What Is Addiction? Understanding This Common but Misunderstood Condition
According to the American Society of Addiction Medicine (ASAM), the definition of addiction is a “treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment, and an individual’s life experiences.” People with addiction use substances or engage in behaviors that become compulsive and often continue despite harmful consequences.
Key characteristics of addiction include:
- Compulsive behavior – Unable to stop using substances or engaging in behaviors despite wanting to quit
- Loss of control – Using more than intended or for longer periods than planned
- Continued use despite harm – Persisting even when facing serious negative consequences
- Craving – Intense urges or need for the substance or behavior
- Brain changes – Altered brain function in areas related to reward, stress, and self-control
Addiction affects a staggering number of people. According to the 2022 National Survey on Drug Use and Health (NSDUH), approximately 48.7 million Americans aged 12 or older had a substance use disorder in the past year. Yet, it remains one of the most misunderstood health conditions. Many people still view addiction as a moral failing, but leading health organizations like the National Institute on Drug Abuse (NIDA) recognize it as a chronic brain disease—similar to diabetes or heart disease—that can be effectively treated with proper care and support.
At Addiction Helpline America, we connect individuals and families nationwide to vital resources, treatment options, and confidential support for understanding the definition of addiction and navigating the path to recovery. Our free helpline is available 24/7 to provide immediate assistance and guidance.
Understanding the Core Definition of Addiction
The journey to understanding addiction often begins with clarifying its fundamental nature. For many years, the term “addiction” was used loosely, sometimes even colloquially, to describe any behavior that felt out of control. We might hear someone say they’re “addicted to coffee” or “addicted to a TV show.” While these phrases highlight a strong inclination, they often miss the profound medical and psychological complexities that define true addiction.
The medical community, particularly organizations like the American Society of Addiction Medicine (ASAM), has worked tirelessly to refine the definition of addiction to promote a consistent, scientific understanding. ASAM provides a detailed clinical definition, stating that addiction is a “primary, chronic disease of brain reward, motivation, memory and related circuitry.” This means that addiction isn’t merely a symptom of other problems; it’s a disease in its own right, impacting the very core of how our brains function.
This medical consensus emphasizes that addiction involves complex interactions among a person’s brain circuits, genetic makeup, environmental influences, and life experiences. It’s a treatable, chronic medical disease, much like other chronic conditions such as asthma or heart disease. The critical element is that individuals with addiction continue to use substances or engage in behaviors compulsively, despite experiencing harmful consequences. This isn’t a desired state; it’s a condition where control has been severely compromised.
The ‘4 Cs’ of Addiction
To help us better grasp the multifaceted nature of addiction, many experts use a framework known as the “4 Cs.” These characteristics serve as key indicators that a behavior or substance use has crossed the line from casual or problematic use into addiction.
Let’s break down each of these essential components:
- Compulsion: An irresistible urge to use a substance or engage in a behavior, even when one wants to stop. This compulsive drive can override rational thought.
- Craving: An intense psychological or physical desire for the substance or activity. Cravings can be triggered by internal feelings (like stress) or external cues (like places or people).
- Consequences: Continuing the behavior despite significant negative consequences in one’s health, relationships, finances, or legal standing.
- Control (Loss of): The inability to stop or limit the substance use or behavior, even with a genuine desire to do so.
These “4 Cs” help us understand that addiction is far more than just a bad habit; it’s a complex condition characterized by a profound loss of self-control and persistent engagement despite clear harm.
Addiction vs. Dependence vs. Withdrawal
It’s common to confuse addiction with other related terms like “dependence” and “withdrawal,” but understanding the distinctions is crucial for accurate diagnosis and effective treatment. While these concepts are interconnected, they are not interchangeable. These distinctions are detailed by health authorities like the National Institute on Drug Abuse (NIDA) and the Substance Abuse and Mental Health Services Administration (SAMHSA).
| Feature | Addiction | Physical Dependence | Withdrawal – | A chronic brain disease characterized by compulsive substance use or behavior despite harmful consequences. It involves impaired control, craving, and a dysfunctional emotional response. | A physiological state where the body adapts to a substance. Stopping or reducing use causes withdrawal symptoms. It can occur with or without addiction. | The physical and psychological symptoms that occur when a substance is stopped or reduced. It is a sign of physical dependence. |
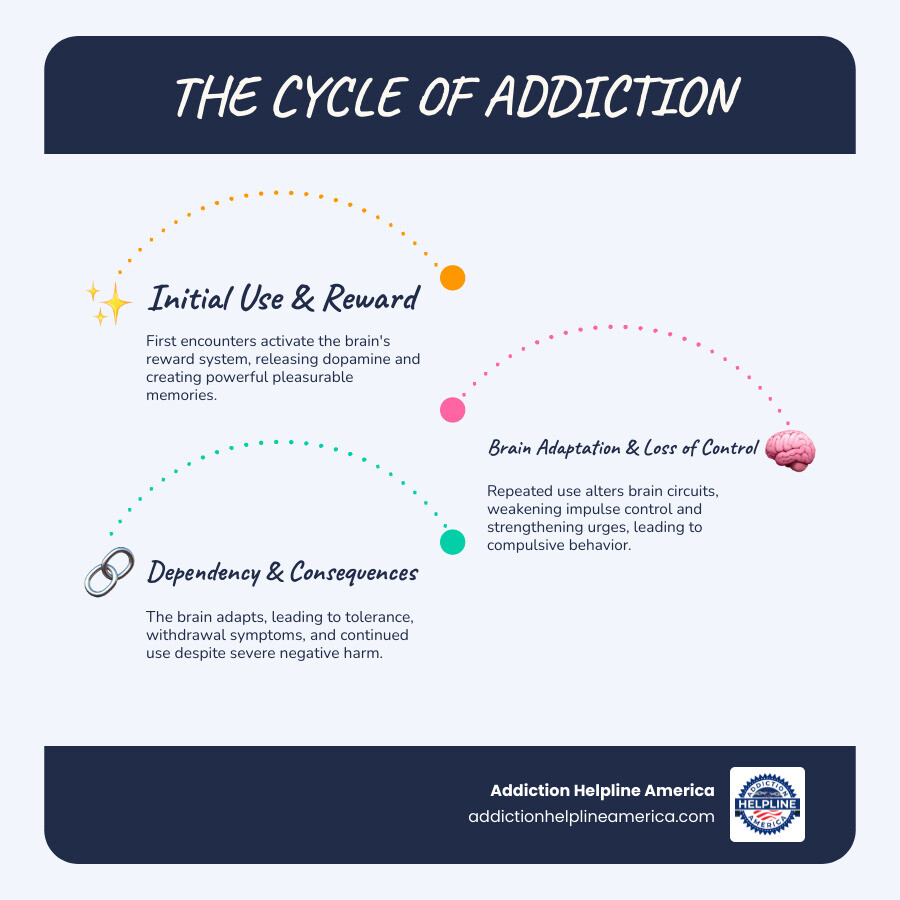
The Science of Addiction: How It Changes the Brain
To truly understand the definition of addiction, we must look beyond its behavioral manifestations and dig into the intricate workings of the brain. Modern science has dramatically reshaped our understanding, moving away from moral judgments to a clear recognition of addiction as a disease rooted in fundamental brain changes.
Our brains have a reward system that releases dopamine, a neurotransmitter associated with pleasure and motivation, when we engage in enjoyable activities. Addictive substances and behaviors hijack this system by causing an unnatural surge of dopamine, creating a powerful drive to repeat the behavior. This repeated exposure leads to long-lasting brain changes (neuroplasticity), especially in circuits for reward, motivation, memory, and self-control. The brain adapts, reducing its response to natural pleasures and requiring the substance just to feel “normal” or avoid withdrawal. The National Institute on Drug Abuse (NIDA) provides comprehensive insights into these brain changes, affirming that addiction is a brain disorder. For a deeper dive into the science, you can explore The science of addiction from NIDA.
Is Addiction a Brain Disease?
This is a question that often sparks debate, but from a medical standpoint, the answer is a resounding “yes.” Addiction is indeed considered a brain disease. The American Society of Addiction Medicine (ASAM) explicitly defines it as such, and major health organizations worldwide concur. This perspective is vital because it shifts the understanding of addiction from a moral failing to a recognized medical condition.
The brain disease model of addiction posits that chronic exposure to addictive substances or behaviors causes fundamental changes in brain structure and function. Specifically, areas of the brain responsible for executive functions—such as judgment, decision-making, and impulse control—become impaired. This is particularly evident in the prefrontal cortex. When this part of the brain is compromised, our capacity for self-control is severely diminished, making it incredibly difficult to resist the urge to use, even when we desperately want to stop.
While the initial decision to try a substance might be voluntary, the development of addiction fundamentally alters the brain’s capacity for self-control. As NIDA explains, this impairment in self-control is the hallmark of addiction. It’s not that individuals with addiction choose to keep using despite consequences; it’s that their brains have been rewired to compel continued use. Genetic factors account for 40% to 60% of a person’s risk, but they interact with environmental factors and life experiences. For more on the neurobiology behind this model, you can read Neurobiology of the brain disease model.
Signs, Symptoms, and the Clinical Definition of Addiction
Recognizing the signs and symptoms of addiction is crucial for early intervention and support. These indicators often manifest across various aspects of a person’s life, affecting their behavior, physical health, and emotional well-being.
According to the Mayo Clinic, common behavioral and physical symptoms we often observe include:
- Inability to stop: Despite repeated attempts or a strong desire to quit, the person cannot stop using the substance or engaging in the behavior.
- Increased tolerance: Needing larger amounts of the substance or more frequent engagement in the activity to achieve the desired effect.
- Withdrawal symptoms: Experiencing physical or psychological discomfort (e.g., anxiety, irritability, tremors, nausea) when reducing or stopping use.
- Intense focus/Preoccupation: Spending an excessive amount of time thinking about, obtaining, using, or recovering from the substance or behavior.
- Neglecting responsibilities: Failing to meet obligations at work, school, or home due to substance use or addictive behavior.
- Giving up activities: Abandoning hobbies, social events, or other important activities that were once enjoyed.
- Continued use despite problems: Persisting with the behavior even when it causes significant physical harm, relationship issues, financial difficulties, or legal troubles.
- Risky use: Engaging in the behavior in dangerous situations, such as driving under the influence.
- Changes in mood or behavior: Increased irritability, anxiety, depression, secrecy, or sudden shifts in personality.
- Changes in physical appearance: Neglect of hygiene, unexplained weight changes, or noticeable physical effects of substance use.
Clinically, the definition of addiction is formally captured in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published by the American Psychiatric Association, which uses the term “Substance Use Disorder” (SUD). An SUD diagnosis is based on 11 criteria across four categories: impaired control, social impairment, risky use, and pharmacological effects (tolerance and withdrawal).
To be diagnosed with an SUD, an individual must meet at least two of these 11 criteria within a 12-month period. The severity of the disorder is then classified based on the number of criteria met:
- Mild SUD: 2-3 criteria
- Moderate SUD: 4-5 criteria
- Severe SUD: 6 or more criteria
One of the critical insights from the research is the strong link between addiction and other mental health conditions. According to the National Institute on Drug Abuse (NIDA), approximately half of the people who experience a mental health condition will also experience a substance use disorder, and vice versa. This phenomenon, known as comorbidity or dual diagnosis, means that mental health issues can increase the risk of addiction, and addiction can, in turn, trigger or worsen mental health problems. Addressing both conditions concurrently is often essential for effective treatment and lasting recovery.
Causes, Risk Factors, and Types of Addiction
Addiction is not a one-size-fits-all condition, nor does it stem from a single cause. Instead, it arises from a complex interplay of various factors unique to each individual. We recognize that understanding this multi-layered origin is fundamental to a comprehensive definition of addiction.
This intricate dance between different influences is often described through the biopsychosocial model, which highlights how biological, psychological, and social factors all contribute to a person’s vulnerability to addiction. While some individuals may have a higher predisposition, others might develop addiction due to overwhelming environmental pressures or underlying psychological struggles. It’s this unique combination that shapes each person’s journey.
Key Risk Factors for Developing an Addiction
While no single factor guarantees addiction, several elements can significantly increase our risk:
- Genetic Predisposition: Genetics account for 40-60% of a person’s addiction risk, according to the National Institute on Drug Abuse (NIDA). A family history of substance use significantly increases vulnerability.
- Environmental Factors: Our surroundings and experiences profoundly shape our vulnerability.
- Family and Peer Influence: A home environment with substance use or lack of supervision, along with peer pressure, increases risk.
- Early Use: Starting drug use at a young age increases the likelihood of addiction, as the adolescent brain is particularly vulnerable.
- Trauma (Adverse Childhood Experiences – ACEs): Stressful or traumatic events during childhood, such as abuse or neglect, are strongly linked to a higher risk of addiction later in life, a connection well-documented by the Centers for Disease Control and Prevention (CDC).
- Drug Availability and Method of Use: Easy access to drugs and methods of use that deliver them to the brain quickly (e.g., injecting, smoking) increase addiction potential.
- Psychological Factors: Our mental health and personality traits also play a part.
- Co-occurring Mental Health Disorders: Conditions like depression, anxiety, or PTSD are significant risk factors, as individuals may use substances to self-medicate. As noted by NIDA, about half of those with a mental illness also experience a substance use disorder.
- Personality Traits: Impulsivity and sensation-seeking can increase the likelihood of substance use and addiction.
Understanding these risk factors is not about assigning blame but about identifying areas where prevention and early intervention can be most effective. The Mayo Clinic provides further insights into these Risk factors for drug addiction.
Substance vs. Behavioral: The Two Main Types of Addiction
When we talk about the definition of addiction, it’s important to recognize that it encompasses more than just drugs and alcohol. Addiction broadly falls into two main categories: substance addictions and behavioral addictions.
-
Substance Addictions (Substance Use Disorders – SUDs): This category includes addictions to psychoactive substances that directly alter brain chemistry. Examples include:
- Alcohol: The most common substance use disorder in the U.S.
- Opioids: Including prescription painkillers (like oxycodone) and illicit opioids (like heroin and fentanyl), often treated with methadone.
- Stimulants: Such as cocaine, methamphetamine, and prescription stimulants (like Adderall).
- Cannabis: Marijuana use can lead to a diagnosable SUD.
- Nicotine: Found in tobacco products and e-cigarettes.
- Sedatives, Hypnotics, or Anxiolytics: Including benzodiazepines (like Xanax, Valium).
- Hallucinogens and Inhalants.
-
Behavioral Addictions (Non-Substance Addictions): These involve compulsive engagement in certain activities that provide a similar “reward” or “high,” leading to significant negative consequences.
- Gambling Disorder: The only behavioral addiction currently recognized in the DSM-5.
- Gaming Disorder: Recognized by the World Health Organization (WHO), this involves compulsive video gaming that impairs daily life.
- Internet Addiction: Compulsive internet use, including social media, that negatively impacts real-life obligations and relationships.
- Shopping Addiction: Compulsive buying that leads to financial and interpersonal problems.
- Sex Addiction/Hypersexual Disorder: Compulsive sexual thoughts and acts that are difficult to control and cause significant distress.
- Food Addiction: An uncontrollable craving for certain foods, often leading to patterns of compulsive eating.
The expansion of the definition of addiction to include problematic behaviors reflects a deeper understanding of the underlying brain mechanisms involved in compulsive reward-seeking, whether the reward comes from a chemical substance or an activity.
Pathways to Recovery: Treatment, Support, and Hope
Understanding the definition of addiction is just the first step; the next, and most crucial, is recognizing that recovery is not only possible but achievable for everyone. Addiction, as a chronic disease, requires ongoing management, much like diabetes or hypertension. There is no “one-size-fits-all” approach, and successful treatment is often a dynamic process that adapts to individual needs over time.
We at Addiction Helpline America believe firmly in the power of hope and the effectiveness of evidence-based care. Our mission is to connect individuals across the nation, including those in California, Texas, Florida, New York, Pennsylvania, Illinois, Ohio, Georgia, North Carolina, Michigan, Arizona, Massachusetts, Washington, and many other states, to the right treatment centers and support systems, guiding them toward lasting recovery.
Evidence-Based Treatment Approaches
Effective addiction treatment is comprehensive and follows evidence-based principles, such as those outlined in NIDA’s Principles of Drug Addiction Treatment. It addresses the whole person, not just their substance use, and integrates various strategies custom to the individual’s specific situation, severity of addiction, and any co-occurring conditions.
Here are some of the evidence-based approaches we help connect people to:
- Medical Detoxification (Detox): Often the first step, medical detox safely manages withdrawal symptoms under supervision. It stabilizes the individual but is not a complete treatment.
- Inpatient and Outpatient Care:
- Inpatient/Residential Treatment: Offers 24/7 structured care in a therapeutic setting, ideal for severe SUDs or those needing intensive support. Options range from 30-day programs to long-term care. Learn more about inpatient rehab.
- Outpatient Treatment: Provides flexibility, allowing individuals to live at home while attending scheduled therapy. It includes various levels of care, such as Intensive Outpatient Programs (IOPs), and is suitable for those with strong support systems. Learn more about Outpatient Drinking Rehab and compare Inpatient vs. Outpatient Rehab.
- Behavioral Therapies: Counseling and psychotherapy are cornerstones of addiction treatment. They help individuals identify triggers, develop coping mechanisms, and address underlying psychological issues. Common therapies include:
- Cognitive Behavioral Therapy (CBT): Helps individuals recognize and change problematic thoughts and behaviors.
- Dialectical Behavior Therapy (DBT): Focuses on emotional regulation, distress tolerance, and interpersonal effectiveness.
- Motivational Interviewing (MI): Helps individuals explore and resolve ambivalence about change.
- Family Behavior Therapy (FBT): Involves family members to improve communication and address dynamics contributing to addiction. For more on various therapeutic approaches, see Types of Addiction Therapy.
- Medication-Assisted Treatment (MAT): For many substance addictions, particularly opioid and alcohol use disorders, medications can be a highly effective component of treatment, as supported by the Substance Abuse and Mental Health Services Administration (SAMHSA). MAT combines FDA-approved medications with counseling and behavioral therapies. For example, methadone is used for opioid use disorder, and naltrexone or disulfiram for alcohol use disorder.
- Dual Diagnosis Treatment: Given the high comorbidity between addiction and other mental health conditions, integrated treatment that addresses both simultaneously is crucial. This can be found at specialized centers that offer comprehensive care for conditions like anxiety or bipolar disorder.
Our network includes treatment centers in your local area, from San Jose, California to New Orleans, Louisiana, and many more locations across the U.S., ready to provide personalized care.
The Role of Support Systems and Community Resources
Recovery is rarely a solitary journey. Strong support systems and community resources are invaluable, providing encouragement, accountability, and a sense of belonging.
- Peer Support Groups: Groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) offer free, anonymous meetings where individuals share experiences and support each other.
- Family Involvement: Engaging family members in therapy and support groups (like Al-Anon or Nar-Anon) can heal relationships and create a more supportive home environment. See Family Involvement in Rehab for more information.
- Community Support: Local community centers, faith-based organizations, and mental health services often provide resources to help individuals rebuild their lives.
- Anonymous Helplines: Services like the Samaritans or various national and local helplines offer immediate, confidential support. Addiction Helpline America is a free and confidential service, connecting individuals nationwide to addiction and mental health treatment centers, providing personalized guidance to find the right recovery program from our vast network. You can reach out to us at any time.
Outlook and Prevention
The outlook for individuals with addiction is increasingly positive with effective treatment. While addiction is a chronic disease, it is highly treatable, and many people achieve long-term recovery. Relapse can be part of the recovery process. As NIDA explains, it is not a sign of failure, but an indication that the treatment plan may need adjustment.
Prevention strategies, such as those promoted by SAMHSA, are crucial, particularly for young people. These strategies focus on:
- Reducing Risks: Managing stress with healthy coping mechanisms, avoiding early substance use, and being aware of family history.
- Building Protective Factors: Fostering strong family bonds, parental monitoring, positive peer relationships, and community involvement.
- Education: Raising awareness about the risks of substance use and the definition of addiction can empower individuals to make informed choices.
By focusing on these areas, we can build resilience and reduce the likelihood of addiction developing in our communities.
Frequently Asked Questions about the Definition of Addiction
We understand that the definition of addiction can be complex and raise many questions. Here, we address some of the most common inquiries we receive.
Can you be addicted to something that isn’t a drug?
Absolutely. While substance addictions are widely recognized, behavioral addictions are increasingly understood. Gambling disorder is officially recognized in the DSM-5, and others like gaming, internet, shopping, and sex addiction share many characteristics with substance addictions, including loss of control and negative consequences. If you or someone you know is struggling with a behavioral addiction, such as sex addiction, we can help connect you with appropriate resources, including specialized programs like a Sex Addiction Treatment Center California Guide.
Is addiction a choice or a disease?
This is perhaps one of the most frequently asked and misunderstood questions. The medical and scientific consensus is clear: addiction is a disease, not a moral failing. As the American Society of Addiction Medicine (ASAM) states, addiction is a chronic brain disease. While the initial decision to use a substance might be voluntary, addiction fundamentally alters the brain’s structure and function. These changes impair the brain’s ability to exert self-control, making it incredibly difficult to stop without professional help. Dr. Nora Volkow, Director of the National Institute on Drug Abuse (NIDA), puts it plainly: “It is not a choice to have the disease of addiction.” Individuals with addiction are not choosing to suffer; they are battling a chronic brain disease that has hijacked their reward and motivation systems.
What is the first step to getting help for addiction?
The first step, and often the hardest, is recognizing that a problem exists and being willing to seek help. This doesn’t necessarily mean being “ready” to stop completely, but rather acknowledging that substance use or a behavior is causing problems in your life. Once this realization occurs, the next crucial step is to seek a professional assessment from a healthcare provider, such as a doctor, psychiatrist, psychologist, or a certified drug and alcohol counselor. This advice is echoed by government health agencies like SAMHSA, which runs a National Helpline to connect people with local assistance and treatment referrals.
If you or a loved one is contemplating this step, you don’t have to steer it alone. Addiction Helpline America offers free, confidential, and personalized guidance to help you understand your options and connect with treatment centers nationwide. You can call us any time to start this vital conversation.
Conclusion: Finding a Path Forward
The definition of addiction has evolved significantly over time, moving from simplistic moral judgments to a nuanced understanding of a complex, chronic medical disease. We now know that addiction is a condition rooted in brain changes, influenced by genetics, environment, and life experiences, and characterized by compulsive behavior despite harmful consequences.
This understanding brings with it immense hope. Because addiction is a treatable disease, recovery is not just a possibility—it’s a reality for millions of Americans. It requires comprehensive, individualized treatment, ongoing support, and a commitment to a lifelong journey of healing and growth.
At Addiction Helpline America, we are dedicated to helping individuals and families find their path forward. We believe in reducing the stigma associated with addiction by promoting education and understanding. Our free and confidential services connect you with a vast network of addiction and mental health treatment centers across the country, providing the personalized guidance you need to take that crucial first step towards recovery.
Don’t let misunderstanding or fear stand in the way of a healthier, happier life. Reach out to us today to Find personalized addiction treatment options. Your journey to recovery starts here.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.