Introduction: Understanding Two Powerful Sedatives
Barbiturates vs benzo — both are powerful sedatives that act as central nervous system (CNS) depressants, but they differ significantly in their safety profiles, mechanisms, and modern medical use. Here’s what you need to know:
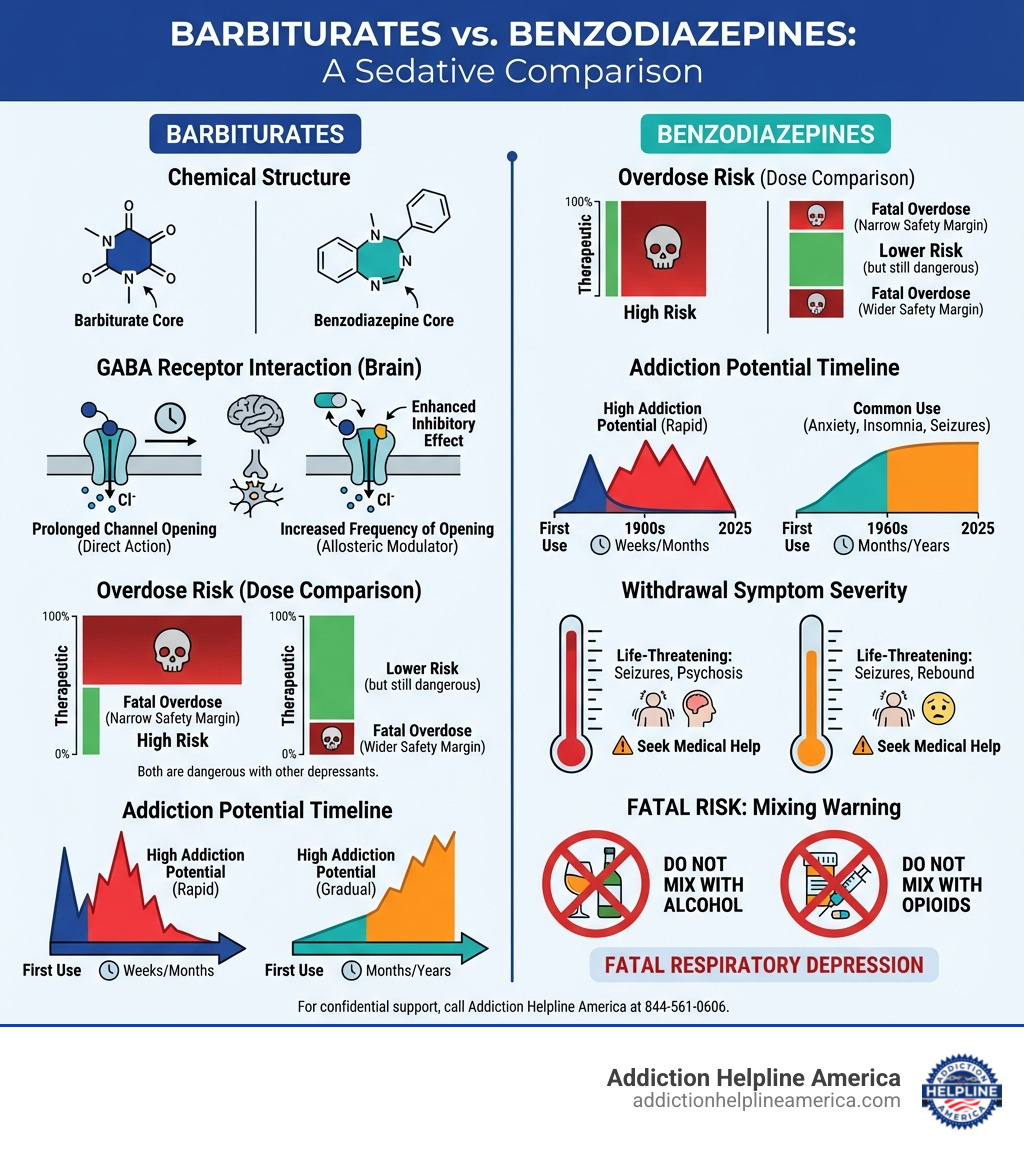
| Factor | Barbiturates | Benzodiazepines |
|---|---|---|
| Era Introduced | Early 1900s | 1960s |
| Overdose Risk | Very High (narrow therapeutic window) | Lower (wider safety margin) |
| Addiction Potential | Extremely High | High |
| Current Medical Use | Rare (anesthesia, severe seizures) | Common (anxiety, insomnia, seizures) |
| Mechanism | Prolong GABA channel opening | Increase frequency of GABA channel opening |
| Withdrawal Risk | Life-threatening (seizures, psychosis) | Life-threatening (seizures, rebound anxiety) |
Both drug classes were developed to treat conditions like anxiety, insomnia, and seizures. Barbiturates were once the most popular sedative worldwide, introduced in the early 1900s. However, their narrow margin between a therapeutic dose and a fatal overdose led to widespread deaths. By the 1960s, benzodiazepines emerged as a safer alternative and largely replaced barbiturates in medical practice.
Despite being “safer,” benzodiazepines are still dangerous. They carry a high risk of dependence, addiction, and life-threatening withdrawal. Mixing either drug class with alcohol or opioids can be fatal. Understanding the critical differences between these two classes of sedatives can help you or a loved one make informed decisions about treatment and recognize the warning signs of addiction.
If you or a loved one are struggling with sedative use, call Addiction Helpline America at 844-561-0606 for confidential support.
At Addiction Helpline America, we’ve spent years helping individuals and families steer the complex challenges of sedative addiction, including understanding the critical differences between barbiturates vs benzo and guiding people toward safe, evidence-based treatment. Our 24/7 helpline connects you with compassionate addiction specialists who can provide immediate assistance, treatment referrals, and ongoing support throughout your recovery journey.
Common barbiturates vs benzo vocab:
What Are Barbiturates and Benzodiazepines?
When we talk about central nervous system (CNS) depressants, we’re referring to a class of drugs that slow down brain activity. This can lead to a calming effect, reduced anxiety, muscle relaxation, and even sleep. Both barbiturates and benzodiazepines fall into this category, but their stories and roles in medicine have evolved quite differently.
The First Wave: A Look at Barbiturates
Barbiturates are a category of sedative-hypnotic medications that were first introduced in the early 20th century. Imagine the medical world before these drugs – limited options for anxiety, insomnia, or even preparing someone for surgery. Barbiturates stepped in to fill that void, quickly becoming widely recognized for their ability to treat a range of conditions.
Historically, barbiturates were commonly prescribed for issues like anxiety, headaches, insomnia, and seizure disorders. Their calming and relaxing effects were comparable to those induced by alcohol, making them potent tools for managing these conditions. They work by diminishing nerve activity, leading to muscle relaxation, a slowed heart rate, and reduced breathing.
The mechanism behind their power lies in their interaction with gamma-aminobutyric acid (GABA), the brain’s primary inhibitory neurotransmitter. Barbiturates act directly on GABA receptors, causing them to remain open for an extended period. This results in a more significant depressive effect on the central nervous system, effectively “slowing down” the brain.
Today, their use is much more restricted due to their high potential for abuse, addiction, and fatal overdose. However, they still have niche applications. For instance, some barbiturates are still used as effective anesthetics for surgery, and certain types, like phenobarbital, remain important for long-term seizure control, especially in cases where other medications are not effective. They are also sometimes used in veterinary medicine for anesthesia and euthanasia.
Here are some common barbiturates you might encounter, though their prescription is now rare:
- Phenobarbital
- Pentobarbital (Nembutal)
- Secobarbital (Seconal)
- Butalbital (often found in combination medications like Fioricet for migraines)
The Modern Alternative: An Introduction to Benzodiazepines
Fast forward to the 1960s, and a new class of drugs emerged: benzodiazepines. These were developed as a safer alternative to barbiturates for treating conditions such as anxiety, insomnia, and seizures. Benzodiazepines, often called “benzos,” quickly became widely prescribed sedatives and central nervous system depressants.
Like barbiturates, benzodiazepines also work by enhancing the effects of GABA. However, their approach is slightly different, making them generally safer (though still carrying significant risks, which we’ll discuss). This mechanism results in a calming effect, reducing stress and anxiety by inhibiting brain activity.
Benzodiazepines are highly versatile and are prescribed for a variety of conditions, including:
- Anxiety disorders: Generalized anxiety disorder, panic disorder, social anxiety disorder.
- Insomnia: Short-term treatment for sleep difficulties.
- Seizure disorders: Used to control acute seizures and some chronic epilepsy.
- Alcohol withdrawal: Managing the severe and potentially life-threatening symptoms of alcohol withdrawal.
- Muscle spasms: Relaxing tense muscles.
- Pre-operative sedation: To calm patients before medical procedures.
Some of the most well-known and widely prescribed benzodiazepines in the U.S. include:
- Diazepam (Valium)
- Alprazolam (Xanax)
- Lorazepam (Ativan)
- Clonazepam (Klonopin)
- Temazepam (Restoril)
These medications are staples in modern medicine, but their widespread use doesn’t negate their potential for dependence and addiction. We often find ourselves helping individuals in states like Alabama, California, Florida, Illinois, New York, and Texas who have become dependent on these powerful medications, even when taking them as prescribed.
If you are concerned about your use of benzodiazepines or other sedatives, help is available. Call Addiction Helpline America at 844-561-0606 for a confidential conversation about your options.
The Critical Differences: Barbiturates vs Benzo Showdown
While both barbiturates vs benzo are CNS depressants that interact with the GABA system, understanding their precise differences is crucial. It’s like comparing two different types of locks and keys – they both interact with the same door, but the way they do it impacts how easily that door can be opened (or jammed).
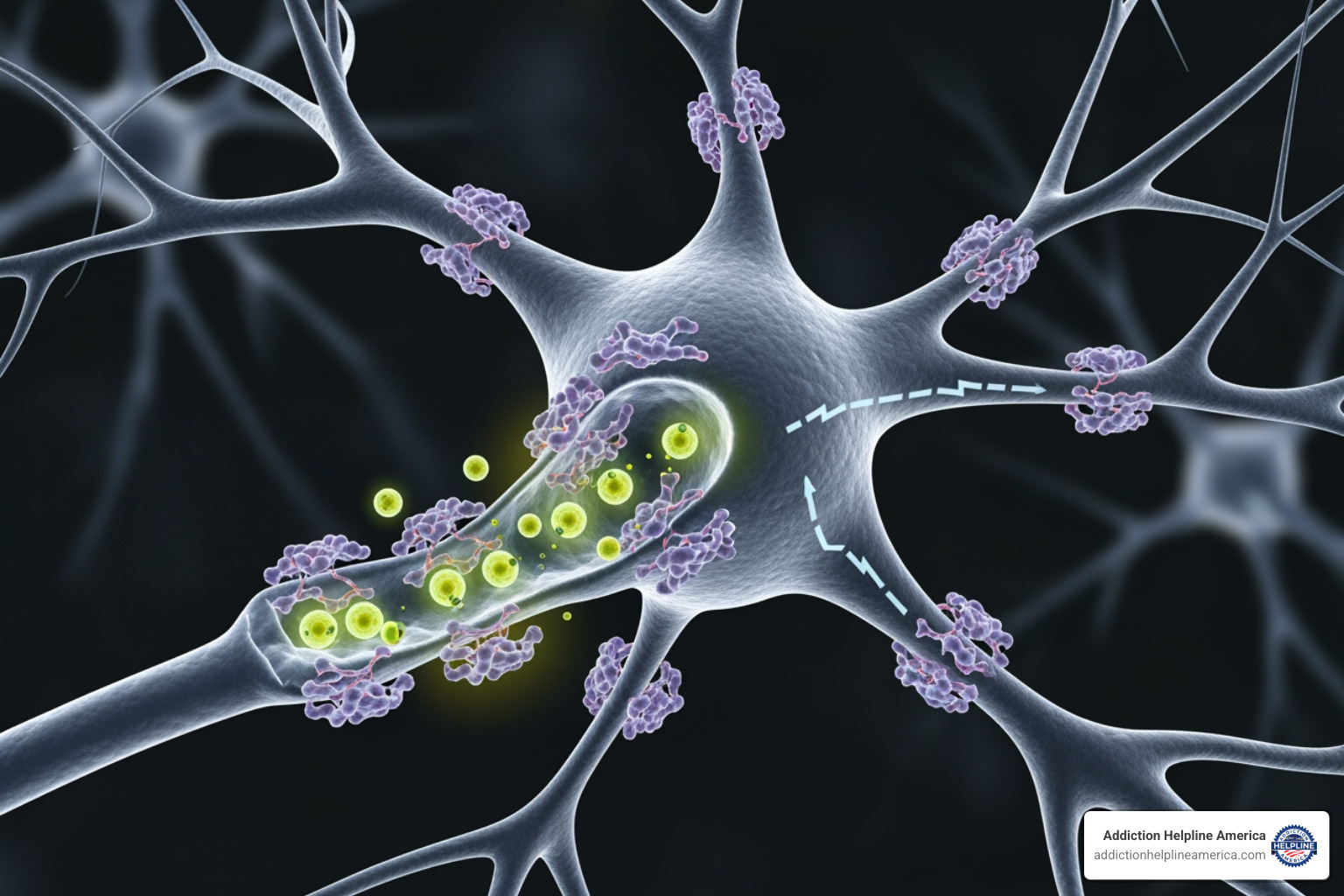
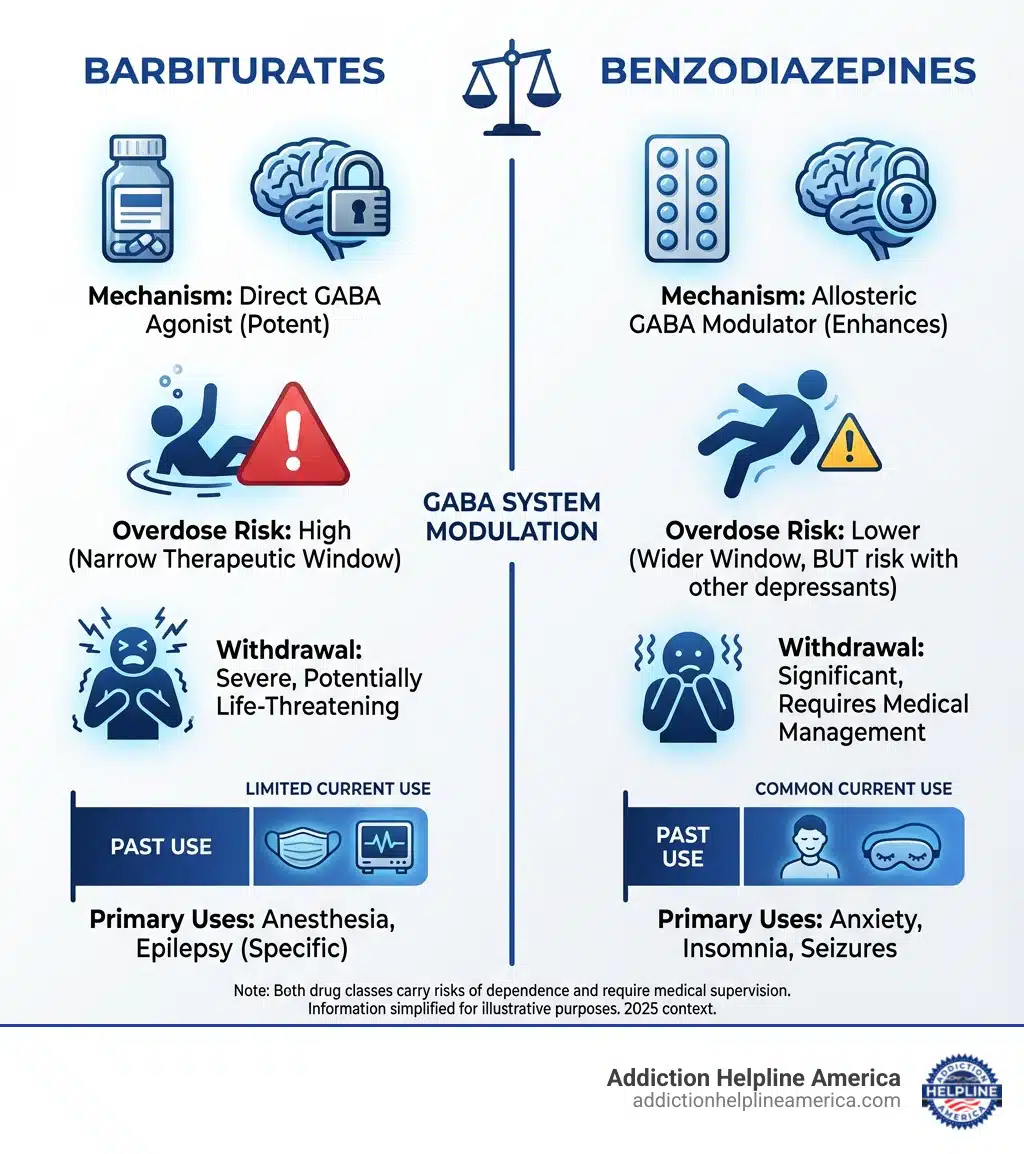
Mechanism of Action: How They Affect the Brain
The primary distinction between barbiturates and benzodiazepines lies in their specific interaction with GABA receptors. Think of GABA receptors as tiny gates on brain cells that, when opened, allow negatively charged ions to flow in, making the cell less likely to fire. This reduces overall brain activity.
-
Barbiturates: These drugs are like a heavy hand on the gate. They directly stimulate GABA receptors and cause the chloride ion channels to remain open for a prolonged duration. This leads to a strong, sustained influx of negative ions, resulting in a profound and generalized depression of the central nervous system. At higher concentrations, barbiturates can even open these channels in the absence of GABA, making them incredibly potent and dangerous. Their effect is less specific and more widespread throughout the brain.
-
Benzodiazepines: In contrast, benzodiazepines are more like a gentle nudge. They don’t directly open the GABA channels. Instead, they improve the efficiency of GABA receptors by increasing the frequency of channel opening when GABA is already present. This means they make the brain’s natural calming system work better, but they rely on the presence of GABA to do so. This “indirect” action makes them less likely to cause a fatal overdose on their own compared to barbiturates, as there’s a ceiling to their effect. As one source puts it, benzodiazepines change the voltage in the brain from positive to negative and cause brain cells to be less sensitive, but they don’t have as depressive an effect as barbiturates.
This difference in mechanism directly influences their potency, duration of effect, addictiveness, and overall danger profile. Barbiturates bind to more GABA receptors and keep them open longer, strongly affecting the entire body. Benzodiazepines, on the other hand, bind to more specific GABA receptors, causing the brain to be less receptive to impulses, leading to more precise and less potent sedative effects.
Therapeutic Index and Overdose Risk
The “therapeutic index” is a fancy term for the ratio between a drug’s effective dose and its toxic dose. This is where the stark differences between barbiturates vs benzo become critically important.
| Factor | Barbiturates | Benzodiazepines |
|---|---|---|
| Mechanism | Prolong GABA channel opening | Increase frequency of GABA channel opening |
| Overdose Risk | Very High (narrow therapeutic window) | Lower (wider safety margin) |
| Addiction Potential | Extremely High | High |
| Medical Use | Rare (anesthesia, severe seizures) | Common (anxiety, insomnia, seizures) |
| Withdrawal Severity | Life-threatening (seizures, psychosis) | Life-threatening (seizures, rebound anxiety) |
Barbiturates have a notoriously narrow therapeutic index. This means the difference between a dose that provides the desired therapeutic effect and a dose that causes severe respiratory depression, coma, or even death is frighteningly small. For barbiturates, a dose just ten times the therapeutic amount can be fatal. This narrow window makes them incredibly dangerous, especially when misused.
Benzodiazepines, in contrast, have a much wider safety margin. An overdose typically requires a dose a hundred times the therapeutic amount to be fatal, though this is significantly reduced when other substances are involved. This wider margin is a key reason why benzodiazepines largely replaced barbiturates in medical practice.
However, “safer” does not mean “safe,” particularly when it comes to polydrug use. The most significant danger for both classes, but especially for benzodiazepines, comes from combining them with other central nervous system depressants. Mixing either barbiturates or benzodiazepines with substances like alcohol, opioids, or even other sedatives dramatically amplifies the depressive effects on the brain and respiratory system. This can lead to:
- Profound sedation
- Respiratory depression (slowed or stopped breathing)
- Coma
- Death
This is not a hypothetical danger; it’s a tragic reality we see across the nation, from busy cities like Los Angeles and New York City to smaller communities. In 2013 alone, barbiturates were linked to nearly 400 deaths in the United States, often involving polydrug use and suicide. The FDA has even issued warnings about the risks of combining benzodiazepines with opioids due to the heightened risk of respiratory depression.
If you or a loved one are mixing substances, call Addiction Helpline America at 844-561-0606 for immediate, confidential help. We’re here 24/7 to guide you to safety.
Medical Uses and Prescription Trends
The history of barbiturates vs benzo is a clear example of medical evolution driven by safety concerns.
Barbiturates were once the go-to for anxiety, insomnia, and seizure control. Their efficacy was undeniable, but the high risk of fatal overdose and addiction led to a significant decline in their use. Today, barbiturate use is mostly limited to very specific, controlled settings, such as:
- Pre-operative settings: As an anesthetic.
- Specific types of epilepsy: When other medications are ineffective.
- Emergency seizure control: In acute situations.
- Euthanasia: In veterinary medicine and, in some jurisdictions, in human medicine.
If prescribed for ailments, it’s typically for a very short duration.
Benzodiazepines, on the other hand, became the “2.0” version of sedatives. Introduced as a safer alternative, they quickly gained popularity and are now among the most widely prescribed medications in the U.S. They’re used for a broad range of conditions, including:
- Anxiety disorders: From generalized anxiety to panic attacks.
- Insomnia: Though typically recommended for short-term use.
- Seizure disorders: For acute and chronic management.
- Alcohol withdrawal: A standard of care for managing symptoms.
- Muscle spasms: To relieve tension and pain.
Despite their widespread use and perceived safety advantage over barbiturates, benzodiazepines are not without their problems. They are typically only prescribed for short-term use due to the significant risk of developing tolerance and dependence. Long-term use, even as prescribed, can lead to physical and psychological dependence, making cessation difficult and dangerous.
If you have questions about your prescription or are concerned about misuse, Addiction Helpline America is here to help at 844-561-0606. We can connect you with resources and support across states like Florida, Georgia, North Carolina, and Pennsylvania.
The Shared Dangers: Addiction, Withdrawal, and Side Effects
The allure of quick relief from anxiety or insomnia offered by both barbiturates vs benzo can quickly pave the path to dependence and addiction. While benzodiazepines are generally considered safer than barbiturates, both drug classes carry significant risks, especially with prolonged use or misuse.
The Path to Dependence and Addiction
Tolerance is often the first step down the path to dependence. This occurs when your body adapts to the presence of the drug, requiring higher and higher doses to achieve the same desired effect. As tolerance builds, physical dependence can develop rapidly. This means your body literally becomes accustomed to the drug’s presence and needs it to function normally.
According to SAMHSA’s 2019 annual substance use survey, nearly 6 million Americans misused prescription tranquilizers or sedatives, a category that includes both benzos and barbiturates. This statistic highlights the widespread nature of the problem. Sadly, we see individuals in all our service areas, from the busy streets of Chicago to the quiet communities of Oregon, struggling with this challenge.
Signs of addiction can manifest in various ways, including:
- Taking more of the medication than prescribed or for longer periods.
- Feeling a compulsive need to use the drug.
- Experiencing withdrawal symptoms when trying to stop or reduce use.
- Neglecting responsibilities at work, school, or home due to drug use.
- Continuing to use the drug despite negative consequences.
- Spending a significant amount of time obtaining, using, or recovering from the drug.
While barbiturates have an extremely high addiction potential, benzodiazepines are also highly habit-forming. For instance, close to 40% of Xanax users will develop a habit. The historical data shows a clear trend: the percentage of 12th-grade students reporting barbiturate use in the previous 30 days declined from 4.7% in 1975 to 1.7% in 1994, a 64% decline, as benzodiazepines became more prevalent. However, this shift didn’t eliminate the problem of sedative misuse; it merely changed its form.
If you notice signs of addiction in yourself or someone you care about, call Addiction Helpline America at 844-561-0606 for support and resources. Our compassionate team is ready to help you find the right path to recovery.
The Risks of Withdrawal: Why You Need Medical Help
Perhaps one of the most critical, and often overlooked, dangers associated with both barbiturates vs benzo is the severity of withdrawal. Abruptly stopping either drug can trigger a range of severe, potentially life-threatening symptoms. This is not just discomfort; it’s a medical emergency.
Withdrawal symptoms can include:
- Severe anxiety and panic attacks: Often worse than the original condition the medication was prescribed for (known as a “rebound effect”).
- Insomnia: Another rebound effect, leading to severe sleep deprivation.
- Sweating, tremors, and muscle pain.
- Nausea and vomiting.
- Hallucinations: Seeing or hearing things that aren’t there.
- Psychosis: A severe mental disorder where thoughts and emotions are so impaired that contact is lost with external reality.
- Seizures: Potentially fatal grand mal seizures.
Barbiturate withdrawal is particularly dangerous, carrying a higher risk of fatal seizures compared to benzodiazepine withdrawal. Some withdrawal symptoms from barbiturates have even been reported to last for years.
This is why medical detox is absolutely essential. Attempting to quit “cold turkey” can be fatal. A medically supervised detoxification program provides a safe environment where healthcare professionals can monitor your vital signs, manage symptoms, and slowly taper the medication. This gradual reduction minimizes the shock to your system and reduces the risk of severe complications.
Withdrawal from sedatives can be fatal. Do not attempt to quit alone. Call Addiction Helpline America at 844-561-0606 for guidance on safe medical detox. We can connect you with facilities that offer medically supervised detox across all our service areas, from Arizona to Virginia.
Common and Severe Side Effects
Beyond the risks of addiction and withdrawal, both barbiturates vs benzo come with a host of common and severe side effects that can impact daily life and long-term health.
Common Side Effects:
- Drowsiness and sedation: This is the intended effect but can be excessive, leading to impaired driving and occupational hazards.
- Confusion and impaired memory: Especially with benzodiazepines, where individuals may underestimate their impairment.
- Impaired coordination: Leading to increased risk of falls and accidents.
- Slurred speech.
- Dizziness and lightheadedness.
- Nausea, vomiting, and abdominal pain.
- Changes in appetite or weight.
Severe Side Effects:
- Respiratory depression: A dangerous slowing or stopping of breathing, especially critical with barbiturates or when mixed with other depressants.
- Coma and death: The ultimate tragic outcome of severe overdose or respiratory depression.
- Jaundice: A rare but serious liver-related side effect of benzodiazepines.
- Long-term cognitive effects: Chronic use can lead to persistent memory problems and cognitive impairment.
- Paradoxical reactions: In some individuals, these drugs can cause agitation, aggression, or hallucinations instead of sedation.
Pregnancy Risks:
Both drug classes pose significant risks during pregnancy.
- Benzodiazepines are classified as FDA Pregnancy Category D, meaning there is positive evidence of human fetal risk. They can cause fetal harm and enter breast milk, potentially leading to lethargy and weight loss in newborns. Therefore, they should not be used by nursing mothers.
- Barbiturates also fall into Pregnancy Category D for some types (like phenobarbital, pentobarbital, and secobarbital), while others are Category C. There is no established evidence of safe use for pregnant women, and they should be avoided in nursing mothers to prevent harm to the infant.
While these medications can offer relief, they are not without significant risks. We always encourage individuals to discuss all potential side effects and risks with their prescribing physician.
If you are experiencing side effects or have concerns about your medication, reach out to Addiction Helpline America at 844-561-0606. Our specialists can provide guidance and connect you with medical professionals who can address your concerns.
Frequently Asked Questions about Barbiturates vs Benzo
We often hear similar questions from individuals and families trying to understand the complexities of barbiturates vs benzo. Here are some of the most common ones:
Which is more dangerous, a barbiturate or a benzodiazepine?
Generally, barbiturates are considered more dangerous than benzodiazepines. This primarily stems from their narrow therapeutic index, meaning the gap between an effective dose and a toxic or fatal dose is very small. For barbiturates, a dose just ten times the therapeutic amount can be lethal, leading to severe respiratory depression and death.
Benzodiazepines, while still dangerous, have a wider safety margin. An overdose typically requires a much higher dose to be fatal on its own (around a hundred times the therapeutic dose). However, this safety advantage is completely negated when benzodiazepines are combined with other CNS depressants like alcohol or opioids, making them equally deadly in such scenarios. So, while benzos are “safer” in isolation, their widespread misuse and combination with other substances make them a significant public health concern.
For more information or help, call Addiction Helpline America at 844-561-0606.
Can you take barbiturates and benzodiazepines together?
Absolutely not. Taking barbiturates and benzodiazepines together is extremely dangerous and can be fatal. Both are powerful CNS depressants that intensify each other’s effects. Combining them exponentially increases the risk of:
- Profound sedation
- Respiratory depression (slowed or stopped breathing)
- Coma
- Death
This combination is a recipe for disaster, and healthcare professionals strongly advise against it. The same goes for mixing either drug class with alcohol, opioids, or other sedatives.
If you or someone you know is combining these medications, call Addiction Helpline America at 844-561-0606 immediately. We can provide urgent guidance and connect you with life-saving help in any of our covered states, from Alaska to Wyoming.
Is withdrawal from benzos or barbs life-threatening?
Yes, withdrawal from both barbiturates and benzodiazepines can be life-threatening. The abrupt cessation of these medications, especially after prolonged use or high doses, can trigger severe and dangerous symptoms. These can include:
- Intense anxiety and panic attacks
- Severe insomnia
- Tremors
- Hallucinations
- Psychosis
- Grand mal seizures
These seizures are particularly dangerous and can lead to serious injury or death. Due to these severe risks, attempting to detox from either drug class without medical supervision is highly discouraged. A medically supervised detoxification program is essential to ensure safety and manage symptoms effectively. Healthcare providers can gradually taper the dosage, minimizing withdrawal discomfort and preventing life-threatening complications.
Call Addiction Helpline America at 844-561-0606 for safe, professional detox options. We can help you find a suitable facility in your area.
Finding Help for Sedative Addiction
The journey to recovery from addiction to powerful sedatives like barbiturates vs benzo can feel overwhelming, but it’s a path that many successfully steer every day. We at Addiction Helpline America understand the complexities involved and are here to provide the compassionate support and guidance you need.
The first and most critical step is acknowledging the problem and seeking professional treatment. Given the life-threatening nature of withdrawal from these drugs, medical detox is usually the recommended starting point. During medical detox, healthcare professionals will:
- Monitor your vital signs around the clock.
- Administer medications to manage withdrawal symptoms.
- Ensure your safety and comfort as your body clears the substance.
After detox, a comprehensive treatment program is crucial for long-term recovery. These programs can vary and may include:
- Inpatient programs: Providing a structured, residential environment away from triggers.
- Outpatient programs (IOPs and PHPs): Offering intensive therapy while allowing you to live at home or in a sober living environment.
- Therapies: Evidence-based approaches like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) help address underlying issues, develop coping mechanisms, and prevent relapse.
- Dual diagnosis treatment: Many individuals struggling with sedative addiction also have co-occurring mental health conditions like anxiety or depression. Effective treatment addresses both simultaneously.
- Medication-Assisted Treatment (MAT): In some cases, medications may be used to support recovery, reduce cravings, or manage co-occurring disorders.
Addiction Helpline America is dedicated to connecting individuals nationwide to addiction and mental health treatment centers. We offer a free, confidential, and personalized guidance service to help you find the right recovery program from our vast network of trusted facilities. Whether you’re in California, New York, Texas, or any other state we serve, we can help you find a program that fits your unique needs, including options that accept various insurance plans like private insurance, Medicaid, or Medicare.
Don’t wait to seek help. Our compassionate specialists are available to guide you toward the right treatment program and a healthier future.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.