to become dependent and experience more uncomfortable withdrawal symptoms than those taking smaller doses for less time.
Common vs. Severe Benzo Withdrawal Symptoms
When facing benzo withdrawal symptoms, it’s helpful to understand the spectrum of experiences. Many people will encounter common physical and psychological symptoms, often referred to as “rebound symptoms” because they represent the return, and often intensification, of the original conditions the benzodiazepine was prescribed for, such as anxiety or insomnia. These rebound effects are distinct from withdrawal symptoms caused by the body adapting to use, but they can overlap.
The importance of medical supervision during withdrawal cannot be overstated. Abrupt cessation of benzodiazepines, often called “cold turkey,” is not only incredibly difficult but can also be extremely dangerous, potentially leading to life-threatening complications. According to recommendations from the Substance Abuse and Mental Health Services Administration (SAMHSA), benzo withdrawal—particularly for those with severe symptoms—should not be attempted without medical supervision.
We dig deeper into The importance of medical supervision for benzo withdrawal in another guide.
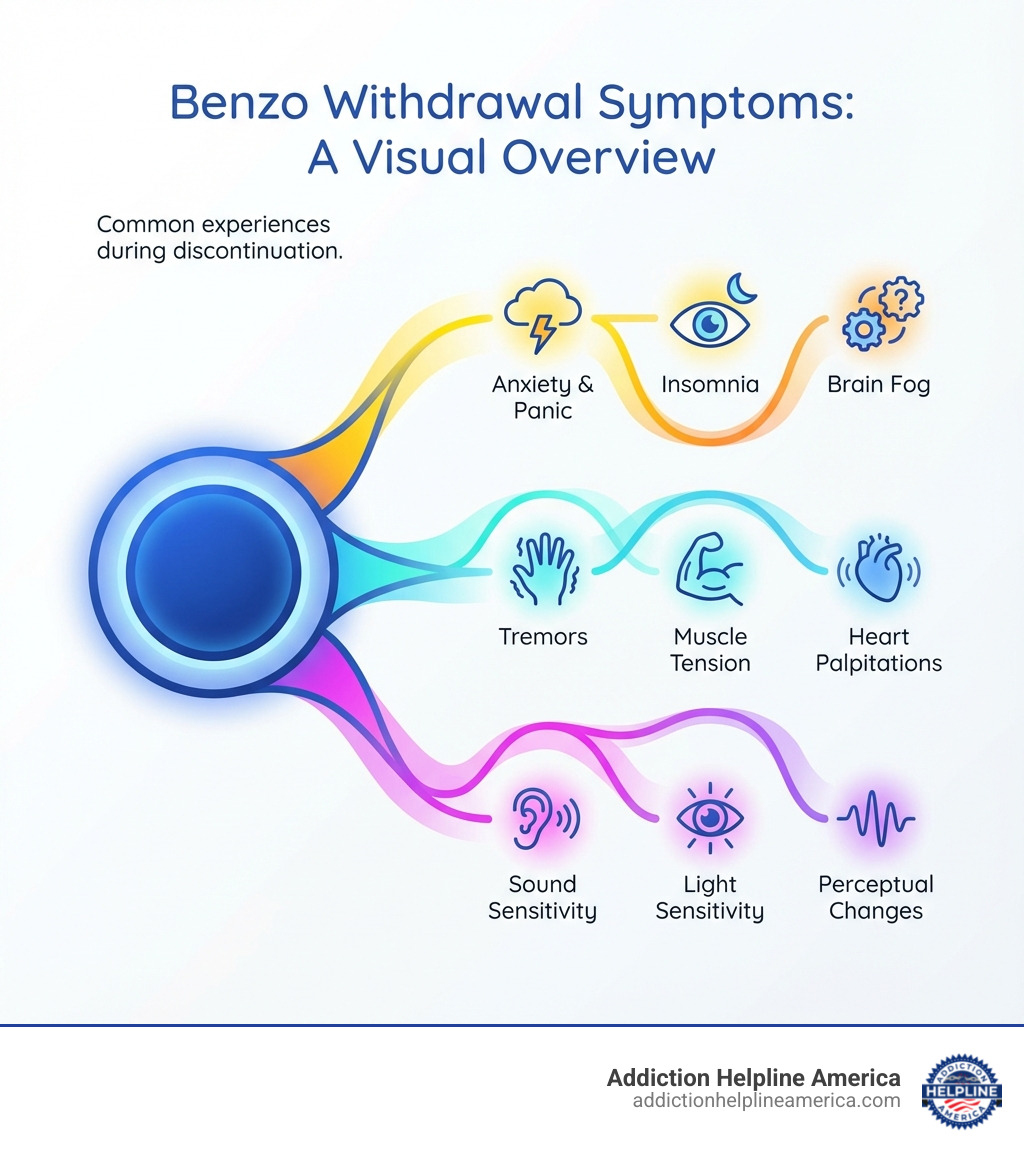
Common Physical and Psychological Symptoms
Common benzo withdrawal symptoms are uncomfortable but usually not life-threatening. They often feel like a more intense version of the issues the benzo was prescribed for:
- Insomnia: Sleep disturbances are very common, often more severe than before medication, and can include vivid nightmares.
- Rebound anxiety: A significant increase in anxiety, panic attacks, and feelings of dread.
- Irritability: Heightened emotional sensitivity, mood swings, and agitation.
- Sweating: Profuse sweating, even in cool environments.
- Headaches: Persistent and sometimes severe headaches.
- Muscle pain and stiffness: Aches, spasms, and a feeling of tension throughout the body.
- Nausea: Accompanied by dry wretching, vomiting, or loss of appetite, sometimes leading to weight loss.
- Poor concentration: Difficulty focusing, clouded thinking, and short-term memory impairment.
- Hand tremor: Involuntary shaking, especially of the hands.
- Heart palpitations: A racing heart or irregular heartbeat.
- Perceptual changes: Mild alterations in sensory perception, such as blurry vision.
These symptoms can be distressing and make daily functioning challenging, highlighting why a gradual, medically supervised taper is the safest approach.
The Dangers of Severe Withdrawal
Severe, life-threatening benzo withdrawal symptoms can occur, especially with abrupt cessation or a rapid taper. These serious complications require immediate medical attention:
- Grand mal seizures: This is one of the most dangerous risks of unsupervised benzo withdrawal, particularly with short-acting benzodiazepines or high doses. Seizures can lead to injury, brain damage, or even death.
- Psychosis: This can include hallucinations (seeing or hearing things that aren’t there), delusions (false beliefs), and severe paranoia.
- Hallucinations: Visual, auditory, or tactile hallucinations can occur, making it difficult to distinguish reality.
- Delirium tremens (DTs): Although more commonly associated with severe alcohol withdrawal, DTs can occur during benzo withdrawal, presenting with severe confusion, disorientation, rapid heart rate, high blood pressure, fever, and agitation.
- Catatonia: A state of unresponsiveness, immobility, and sometimes unusual postures.
- Suicidal ideation: The intense psychological distress, anxiety, and depression during withdrawal can increase the risk of suicidal thoughts or behaviors. The U.S. Food and Drug Administration (FDA) includes a warning about this risk for users of Ativan with pre-existing depression.
- Myocardial ischemia: In rare cases, severe withdrawal can lead to heart problems.
These severe benzo withdrawal symptoms underscore why medical detox is not just recommended but often critical. If you or a loved one are experiencing any of these severe symptoms, please seek immediate medical help.
For life-threatening emergencies, call 911 immediately.
7 Lesser-Known Benzo Withdrawal Symptoms
While the common benzo withdrawal symptoms like anxiety and insomnia are widely recognized, there’s a host of other experiences that can catch individuals off guard. These lesser-known symptoms can be profoundly unsettling and often go unmentioned in general discussions about withdrawal. Understanding them can help validate your experience and prepare you for a smoother recovery journey.
Withdrawal is more than just anxiety; it’s a profound systemic recalibration. Here are seven benzo withdrawal symptoms that might surprise you:
1. Protracted Withdrawal Syndrome (PAWS)
One of the most frustrating aspects of benzo withdrawal is protracted withdrawal syndrome (PAWS), where symptoms persist for months or even years after stopping the drug. While not an official diagnosis, PAWS is widely recognized in the recovery community.
Studies suggest that an estimated 10 to 25% of long-term benzo users experience protracted withdrawal, with some feeling symptoms years after they have stopped.
The symptoms of PAWS often fluctuate, described as “waves and windows,” where intense symptom periods (“waves”) are interspersed with periods of relative calm (“windows”). Lingering PAWS symptoms can include persistent anxiety, insomnia, cognitive issues, and depression. This prolonged state can severely impact daily life, making sustained support crucial. For more information on More info on long-term recovery after withdrawal, we have dedicated resources.
2. Depersonalization and Derealization
These are profound and often terrifying psychological symptoms that can occur during benzo withdrawal. They involve a distorted sense of reality or self:
- Depersonalization: Feeling detached from your own body, thoughts, or emotions, as if you are an outside observer of your own life. You might feel like a robot or that your body isn’t real.
- Derealization: Feeling that the world around you isn’t real, or that people and objects are distant, foggy, or dream-like. Familiar places might seem strange or unfamiliar.
These experiences can be incredibly disorienting and can make individuals question their sanity, often leading to increased anxiety and panic. These are known withdrawal phenomena. To learn more about mental health symptoms during withdrawal, our resources can provide further insight.
3. Heightened Sensory Perception
As the brain’s inhibitory system (GABA) recalibrates, the nervous system can become overstimulated, leading to sensory hypersensitivity. This can manifest as:
- Hypersensitivity to light (photophobia): Ordinary light can feel painfully bright.
- Hypersensitivity to sound (hyperacusis): Normal sounds can seem excessively loud or jarring.
- Metallic taste: A persistent, unpleasant metallic taste in the mouth.
- Altered sense of smell: Odors can become unusually strong or distorted.
- Tingling or numbness (paresthesia): Sensations like “pins and needles” or numbness in the extremities, or even burning sensations on the skin.
These symptoms can make everyday environments feel hostile and contribute significantly to distress.
4. Formication
Formication is a type of tactile hallucination where you experience the sensation of insects crawling on or under your skin, even though nothing is physically there. This can be an incredibly distressing and disturbing symptom, often leading to intense itching, scratching, and increased anxiety. While it can occur with other types of withdrawal, it is a recognized, albeit less common, benzo withdrawal symptom.
5. Persistent Tinnitus
Tinnitus is the perception of ringing, buzzing, hissing, clicking, or roaring sounds in one or both ears, even when there is no external sound source. While many people experience temporary tinnitus, during benzo withdrawal, it can become persistent and highly bothersome. This symptom can be temporary, resolving as the brain heals, or it can become protracted, lasting for months or even years, significantly impacting quality of life and sleep.
6. New or Worsening OCD-like Symptoms
Some individuals undergoing benzo withdrawal may experience the emergence or exacerbation of obsessive-compulsive disorder (OCD)-like symptoms. This can include:
- Development of obsessive thoughts: Intrusive, unwanted thoughts or images that are difficult to control.
- Emergence of compulsive behaviors: Repetitive behaviors or mental acts performed in response to an obsession, often to reduce anxiety.
These symptoms can be particularly confusing if there was no prior history of OCD, leading to concerns about developing a new mental health condition. This is another sign of the brain’s dysregulation during withdrawal.
7. Severe Gastrointestinal Distress
Withdrawal can also trigger severe, often overlooked gastrointestinal issues beyond simple nausea:
- Abdominal cramps mimicking surgical conditions: Intense, sharp abdominal pains that can be mistaken for more serious medical issues.
- Diarrhea or constipation: Significant changes in bowel habits.
- Loss of appetite: Leading to further weight loss and nutritional deficiencies.
These symptoms contribute to physical discomfort and can complicate the withdrawal process, sometimes requiring medical intervention to manage.
The Withdrawal Timeline and Influencing Factors
Understanding the timeline of benzo withdrawal symptoms is crucial for managing expectations and planning a safe recovery. It’s not a one-size-fits-all experience, as various factors can significantly influence how long symptoms last and their intensity.
| Type of Benzodiazepine | Onset of Symptoms | Peak of Symptoms | Duration of Acute Withdrawal | Severity Considerations |
|---|---|---|---|---|
| Short-Acting | 6-24 hours after last dose | Day 2-4 | 1-2 weeks | More rapid onset, often more intense, higher risk of seizures. |
| Long-Acting | 1-7 days after last dose | Week 2-3 | 2-8 weeks (or longer) | Slower onset, generally less intense acute phase, but can be prolonged. |
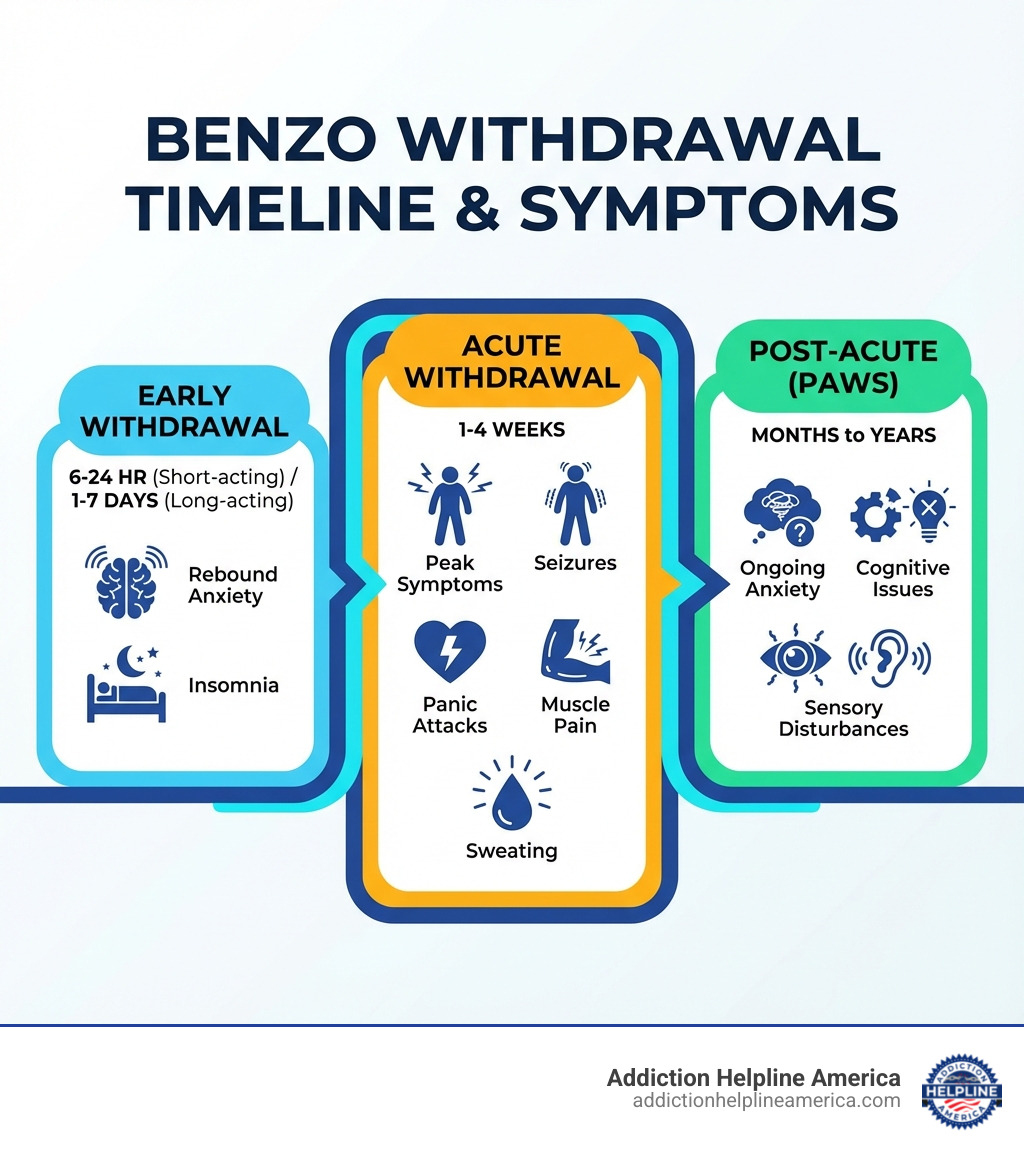
A Typical Timeline for Benzo Withdrawal Symptoms
Benzo withdrawal typically involves several phases:
- Acute phase: This phase generally begins once the drug leaves your system and can last from one to four weeks. During this time, you’ll experience the most intense physical and psychological symptoms. For short-acting benzos like Xanax or Ativan, symptoms can begin within 6-24 hours. For long-acting benzos like Valium or Klonopin, symptoms might not appear for 1-7 days. The peak intensity of symptoms typically occurs around day 2-4 for short-acting benzos and week 2-3 for long-acting ones.
- Post-acute phase (PAWS): After the acute phase, some individuals enter PAWS, where symptoms can persist for months or years, often coming and going in “waves.”
Recovery from benzo withdrawal is rarely a straight line. There will be good days and bad days, and patience with yourself and the process is key.
How the Type of Benzo Affects Withdrawal
The drug’s half-life—the time it takes for half of it to leave your body—plays a significant role in your withdrawal experience.
- Short-acting benzodiazepines (e.g., Xanax, Ativan): These drugs have a shorter half-life, meaning they leave your system quickly. This leads to a more rapid onset of benzo withdrawal symptoms (within hours) and often a more intense, but shorter, acute withdrawal period. The risk of severe symptoms like seizures can be higher with abrupt discontinuation of short-acting benzos.
- Long-acting benzodiazepines (e.g., Valium, Klonopin): These drugs have a longer half-life, leading to a slower elimination from the body. Consequently, benzo withdrawal symptoms may not begin for several days or even up to three weeks after your last dose. The acute withdrawal phase tends to be less intense but can last for a longer duration. This longer half-life is why long-acting benzos like diazepam are often used in tapering schedules to provide a smoother, more controlled withdrawal.
Factors That Influence Your Experience with Benzo Withdrawal Symptoms
While the type of benzo is a major factor, several other elements can influence the severity and duration of your benzo withdrawal symptoms:
- Dosage and duration of use: The higher the dose and the longer you’ve been taking benzodiazepines, the more significant the physical dependence and the more severe and prolonged your withdrawal symptoms are likely to be. For example, individuals taking 4 mg/day or higher of Xanax for longer than three months were more likely to become dependent and experience more uncomfortable withdrawal symptoms.
- Individual physiology and genetics: Each person’s body metabolizes drugs differently, and genetic factors can influence how severe withdrawal symptoms are.
- Co-occurring mental health conditions: If you have underlying anxiety, depression, or other mental health disorders, these conditions can be exacerbated during withdrawal, making the experience more challenging. Specialized treatment for dual diagnoses is often beneficial.
- Polysubstance use: Using benzodiazepines alongside other substances, especially other CNS depressants like alcohol or opioids, significantly increases the risks and complicates withdrawal. A 2014 report from the Drug Abuse Warning Network (DAWN) found that mixing benzodiazepines with alcohol or opioids increases the risk of a serious medical outcome by 24 to 55 percent.
- Method of discontinuation (taper vs. cold turkey): Abruptly stopping benzodiazepines is the most dangerous approach and significantly increases the risk of severe and life-threatening symptoms. A gradual, medically supervised tapering schedule is crucial for minimizing the intensity and duration of benzo withdrawal symptoms.
How to Safely Manage Withdrawal and Begin Recovery
Facing benzo withdrawal symptoms is overwhelming, but recovery is achievable with the right support. You don’t have to go through this alone. However, quitting without medical supervision is dangerous and can lead to severe complications.
Addiction Helpline America connects people across the United States with medical detox programs, inpatient rehab, and outpatient services for benzodiazepine dependence. Our guidance is free, confidential, and focused on helping you find care that fits your situation.
The Gold Standard: Medically Supervised Detox and Tapering
The safest and most effective way to manage benzo withdrawal symptoms is through medically supervised detox and a gradual tapering schedule. Quitting “cold turkey” can be life-threatening due to the risk of seizures and other severe complications.
- Why tapering is essential: Tapering involves slowly reducing your benzodiazepine dose over time, allowing your brain and body to gradually adjust. This minimizes the shock to your system and significantly reduces the severity of withdrawal symptoms. The American Society of Addiction Medicine (ASAM) recommends a gradual taper, often over 8-12 weeks or longer, to ensure safety.
- Working with a medical professional: A doctor, ideally one specializing in addiction medicine or psychiatry, will create an individualized tapering plan custom to your specific needs, the type of benzo you’re on, your dosage, and your overall health. This plan might involve switching to a longer-acting benzodiazepine like diazepam, which has a smoother withdrawal profile, and then slowly reducing that dose.
- Medical oversight: During medical detox, healthcare professionals monitor your vital signs, manage symptoms, and adjust your taper schedule as needed to ensure your safety and comfort. This can take place in an inpatient or outpatient setting, depending on your situation. We can help you Find a medical detox program near you through our extensive network.
Medications That Can Help
While tapering is the primary method, certain adjunct medications can help manage specific benzo withdrawal symptoms and make the process more tolerable:
- Anticonvulsants: Medications like gabapentin or carbamazepine may be prescribed to help prevent seizures, especially in severe withdrawal cases.
- Beta-blockers: These can help alleviate physical symptoms of anxiety, such as a rapid heart rate and tremors.
- Antidepressants: For individuals experiencing significant depression during or after withdrawal, certain antidepressants may be considered. However, some research suggests that SSRI antidepressants may not be effective for treating depression that occurs after benzo withdrawal.
- Flumazenil: This medication is a benzodiazepine receptor antagonist. While it can precipitate acute withdrawal if given too quickly, studies suggest it might have a role in treating protracted withdrawal symptoms. Its use requires very careful medical supervision.
These medications are supportive, not a cure for dependence. Always consult a USA-based healthcare provider, as some medications (like bupropion, certain antipsychotics, and fluoroquinolone antibiotics) are contraindicated and can be dangerous during benzo withdrawal.
Inpatient vs. Outpatient Treatment Settings
The choice between inpatient and outpatient treatment depends on the severity of your dependence, your overall health, and your support system.
- Inpatient care: This is typically recommended for individuals with severe benzodiazepine dependence, a history of complicated withdrawals, co-occurring mental health disorders, or a lack of stable home environment. Inpatient facilities provide 24/7 medical supervision, structured therapy, and a safe, drug-free environment. Patients using more than 50mg diazepam equivalent per day are often managed in an inpatient setting. Learn more about inpatient treatment options.
- Outpatient care: This option is suitable for individuals with milder dependence, good physical health, and a strong support system at home. Outpatient medically managed detox allows you to continue living at home while attending regular medical appointments and therapy sessions. This approach is often used for patients taking less than 50mg diazepam equivalent per day.
Both settings emphasize a gradual taper, medical monitoring, and comprehensive support.
The Critical Role of Psychological and Holistic Support
Beyond medical management, psychological and holistic support are vital components of successful benzo withdrawal and long-term recovery. These interventions address the underlying reasons for substance use and equip you with coping mechanisms.
- Cognitive-Behavioral Therapy (CBT): CBT is highly effective for changing negative thought patterns and behaviors related to anxiety and substance use. It teaches vital coping skills for managing post-withdrawal symptoms and preventing relapse.
- Support groups: Groups such as benzodiazepine-focused peer meetings and other USA-based recovery communities provide a safe space to share experiences, gain peer support, and reduce feelings of isolation. The reassurance from family, friends, and peers significantly improves outcomes.
- Stress management techniques: Practices such as mindfulness meditation, deep breathing exercises, and yoga can help calm the nervous system and manage anxiety without medication.
- Nutrition and exercise: A healthy diet supports brain healing, and regular physical activity can improve mood, reduce anxiety, and promote better sleep.
- Counseling and therapy: Individual and family therapy can address trauma, relationship issues, and other psychological factors contributing to dependence. Psychosocial interventions have been shown to be effective for benzodiazepine dependence. We provide resources for Psychosocial interventions for benzodiazepine dependence to help you find the right support.
If you are in the United States and considering tapering off benzodiazepines, reaching out for professional help can be the safest first step. Addiction Helpline America is available to offer free, confidential information about treatment options and support resources near you.
Frequently Asked Questions about Benzo Withdrawal
Can you die from benzodiazepine withdrawal?
Yes, benzo withdrawal symptoms can be fatal due to complications like seizures, suicidal behavior, or catatonia. Abrupt cessation, especially from high doses or short-acting benzodiazepines, can trigger severe neurological and cardiac events that are life-threatening. This is why medically supervised detoxification is crucial, and you should never attempt to quit “cold turkey” on your own. Professional medical care ensures that severe symptoms are managed promptly and safely.
How long do the worst benzo withdrawal symptoms last?
The most intense, or “acute,” benzo withdrawal symptoms typically peak within the first two weeks (often day 2-4 for short-acting benzos, and week 2-3 for long-acting ones) and begin to subside after that. However, some individuals may experience Post-Acute Withdrawal Syndrome (PAWS), where less intense but still disruptive symptoms can linger for months or even years. The average duration of acute withdrawal is around two months, but this can vary significantly based on individual factors.
What is the first step to safely stop taking benzodiazepines?
The most important first step is to speak with a qualified medical professional, such as your prescribing doctor or an addiction specialist. They can help you create a safe tapering plan that is gradual and custom to your specific needs. For immediate guidance and to find a specialist, you can call a confidential helpline. Addiction Helpline America is here to help you take that first step. Call us at 844-561-0606 for free and confidential assistance.
Conclusion: There Is Hope and a Path Forward
The journey through benzo withdrawal symptoms is challenging, marked by unexpected physical and psychological discomforts. Understanding the full range of symptoms—from common anxiety to lesser-known issues like depersonalization or sensory hypersensitivity—is the first step toward healing.
This guide has highlighted the complexities of benzo withdrawal and reinforced a critical message: you do not have to endure it alone. Recovery is achievable. The key is seeking professional help for a medically supervised, gradual taper, complemented by psychological and holistic support.
At Addiction Helpline America, we are dedicated to connecting individuals across the United States with the resources and compassionate care needed for a safe and sustainable recovery. Our service is free, confidential, and focused on helping you explore treatment programs that align with your needs.
Your journey to a healthier life can start with a single, informed step. When you are ready, reaching out for support can open the door to effective treatment, ongoing recovery resources, and a future that is not defined by benzodiazepines.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.