Understanding the Challenge of Benzodiazepine Withdrawal
Benzo withdrawal help is a critical need for millions of people who’ve become physically dependent on these commonly prescribed medications. Whether you’ve been taking Xanax for anxiety, Valium for sleep, or Ativan for panic attacks, stopping these drugs can trigger a complex withdrawal syndrome that requires careful management and professional support.
Essential Benzo Withdrawal Help Options:
- Medical Supervision – Never quit “cold turkey” – seizures and life-threatening complications can occur
- Gradual Tapering – Slowly reduce dosage over weeks or months under doctor guidance
- Substitution Method – Switch to longer-acting benzos like Valium for smoother tapering
- Symptom Management – Medications and therapies to ease withdrawal discomfort
- Support Groups – Peer support from others going through similar experiences
- Professional Treatment – Inpatient or outpatient programs with addiction specialists
Benzodiazepines work by enhancing GABA, your brain’s main calming neurotransmitter. Over time, your brain reduces its natural GABA production and becomes dependent on the medication. When you stop taking benzos, this creates a dangerous imbalance that can last weeks to months – or even years in some cases.
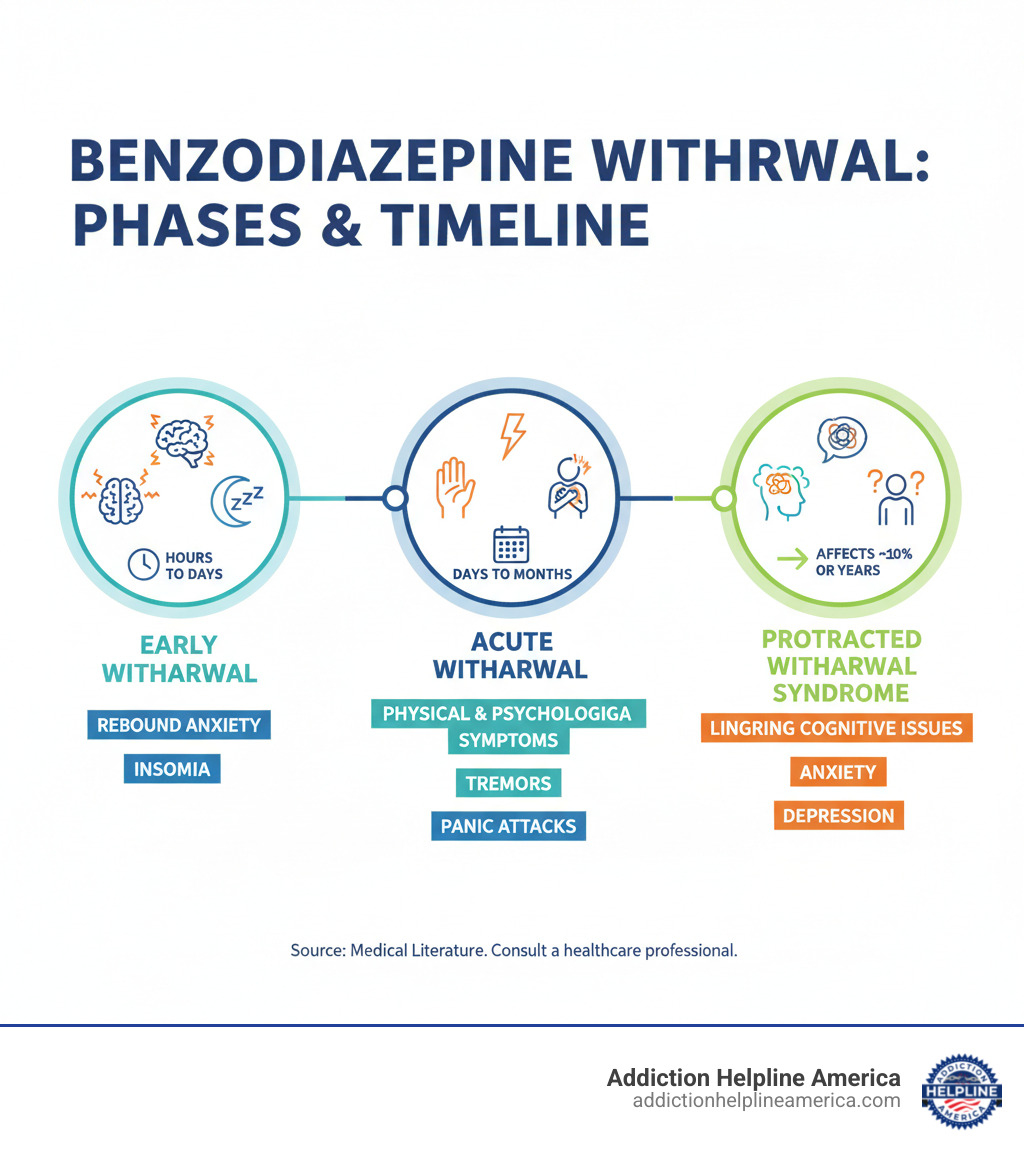
The withdrawal process typically unfolds in three phases: early withdrawal (hours to days), acute withdrawal (days to months), and for about 10% of users, protracted withdrawal syndrome that can extend much longer. Symptoms range from anxiety and insomnia to potentially life-threatening seizures.
At Addiction Helpline America, we’ve helped thousands of individuals and families steer the complex journey of benzodiazepine withdrawal through our 24/7 helpline and treatment referral services. Our experienced team understands that finding the right benzo withdrawal help can mean the difference between a safe, successful recovery and dangerous complications.
Understanding Benzo Withdrawal: Symptoms, Phases, and Timeline
If you’ve been taking benzodiazepines like Xanax, Valium, or Klonopin, understanding what happens when you stop is the first step toward getting the benzo withdrawal help you need.
Benzodiazepines boost GABA, your brain’s natural calming chemical. Over time, your brain adapts by producing less of its own GABA, becoming dependent on the medication to function normally. When you stop, your nervous system goes into overdrive, causing a withdrawal syndrome as it tries to rebalance.
Withdrawal severity is influenced by the duration of use, dosage, the type of benzo, and any co-occurring disorders like depression or other substance use issues.
Common Withdrawal Symptoms
Benzo withdrawal affects both mind and body. These symptoms are a natural response as your brain heals, not a sign of weakness.
Psychological symptoms often include a temporary “rebound” effect, where the original issues return with greater intensity. Common symptoms are:
- Intense anxiety and panic attacks
- Insomnia and sleep disturbances
- Irritability and mood swings
- Depression and feelings of hopelessness
- Derealization (feeling disconnected from reality)
- Memory problems and difficulty concentrating
Physical symptoms can be equally challenging and may include:
- Severe headaches and profuse sweating
- Muscle pain, stiffness, and tremors
- Nausea and digestive issues
- Heart palpitations or a racing heart
- Sensory changes like light sensitivity (photophobia) or ringing in the ears (tinnitus)
The most serious physical risk is seizures, which can be life-threatening. This is why professional medical supervision is critical.
The Withdrawal Timeline and Phases
Everyone’s timeline is unique, but it generally follows a pattern based on the type of benzodiazepine used.
| Characteristic | Short-Acting Benzos (Xanax, Ativan) | Long-Acting Benzos (Valium, Klonopin) |
|---|---|---|
| Onset of Symptoms | 10-12 hours | 2-10 days (up to 3 weeks) |
| Peak of Symptoms | 2-3 days | 1-2 weeks |
| Duration of Acute Phase | Weeks to a few months | Weeks to several months |
Early withdrawal begins with rebound symptoms like anxiety and insomnia as the medication leaves your system.
Acute withdrawal is the most challenging phase, lasting from days to months. During this time, you’ll experience the full range of physical and psychological symptoms as your brain works to restore its natural balance.
What is Protracted Withdrawal Syndrome (PAWS)?
About 10% of users experience PAWS, where some symptoms persist for months or even years after the acute phase. This is also known as post-acute withdrawal.
PAWS symptoms often appear in waves (periods of intense symptoms) and windows (periods of relief). Common symptoms include muscle twitches, prolonged anxiety, and cognitive issues. While this sounds daunting, it is manageable with the right support. The brain is rewiring itself, and this healing process takes time. With patience and proper management strategies, people with PAWS do recover.
At Addiction Helpline America, we understand that benzo withdrawal help is a long-term journey. We connect you with resources for every phase of your recovery.
Safe Tapering and Professional Benzo Withdrawal Help
The single most important rule of stopping benzodiazepines is: never quit cold turkey. Abruptly stopping can cause life-threatening seizures, psychosis, and other medical emergencies. Your brain needs time to readjust after becoming dependent on the medication.
Safe benzo withdrawal help is centered on a gradual taper—slowly reducing your dose over time under medical supervision. This is like walking down a staircase instead of jumping off a cliff. Your tapering schedule must be individualized to your specific needs, stress levels, and support system.
Recommended Tapering Methods
A doctor can help you choose the best method based on your medication, duration of use, and individual response.
- Direct Tapering: Gradually reducing your current medication, typically by 5-25% every one to four weeks. Slower is often gentler.
- Substitution Tapering: Switching to a long-acting benzo like Valium (diazepam) before tapering. This is especially helpful for short-acting drugs like Xanax, as it provides more stable blood levels and reduces inter-dose withdrawal.
- Titration Tapering: Dissolving medication in liquid to make very small, precise dose reductions. This is useful in the final stages of a taper when sensitivity to cuts is high.
Resources like The Ashton Manual and VA tapering guidelines provide structured approaches. A taper can last from eight weeks to over a year; the goal is safety, not speed.
Medical Interventions for Benzo Withdrawal Help
Medical detox provides the safest environment for withdrawal. While no medication can eliminate all symptoms, some can help manage specific issues:
- Anticonvulsants (e.g., gabapentin) may be used to reduce seizure risk, especially when coming off high doses.
- Antidepressants (e.g., SSRIs) can help manage severe depression but must be introduced carefully.
- Beta-blockers (e.g., propranolol) can relieve physical anxiety symptoms like a racing heart, tremors, and sweating.
- Other medications like trazodone for sleep or clonidine for physical symptoms may also be used.
Any additional medication should be part of a comprehensive plan managed by your healthcare provider.
Non-Medical Support and Coping Strategies
Successful withdrawal combines medical tapering with strong emotional and practical support.
- Cognitive Behavioral Therapy (CBT): Helps you change negative thought patterns and learn practical coping skills to manage anxiety without medication.
- Support Groups: Peer support from online communities or local groups provides understanding and hope from people with shared experiences.
- Stress Management: Techniques like deep breathing, mindfulness, and gentle yoga can help calm an overactive nervous system.
- Lifestyle Choices: Avoiding caffeine and alcohol is essential, as they can worsen anxiety and disrupt sleep. Gentle exercise like walking can reduce symptoms, but listen to your body and avoid intense workouts that may backfire.
- Nutrition and Hydration: A balanced diet supports brain healing, and staying hydrated is important.
- Education: Understanding the withdrawal process makes it less frightening and empowers you to manage your recovery.
Addiction Helpline America can connect you with providers and programs that offer this comprehensive support.
Navigating Risks and Special Considerations
An honest conversation about benzodiazepine withdrawal must include the serious risks involved. Benzo withdrawal help is not just a recommendation—it is essential for your safety. As Psychology Today notes, withdrawal from substances like alcohol, benzos, and opiates “might kill you”. This is why professional medical supervision is non-negotiable.
The most severe risks of abrupt withdrawal include:
- Seizures: Can occur without warning, especially after long-term or high-dose use.
- Psychosis: Hallucinations, delusions, and severe confusion.
- Delirium Tremens-like symptoms: Dangerous shifts in heart rate, blood pressure, and body temperature.
- Suicidal Thoughts: Intense emotional pain during withdrawal can feel overwhelming.
A healthcare provider who understands benzodiazepine withdrawal can create a safe tapering plan that minimizes these dangers.
When to Seek Professional Benzo Withdrawal Help
While professional help is always advised, it is absolutely critical in these high-risk situations:
- History of seizures
- High-dose or long-term use
- Use of other substances, especially alcohol
- Severe mental health conditions like bipolar disorder or psychosis
- Lack of a stable or supportive home environment
- Previous failed attempts to taper
- Inability to function or thoughts of self-harm
In these cases, an inpatient medical detox facility provides the safest environment. For less severe cases, intensive outpatient care may be sufficient.
Special Considerations for Certain Populations
Withdrawal affects different people in different ways, requiring customized care.
Seniors face unique challenges due to slower metabolism, an increased risk of falls from confusion or poor coordination, and potential interactions with other medications. Their tapers must be extremely gradual and carefully monitored.
People with co-occurring disorders (e.g., benzodiazepine dependence plus depression or PTSD) require integrated dual diagnosis treatment that addresses both conditions simultaneously. Treating one while ignoring the other is rarely effective. Addiction Helpline America specializes in connecting people to these programs. More information about co-occurring disorders treatment is available through our services.
Pregnant individuals also face unique risks, as withdrawal affects both mother and baby. This requires close collaboration with medical experts to ensure the safety of both.
These considerations underscore why a personalized, professional approach to benzo withdrawal help is so important.
Frequently Asked Questions about Benzo Withdrawal
When you’re facing benzo withdrawal, it’s natural to have questions. Here are honest answers to the ones we hear most often.
How long does benzo withdrawal last?
The timeline varies for everyone. The acute phase, or the most intense period, typically lasts from a few weeks to several months. The duration depends on factors like how long you used benzos, your dosage, the type of benzo, and the speed of your taper.
For those with long-term dependencies, the entire recovery process, including the taper and post-taper healing, can take six to eighteen months. About 10% of people experience Protracted Withdrawal Syndrome (PAWS), where some symptoms linger for longer, but they do improve over time. Full recovery is always the goal and is absolutely possible.
Can you die from benzodiazepine withdrawal?
Yes, benzodiazepine withdrawal can be life-threatening if not managed properly. This is why you should never quit “cold turkey” or without medical supervision.
The most serious risks are grand mal seizures, a condition similar to delirium tremens (severe confusion, agitation, and dangerous vital sign changes), and an increased risk of suicide due to intense psychological distress.
A gradual taper supervised by a healthcare professional dramatically reduces these risks, making the process safe.
Will the anxiety I took benzos for come back?
This is a complex but important question. In early withdrawal, you will likely experience rebound anxiety, which is a temporary withdrawal symptom that can feel more intense than your original anxiety. It’s your brain reacting to the absence of the drug.
Once withdrawal subsides, your original anxiety may or may not return. However, the withdrawal process is an opportunity to learn new, healthier ways to manage anxiety. Cognitive Behavioral Therapy (CBT) is a highly effective, non-pharmacological treatment that provides better long-term results than medication for many people.
By developing new coping skills, you can build a more resilient and sustainable approach to your mental health, moving forward without depending on medication.
Conclusion
The path through benzodiazepine withdrawal can feel overwhelming, but here’s what we want you to remember: recovery is absolutely possible. Thousands of people have successfully freed themselves from benzodiazepine dependence, and with the right support and approach, you can too.
Throughout this guide, we’ve walked through the complex reality of how benzos rewire your brain’s chemistry, creating the physical dependence that makes stopping so difficult. We’ve explored the wide range of symptoms you might face – from the challenging but temporary acute withdrawal phase to the less common but very real protracted withdrawal syndrome that affects about one in ten people.
Most importantly, we’ve emphasized that this journey requires patience, professional guidance, and a personalized plan. The dangers of trying to quit cold turkey are simply too great. Your brain needs time to heal and readjust, which is why medically supervised tapering – whether through a direct taper or switching to a longer-acting medication like Valium – is so crucial for your safety.
The benzo withdrawal help you need comes in many forms. Medical supervision protects you from life-threatening complications like seizures. Therapeutic support through approaches like Cognitive Behavioral Therapy gives you new tools to manage anxiety without medication. Support groups connect you with others who truly understand what you’re experiencing. Even simple lifestyle changes – like avoiding caffeine, getting gentle exercise, and practicing stress management techniques – can make a meaningful difference in your recovery.
Healing isn’t always linear. You might experience those frustrating “waves” of symptoms followed by hopeful “windows” of relief. This doesn’t mean you’re not making progress – it’s a normal part of how your brain heals from long-term benzodiazepine use.
At Addiction Helpline America, we’ve helped countless individuals and families steer this exact journey. We understand that finding the right treatment approach can feel confusing and overwhelming when you’re already struggling with withdrawal symptoms. That’s why our experienced team is here to provide free, confidential guidance to connect you with the specific resources and treatment centers that match your unique situation.
Your journey toward a benzo-free life doesn’t have to wait. Whether you’re just starting to consider tapering, currently working through withdrawal symptoms, or dealing with lingering effects months later, professional help is available right now.
Take the first step towards a benzo-free life. Find confidential benzo withdrawal help today through our nationwide network of treatment professionals who specialize in benzodiazepine withdrawal and recovery.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.