Understanding Barbiturates Overdose: A Life-Threatening Medical Emergency
Barbiturates overdose is a serious, potentially fatal medical emergency that requires immediate intervention. If someone has taken too much of these powerful sedative medications, here’s what you need to know right now:
Immediate Actions for Barbiturates Overdose:
- Call 911 immediately – This is a life-threatening emergency
- Contact Poison Control at 1-800-222-1222 for expert guidance
- Do NOT induce vomiting or give food/water
- Keep the person on their side to prevent choking
- Stay with them until help arrives
Critical Warning Signs:
- Extremely slow or stopped breathing
- Unconsciousness or unresponsive
- Weak pulse and clammy skin
- Dilated pupils
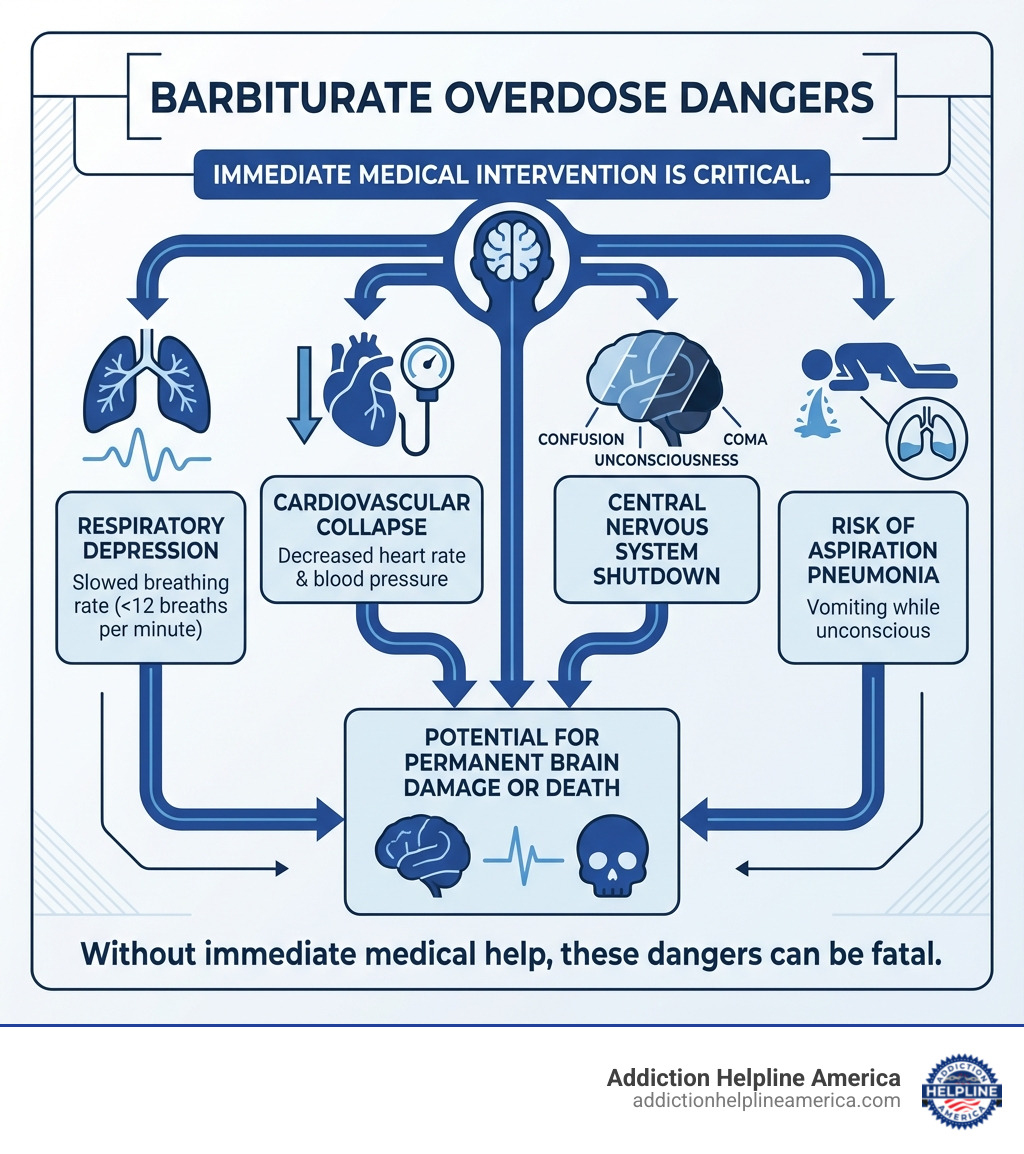
Barbiturates are central nervous system (CNS) depressants that slow down vital functions like breathing and heart rate. When someone takes too much—whether accidentally or intentionally—these drugs can cause respiratory depression, coma, and death. About 1 in 10 people who overdose on barbiturates will die, usually from respiratory failure and related complications.
The danger increases dramatically when barbiturates are mixed with other substances like alcohol, opioids, or benzodiazepines. There is no specific antidote for barbiturate overdose, making rapid medical intervention the only path to survival.
Time is critical. Every minute counts in a barbiturate overdose situation. The faster someone receives medical care, the better their chances of recovery.
At Addiction Helpline America, we’ve helped countless individuals and families steer the crisis of barbiturates overdose and connect with life-saving treatment resources. Our 24/7 helpline at 844-561-0606 provides immediate, confidential support when you need it most—whether you’re facing an emergency or seeking help for addiction recovery.
Barbiturates overdose basics:
Recognizing the Signs: Symptoms of Barbiturate Intoxication and Overdose
Understanding the difference between barbiturate intoxication and a full-blown barbiturates overdose is crucial, though both require attention. Barbiturates are powerful central nervous system depressants, meaning they slow down brain activity. This can lead to a range of effects, from mild sedation to a life-threatening coma. When someone has taken too many barbiturates, their body and mind will show distinct physical and behavioral changes. These changes are often described as a “sedative-hypnotic toxidrome” by medical professionals, indicating a specific pattern of symptoms caused by sedative drugs.
Symptoms of Barbiturate Intoxication
Even without reaching a full overdose, taking more barbiturates than prescribed or intended can lead to intoxication, which impairs a person’s judgment and physical abilities. These symptoms indicate that the central nervous system is significantly depressed:
- Drowsiness: Feeling unusually sleepy or lethargic.
- Slurred speech: Difficulty articulating words clearly, similar to someone who has consumed too much alcohol.
- Poor coordination: Struggling with balance, walking, or fine motor skills. This can manifest as staggering or an unsteady gait.
- Faulty judgment: Making poor decisions or acting impulsively.
- Nystagmus: Involuntary, rapid eye movements, often from side to side.
- Confusion: Disorientation about time, place, or person.
- Difficulty thinking: Problems concentrating or processing information.
- Sluggishness: A general lack of energy or responsiveness.
These signs, while not immediately life-threatening on their own, are clear indicators that a person is under the influence of too many barbiturates and needs close monitoring. They also significantly increase the risk of accidents, such as falls, which can lead to further injuries.
Life-Threatening Symptoms of a Barbiturates Overdose
When intoxication progresses to a full barbiturates overdose, the body’s vital functions can shut down, leading to a critical medical emergency. The symptoms become much more severe and directly threaten life:
- Shallow breathing or respiratory depression: Breathing becomes very slow, weak, or even stops entirely (apnea). This is the most dangerous symptom, as a lack of oxygen quickly leads to brain damage and death. Barbiturates depress the medullary respiratory center, which controls breathing.
- Weak and rapid pulse: The heart may struggle to pump blood effectively, leading to a weak, thready pulse. At higher doses, cardiovascular depression can occur, potentially leading to cardiovascular collapse and dangerously low blood pressure (hypotension).
- Clammy skin: The skin may feel cold and moist due to poor circulation.
- Dilated pupils: The pupils of the eyes may become enlarged and unresponsive to light.
- Profound coma: The person becomes unresponsive to external stimuli, unable to be roused. This is a deep state of unconsciousness where brainstem reflexes may be suppressed.
These severe symptoms represent a direct threat to life and demand immediate emergency medical intervention. Without quick action, the consequences can be devastating, including permanent disability or death.
Chronic Symptoms of Barbiturate Abuse
Long-term misuse of barbiturates, even without acute overdose, can lead to chronic symptoms and significant health problems. The body can develop physical dependence rapidly, meaning it needs the drug to function “normally.” This dependence is distinct from addiction but often co-occurs. According to scientific research on sedative misuse, chronic symptoms may include:
- Memory loss: Persistent difficulty recalling information or forming new memories.
- Irritability: Increased agitation or short temper.
- Changes in alertness: Fluctuations between excessive drowsiness and periods of restlessness.
- Decreased functioning: A general decline in cognitive and physical abilities, impacting daily life, work, and relationships.
These chronic issues highlight the pervasive negative impact barbiturate misuse can have on a person’s life, even outside of acute overdose situations. For more detailed information on the effects of sedative misuse, you can refer to Scientific research on sedative misuse. If you recognize these signs in yourself or someone you care about, please know that help is available. Contact Addiction Helpline America at 844-561-0606 for confidential support and guidance.
Immediate Steps to Take During a Barbiturates Overdose Emergency
When faced with a suspected barbiturates overdose, quick and decisive action can be the difference between life and death. This is not a situation for hesitation or self-diagnosis; it’s a critical medical emergency that demands professional help. Your role as a bystander is to recognize the danger, call for help, and provide basic supportive care until emergency services arrive. For guidance, call our 24/7 helpline at 844-561-0606.
Step 1: Call 911 Immediately
This is the absolute top priority. Do not delay, even if you are unsure of the exact substance or amount taken. The faster emergency medical services (EMS) can reach the individual, the better their chances of survival and recovery.
When you call 911, be prepared to provide the dispatcher with crucial information:
- Your precise location: This ensures EMS can find you quickly.
- The person’s condition: Describe what you observe – are they unconscious? Are they breathing? What are their symptoms?
- Breathing status: Specifically mention if their breathing is shallow, labored, or if they have stopped breathing entirely. This information is vital for EMS to prepare their response.
- Information about the substance (if known): If you know the person’s age, weight, the name of the product (and its ingredients/strength), the approximate time it was swallowed, and the amount taken, share this with the dispatcher. However, do NOT delay calling for help if this information is not immediately available. Getting help en route is more important than gathering every detail beforehand.
EMS professionals are trained for these situations and will provide life-saving care upon arrival.
Step 2: Contact Poison Control
After calling 911, or if advised by the 911 dispatcher, contact your local poison control center. You can reach the national toll-free Poison Help hotline at 1-800-222-1222 from anywhere in the United States. This service offers expert, free, and confidential advice 24 hours a day, 7 days a week.
Poison control specialists can provide:
- Expert guidance: They can offer specific instructions custom to the situation, sometimes even before EMS arrives.
- Additional information: They can help clarify what to expect and what actions to take.
- Support: They can stay on the line with you, offering reassurance and guidance until help arrives.
Always follow the instructions given by poison control experts.
Step 3: Provide Supportive Care While Waiting for Help
While waiting for emergency services, there are a few critical things you can do to help the person:
- Check for breathing: If the person is not breathing, and you are trained in CPR, begin chest compressions.
- Place the person in the recovery position: If the person is unconscious but breathing, gently roll them onto their side. This helps prevent them from choking on vomit or saliva, which is a common and dangerous complication in overdose situations.
- Prevent aspiration (choking): Ensure their airway is clear. Loosen any tight clothing around their neck.
- Keep the person warm: Overdose can lead to a drop in body temperature (hypothermia). Cover them with a blanket if available.
- DO NOT induce vomiting: Trying to make the person vomit can cause them to choke, especially if their consciousness is impaired.
- DO NOT give food or liquids: If the person is unconscious or has a decreased level of consciousness, giving them anything by mouth can lead to aspiration.
- Stay with them: Do not leave the person alone. Continue to monitor their breathing and responsiveness until medical professionals take over.
Your calm and quick response can significantly improve the outcome for someone experiencing a barbiturates overdose.
Medical Treatment and What to Expect at the Hospital
Once emergency medical services arrive and transport the individual to a hospital, they will receive specialized medical care for a barbiturates overdose. The primary goal of treatment is to support the person’s vital functions and help their body eliminate the drug. While barbiturate overdoses were once a more common cause of death, advancements in emergency medicine have significantly improved survival rates. With appropriate supportive care, in-hospital mortality for barbiturate toxicity ranges from 0.5% to 2%. However, severe cases can still lead to prolonged complications or permanent disability.
Emergency Room Procedures for Overdose
Upon arrival at the emergency room, a team of healthcare providers will immediately begin a series of diagnostic and treatment procedures:
- Vital signs monitoring: Continuous monitoring of heart rate, blood pressure, respiratory rate, and oxygen saturation is crucial.
- Airway management: If the person’s breathing is compromised or they are unconscious and unable to protect their airway, medical staff may perform endotracheal intubation, inserting a tube into the windpipe to connect to a mechanical ventilator.
- Mechanical ventilation: For severe respiratory depression or apnea, a ventilator will breathe for the person until the effects of the barbiturates wear off.
- Intravenous (IV) fluids: Administered to maintain hydration, support blood pressure, and help with drug elimination.
- Activated charcoal: If the barbiturates were ingested recently (typically within an hour or two), activated charcoal may be given orally or through a tube. It works by binding to the drug in the stomach and intestines, preventing its absorption into the bloodstream. Multiple doses might be considered for long-acting barbiturates like phenobarbital.
- Blood and urine tests: These tests help confirm the presence of barbiturates, assess the severity of the overdose, and check for any co-ingested substances or complications.
- Electrocardiogram (ECG): To monitor heart rhythm and detect any cardiac issues caused by the overdose.
- Other tests: Depending on the patient’s condition, a chest X-ray may be done to check for aspiration pneumonia, and a CT scan might be performed to rule out other causes of altered mental status.
The Role of Naloxone in a Suspected Barbiturates Overdose
It’s important to clarify the role of Naloxone (often known by the brand name Narcan) in a barbiturates overdose. Naloxone is a life-saving medication that rapidly reverses the effects of an opioid overdose. It works by blocking opioid receptors in the brain.
However, Naloxone is not an antidote for barbiturates alone. Barbiturates and opioids affect the brain through different mechanisms. Therefore, if a person has only taken barbiturates, Naloxone will not reverse the overdose symptoms.
The exception is in cases of polydrug use or co-ingestion where opioids are also involved. Since polydrug use has long been associated with barbiturate abuse, and barbiturates have historically been a secondary drug of abuse for people who misuse alcohol and heroin, medical professionals may administer Naloxone if they suspect an opioid is also present. This is a common practice in emergency settings where the exact substances ingested may not be immediately known. If Naloxone is given and the person improves, it suggests opioid involvement. If there’s no improvement, the treatment will focus solely on managing the barbiturate overdose. For more information on mixing barbiturates with other drugs, see Information on mixing barbiturates with other drugs.
Advanced Treatments for Severe Cases
For individuals with severe barbiturates overdose or those who don’t respond to initial supportive care, more advanced treatments may be necessary, often requiring transfer to an Intensive Care Unit (ICU):
- Intensive Care Unit (ICU): Patients with profound coma, persistent respiratory failure, or cardiovascular instability will be admitted to the ICU for continuous, specialized monitoring and treatment.
- Hemodialysis: In select and extreme cases, particularly with long-acting barbiturates like phenobarbital, hemodialysis may be used. This procedure acts like an artificial kidney, filtering the barbiturates directly from the blood, accelerating their elimination from the body.
- Multi-dose activated charcoal: For severe toxicity, especially with long-acting barbiturates, repeated doses of activated charcoal may be given to interrupt enterohepatic recirculation and promote further elimination of the drug.
- Urinary alkalinization: While its efficacy is debated and it’s less commonly used now than in the past, urinary alkalinization with sodium bicarbonate can, in theory, help increase the excretion of certain barbiturates by making the urine more alkaline. This is typically reserved for specific situations and requires careful monitoring.
The prognosis for barbiturate overdose depends heavily on the severity of the overdose and how quickly treatment is received. With prompt and appropriate medical care, many individuals can recover. However, prolonged coma, respiratory complications, or shock can lead to permanent disability. Once a person is medically stable, the next step is addressing the underlying addiction. Addiction Helpline America can help you find the right treatment program. Call us at 844-561-0606 to explore recovery options.
The Dangers of Barbiturate Misuse and Withdrawal
The risks associated with barbiturates extend far beyond acute overdose. These drugs carry a significant potential for addiction, physical dependence, and dangerous withdrawal symptoms. For anyone struggling with barbiturate misuse, we at Addiction Helpline America are here to help. Call us at 844-561-0606 for confidential help.
Why Barbiturates Are So Risky: Tolerance and Polydrug Use
Barbiturates are a class of drugs with a narrow therapeutic index. This means there’s a small difference between a dose that provides therapeutic effects and a dose that causes toxicity or death. This inherent characteristic makes them highly dangerous when misused.
- High addiction potential: Barbiturates are highly addictive, and physical dependence can develop rapidly, sometimes even with prescribed use.
- Tolerance development: With repeated use, the body quickly develops tolerance to the mood-altering effects of barbiturates, meaning a person needs to take larger doses to achieve the same desired effect. However, tolerance to the lethal effects (like respiratory depression) develops much more slowly. This creates a perilous situation where an individual might take increasingly larger doses, unknowingly approaching the lethal threshold. As little as a 10% to 25% increase over a usual daily dosage may be fatal to an addict whose tolerance has narrowed this therapeutic window.
- Increased overdose risk: This discrepancy in tolerance development is a primary reason why barbiturates are so dangerous.
- Dangers of mixing with alcohol: Polydrug use has long been associated with barbiturate abuse. Co-administering barbiturates with alcohol is extremely dangerous. Both substances are central nervous system depressants, and their effects are additive, significantly increasing the risk of profound respiratory depression, coma, and death.
- Dangers of mixing with opioids: Similarly, combining barbiturates with opioids like heroin or prescription painkillers also drastically increases the risk of overdose. This combination also leads to additive depressant effects on the CNS, making respiratory failure much more likely.
Some common barbiturates, though less frequently prescribed today, include:
- Phenobarbital
- Secobarbital
- Butalbital (often found in combination pain medications)
The combination of a narrow therapeutic index, rapid tolerance development, and the additive effects with other depressants makes barbiturates incredibly risky drugs to misuse.
Barbiturate Withdrawal: A Medical Emergency
Once physical dependence has developed, stopping barbiturate use abruptly can trigger a severe and potentially life-threatening withdrawal syndrome. Unlike some other drug withdrawals, barbiturate withdrawal is considered a medical emergency and requires professional medical supervision.
Withdrawal symptoms can begin within 8 to 15 hours of stopping the drug, or even within 2 hours for some related substances like phenibut. Minor withdrawal symptoms usually begin 24 to 36 hours after the last dose, while major symptoms, including convulsions and delirium, can appear between the third and seventh days, sometimes as late as 14 days. These symptoms include:
- Restlessness and anxiety: Intense feelings of unease and nervousness.
- Tremors: Uncontrollable shaking.
- Liftd body temperature: Fever.
- Sweating: Profuse perspiration.
- Insomnia: Severe difficulty sleeping.
- Seizures: These are a particularly dangerous complication and can be grand mal seizures, posing a significant risk of injury or death.
- Delirium: Severe confusion, disorientation, and sometimes hallucinations.
Attempting to detox from barbiturates at home without medical assistance is extremely dangerous and can be fatal due to the risk of seizures and other severe complications.
Finding Help for Barbiturate Addiction
If you or a loved one is struggling with barbiturate misuse, dependence, or addiction, help is available. Recovery is a journey that often begins with professional medical support.
- Medical detox: This is the crucial first step. During medical detoxification, individuals are monitored 24/7 by medical professionals in a specialized treatment facility. Dosages are gradually tapered off by doctors to safely wean the individual off barbiturates, minimizing severe withdrawal symptoms and preventing life-threatening complications like seizures. This process ensures the person’s safety and comfort.
- Inpatient treatment: Following detox, many individuals benefit from inpatient treatment programs. These programs provide a structured, supportive environment with 24/7 care, allowing individuals to focus entirely on their recovery away from external triggers.
- Cognitive Behavioral Therapy (CBT): A widely used and effective therapy, CBT helps individuals identify and change negative thought patterns and behaviors that contribute to drug use. It teaches coping mechanisms and strategies for relapse prevention, which are essential for long-term sobriety.
- Support groups: Participation in support groups like Alcoholics Anonymous and Narcotics Anonymous can provide invaluable peer support, shared experiences, and a sense of community during recovery.
- Long-term recovery: Addiction is a chronic disease, and long-term sobriety is achieved through ongoing commitment to learned behaviors from therapy, support from family, medical professionals, and community support groups.
We at Addiction Helpline America understand the complexities of barbiturate addiction. We can connect you with treatment centers across the country, including those in Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, Virginia, Washington, West Virginia, Wisconsin, and Wyoming. Call 844-561-0606 to discuss treatment options custom to your needs.
Frequently Asked Questions about Barbiturate Overdose
What are barbiturates and what are they used for?
Barbiturates are a group of sedative-hypnotic drugs derived from barbituric acid. They act as central nervous system depressants, slowing down brain activity by enhancing the action of the neurotransmitter GABA. Historically, they were widely used for a broad range of medical purposes, including:
- Treating seizure disorders (epilepsy), with phenobarbital being a notable example.
- Managing insomnia and other sleep disorders.
- Reducing anxiety and tension.
- Providing anesthesia during surgery.
- Inducing a coma for increased intracranial pressure (ICP) in critical care settings.
However, due to their narrow therapeutic index, high potential for addiction, and the severe risks associated with overdose, barbiturates have largely been replaced by safer alternatives, primarily benzodiazepines, for many of these indications.
Is there an antidote for barbiturate overdose?
No, there is no specific antidote that can directly reverse the effects of a barbiturate overdose. This is a critical difference compared to opioid overdoses, which can be reversed by Naloxone.
Treatment for barbiturates overdose is primarily supportive care. This means medical professionals focus on:
- Maintaining the person’s breathing (often with mechanical ventilation).
- Supporting their blood pressure and circulation.
- Helping the body eliminate the drug through methods like activated charcoal or, in severe cases, hemodialysis.
The absence of a direct antidote underscores the importance of rapid medical intervention and aggressive supportive care to manage the overdose and prevent life-threatening complications.
How deadly is a barbiturate overdose?
A barbiturate overdose can be fatal. Approximately 1 in 10 people who overdose on barbiturates or a mixture that contains them will die. Death typically occurs due to profound respiratory depression, meaning the person stops breathing, leading to a lack of oxygen to the brain and other vital organs.
The deadliness of a barbiturate overdose is significantly increased when:
- Mixed with other depressants: Combining barbiturates with alcohol, opioids, or benzodiazepines creates an additive depressant effect, greatly escalating the risk of respiratory and cardiovascular collapse.
- Tolerance issues: As discussed, tolerance to the mood-altering effects develops faster than tolerance to the lethal effects, making it easy for individuals to accidentally take a fatal dose.
- Delayed medical attention: The prognosis for a barbiturate overdose depends heavily on the severity of the overdose and, crucially, how quickly professional medical treatment is received. The faster the intervention, the better the chances of survival and avoiding long-term complications. If you have more questions about barbiturate addiction and the path to recovery, our team at Addiction Helpline America is here to help. Call our confidential helpline 24/7 at 844-561-0606 for answers and support.
Conclusion: Your Path to Recovery Starts Now
Experiencing or witnessing a barbiturates overdose is a terrifying and life-altering event. We’ve explored the critical signs of intoxication and overdose, emphasizing that immediate action, starting with a call to 911 and poison control, is paramount. We’ve also dug into the life-saving medical treatments available in hospitals and the profound dangers of barbiturate misuse, including the severe and potentially fatal withdrawal syndrome.
An overdose is a medical crisis, and barbiturate withdrawal is also a dangerous process that requires professional medical supervision. But there is hope for recovery. Long-term treatment, including medically supervised detox, inpatient or outpatient programs, and evidence-based therapies like Cognitive Behavioral Therapy, can be incredibly effective in helping individuals achieve lasting sobriety.
At Addiction Helpline America, we are dedicated to guiding you or your loved ones through these challenging times. We offer free, confidential, and personalized guidance to connect you with the right recovery program from our vast network. Don’t face this alone. Our team is available around the clock to help you find the right treatment program. Your path to recovery starts now.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.