Why Medical Supervision is Critical When Stopping Alcohol
Alcohol withdrawal is a potentially life-threatening condition that occurs when a person who drinks heavily suddenly stops or cuts back. Their brain and body have physically adapted to alcohol, and its removal sends the nervous system into overdrive.
Symptoms typically begin 6-24 hours after the last drink, with the peak danger period for seizures and delirium tremens (DTs) occurring at 24-72 hours. About half of people with alcohol use disorder experience withdrawal, with symptoms ranging from mild tremors and anxiety to life-threatening seizures. Quitting “cold turkey” without medical help can be deadly, as DTs have a 1-5% mortality rate even with treatment.
Common symptoms include:
- Anxiety and restlessness
- Trembling hands (the “shakes”)
- Sweating and rapid heartbeat
- Nausea and vomiting
- Confusion and hallucinations
- Seizures
- Delirium tremens (DTs): a medical emergency with severe confusion, fever, and dangerous changes in heart rate and blood pressure
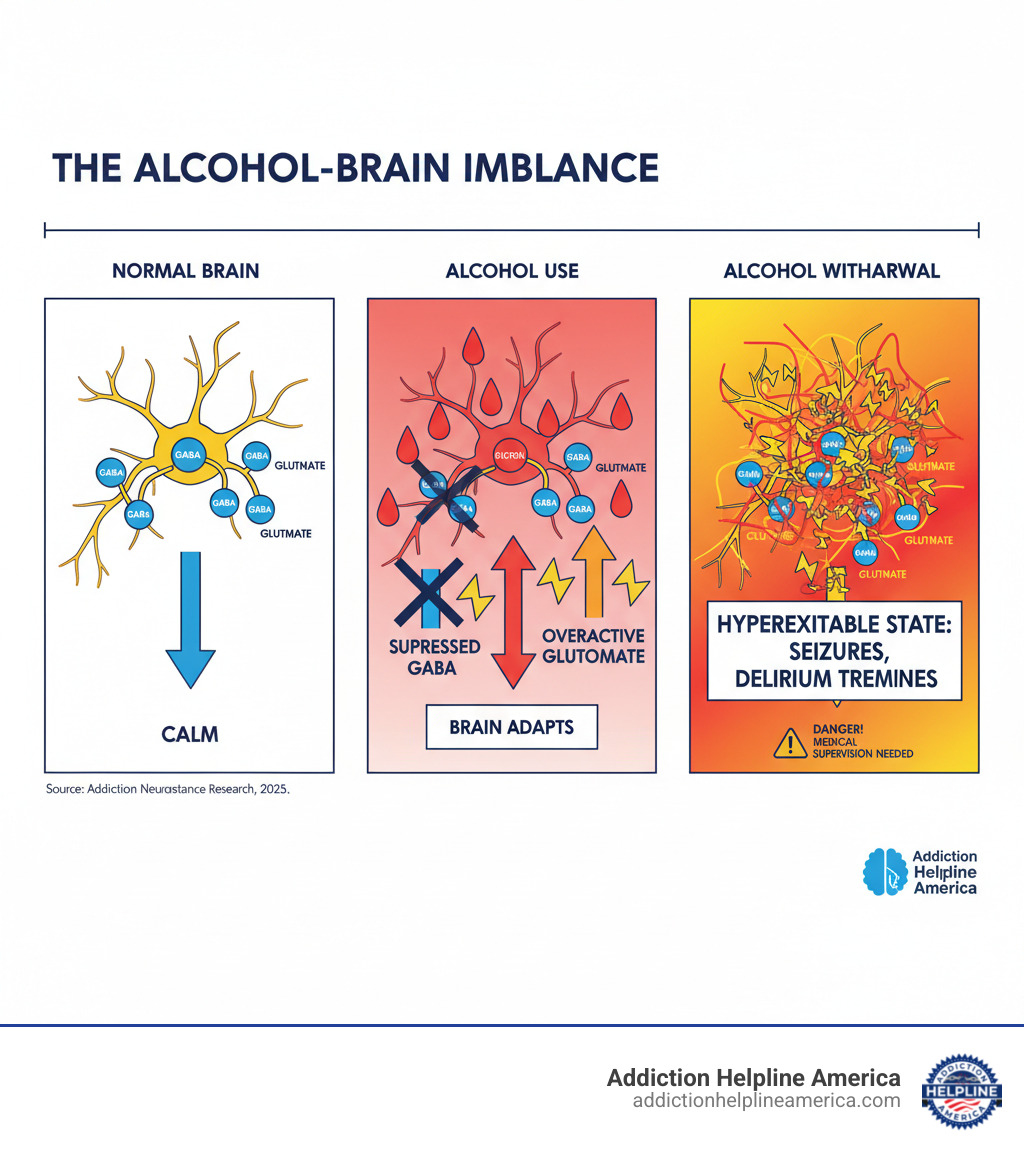
This happens because alcohol is a depressant. Your brain compensates by producing more excitatory chemicals. When alcohol is removed, the brain is left in a hyperexcitable state. At Addiction Helpline America, we understand the severity of alcohol withdrawal and connect people with the safe, supervised medical detox needed to save lives.
Simple alcohol withdrawal word guide:
Understanding Alcohol Withdrawal: Causes and Symptoms
Understanding the science behind alcohol withdrawal and its warning signs could save a life.
What Causes Alcohol Withdrawal?
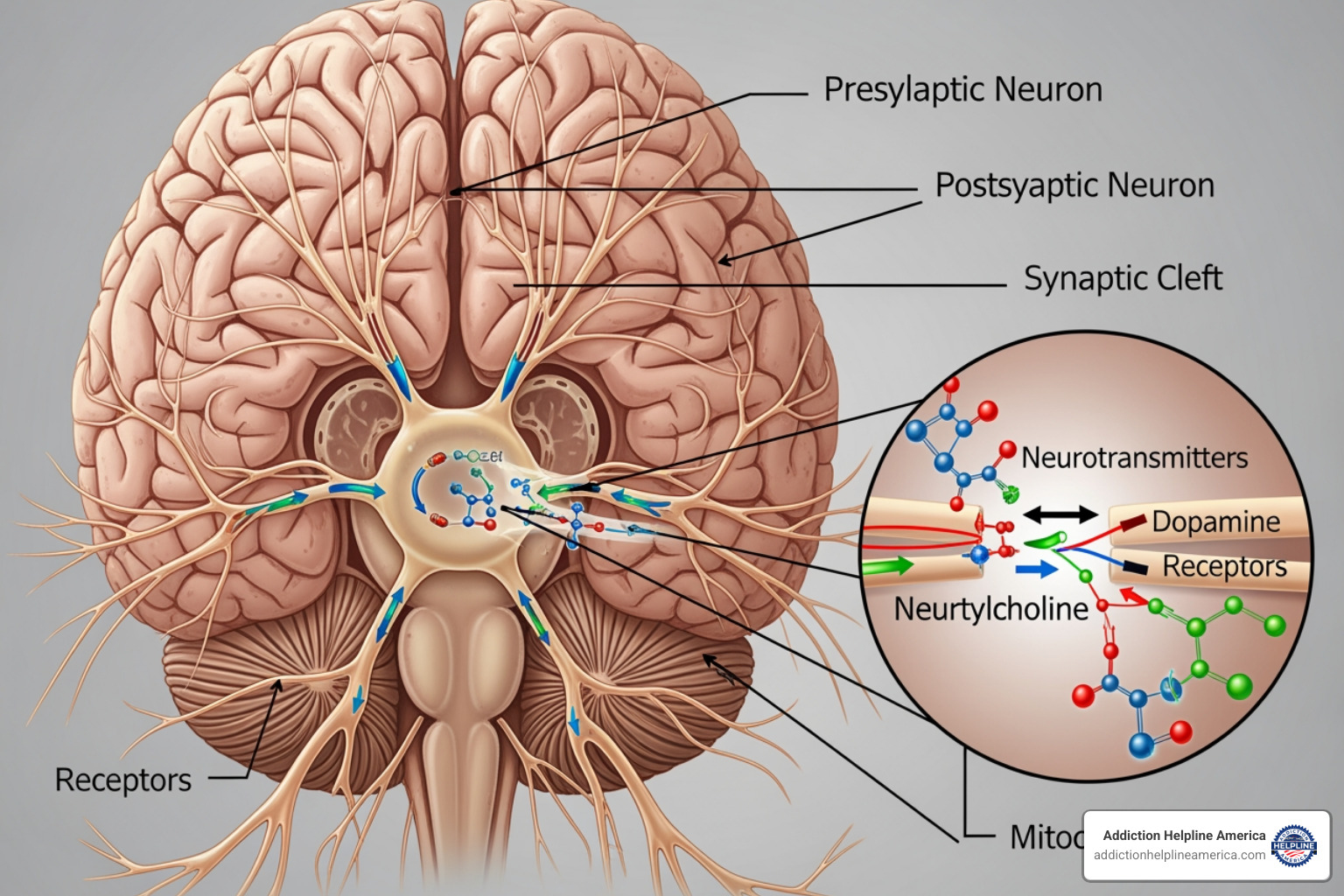
Think of your brain as constantly balancing itself. Alcohol is a central nervous system (CNS) depressant. Over time, your brain adapts to its presence. It reduces the activity of its main “calm down” chemical (GABA) and ramps up its main “accelerator” chemical (glutamate) to maintain normal function.
When you suddenly stop drinking, this balance is thrown off. The brakes (GABA) are weak, but the accelerator (glutamate) is floored. This creates a dangerous hyperexcitable state, sending your nervous system into overdrive. As detailed in studies on the neurobiology of alcohol withdrawal, this is a physical medical condition, not a failure of willpower.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Common Symptoms of Alcohol Withdrawal
Symptoms range from uncomfortable to life-threatening. The severity varies, but even mild symptoms can escalate quickly.
Early symptoms often appear first and feel like a severe hangover that doesn’t improve:
- Anxiety or nervousness
- Insomnia, despite exhaustion
- Nausea, vomiting, and headaches
- Heart palpitations (racing or pounding heart)
- Excessive sweating
- Tremors (“the shakes”), especially in the hands
These are warning signs that require medical attention.
Severe symptoms indicate a medical emergency:
- Hallucinations (visual, auditory, or tactile)
- Seizures, which can occur without any prior history
- Profound confusion and disorientation
- Severe agitation
- Significantly high blood pressure, rapid heart rate, and high body temperature
It’s impossible to predict if mild symptoms will become severe, which is why medical supervision is essential from the start.
Risk Factors for Severe Complications
Certain factors increase your risk for life-threatening complications:
- A history of previous withdrawals: The “kindling effect” means each withdrawal can be more severe than the last.
- Heavy, long-term drinking: The more your brain has adapted to alcohol, the more intense the rebound effect will be.
- Co-occurring medical conditions: Liver disease, heart conditions, or infections reduce your body’s ability to handle the stress of withdrawal.
- Nutritional deficiencies: Low levels of thiamine (vitamin B1), folate, and magnesium are common and can worsen neurological symptoms, increasing the risk of Wernicke-Korsakoff syndrome.
- Older age: Age-related health changes make withdrawal more dangerous.
- Concurrent substance use: Using other substances, especially sedatives, makes withdrawal unpredictable.
While about 50% of people with alcohol use disorder experience withdrawal, around 5% develop delirium tremens (DTs). The mortality rate for untreated severe withdrawal can be as high as 15%. With medical care, it drops to 1-5%. These statistics underscore why medical supervision is not optional—it’s life-saving.
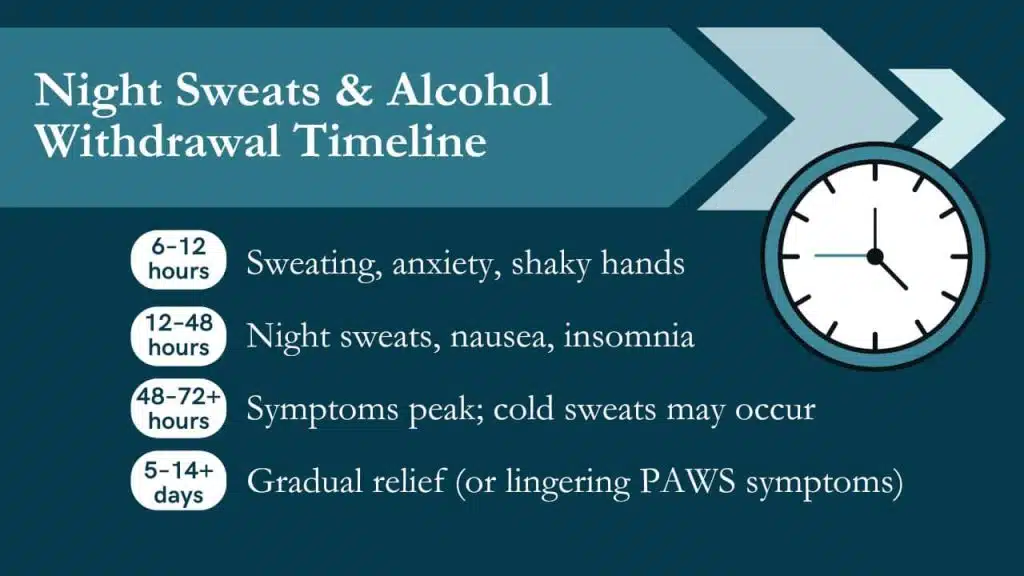
The Timeline and Stages of Alcohol Withdrawal
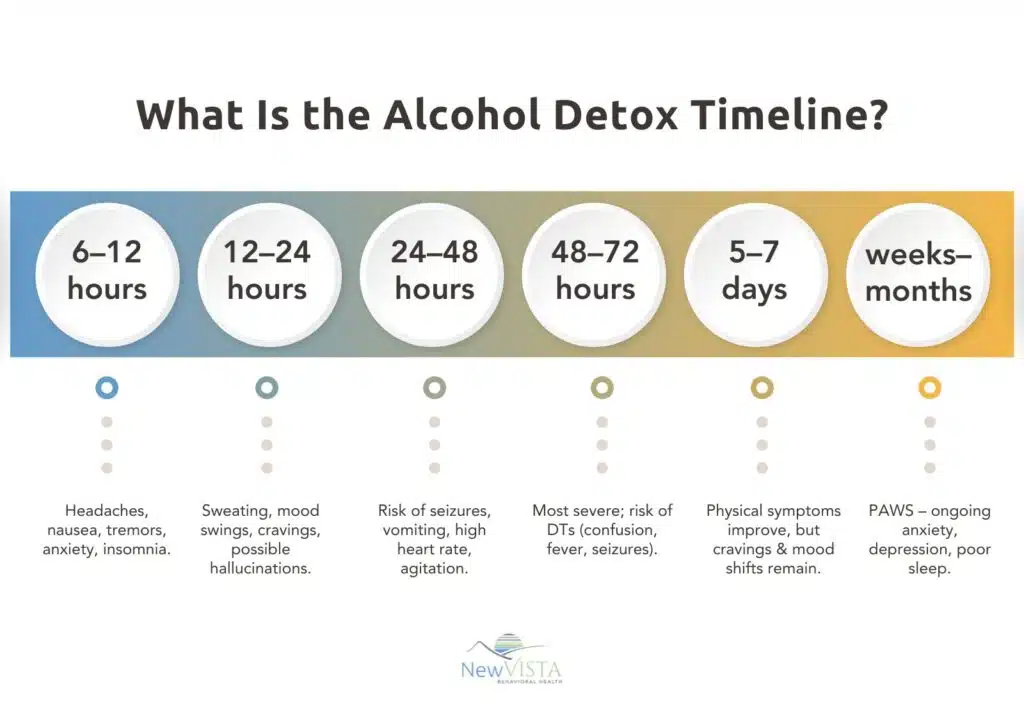
Alcohol withdrawal symptoms follow a general timeline, though each person’s experience is unique. Symptoms usually start within 8 hours of the last drink and peak between 24 to 72 hours, the most dangerous period. Your personal timeline depends on your drinking history, health, and genetics.
Stage 1: Early Withdrawal (6-12 Hours)
The first signs often appear within 6-12 hours and can feel like a severe hangover. You may experience:
- Mild anxiety
- Headaches
- Insomnia
- Nausea or vomiting
- Heart palpitations
- Sweating
- Tremors (“the shakes”)
Even if these symptoms seem manageable, they can escalate quickly. This is the time to seek medical help.
Stage 2: Peak Symptoms & Hallucinations (12-48 Hours)
Between 12 and 48 hours, withdrawal intensifies as the brain’s chemical imbalance peaks. Symptoms can become frightening and dangerous.
- Increased blood pressure and heart rate
- Confusion and disorientation
- Alcoholic hallucinosis: Seeing, hearing, or feeling things that aren’t there. Typically, you remain aware that the hallucinations aren’t real.
The greatest danger in this stage is seizures, with the risk peaking at 24-48 hours. These are a medical emergency and a key reason why medical supervision is critical.
Stage 3: Delirium Tremens (DTs) (48-72+ Hours)
Delirium tremens is the most severe form of alcohol withdrawal, affecting about 5-20% of people in detox. DTs are a medical emergency that usually appears 48-72 hours after the last drink but can occur up to 10 days later.
Symptoms of DTs are severe and require immediate hospitalization, often in an ICU:
- Severe disorientation and confusion
- Extreme agitation
- High fever and soaking sweats
- Wildly fluctuating blood pressure and heart rate
- Severe, full-body tremors
- Vivid and persistent hallucinations
As detailed in studies on the Recognition and management of delirium tremens, this condition can be fatal due to dangerous shifts in breathing, circulation, and temperature. The mortality rate is 1-5% even with treatment. With proper medical care, acute symptoms usually improve within 5-7 days, though some effects can linger for weeks or months.
Diagnosis and Medical Treatment Options

Proper medical assessment during alcohol withdrawal is life-saving. Here’s how professionals diagnose and treat the condition.
How is Alcohol Withdrawal Diagnosed?
Diagnosis involves a comprehensive evaluation:
- Physical Exam: Checking vital signs (heart rate, blood pressure, temperature) and looking for physical signs like tremors or sweating.
- Medical and Alcohol Use History: An honest discussion about your drinking patterns and any previous withdrawal experiences is crucial for your safety.
- Symptom Assessment: Healthcare providers use the Clinical Institute Withdrawal Assessment for Alcohol, Revised (CIWA-Ar) scale to score the severity of ten common symptoms. This score guides treatment decisions. You can learn more about it at CIWA-Ar for Alcohol Withdrawal.
- Blood Tests: These check for electrolyte imbalances, assess liver and kidney function, and identify nutritional deficiencies (especially thiamine). They also help rule out other conditions with similar symptoms.
Treatment for Mild to Moderate Withdrawal
If withdrawal is assessed as mild to moderate and you have a strong support system, outpatient treatment may be an option, but medical supervision is always recommended. The goals are to manage discomfort, prevent complications, and prepare you for long-term recovery.
- Supportive Care: A calm, quiet environment is provided, with regular monitoring of vital signs.
- Hydration and Nutrition: Fluids and nutritious food help your body heal from the effects of chronic alcohol use.
- Vitamin Supplementation: Thiamine (Vitamin B1) and folic acid are standard to prevent serious neurological complications like Wernicke-Korsakoff syndrome. Electrolytes like magnesium are also replenished.
- Medications: Benzodiazepines (e.g., diazepam, lorazepam) are the primary treatment. They calm the nervous system, reduce anxiety, and prevent seizures. They are given in tapering doses. Anticonvulsants like gabapentin may also be used.
Treating Severe Alcohol Withdrawal and DTs
Severe alcohol withdrawal and delirium tremens (DTs) are medical emergencies requiring hospitalization.
- Hospitalization: Treatment in an Intensive Care Unit (ICU) is standard for severe cases.
- Continuous Monitoring: Vital signs, oxygen levels, and mental status are watched closely to respond immediately to complications.
- Medications: Benzodiazepines are given intravenously (IV) in higher, symptom-triggered doses to control severe agitation and prevent seizures. Phenobarbital, a powerful sedative, may be used if benzodiazepines are not effective enough.
- Supportive Medications: Beta-blockers may be used to control high blood pressure and heart rate.
- Intravenous Fluids: IV fluids correct dehydration and electrolyte imbalances.
With prompt, aggressive medical treatment, the mortality rate for DTs is 1-5%. Without it, the rate is much higher. This is why professional medical care is essential.
Life After Detox: Prevention and Long-Term Recovery

Medical detox is a critical first step, but it’s the beginning of recovery, not the end. The real work is building a life free from alcohol. At Addiction Helpline America, we guide people through this transition.
Preventing Future Relapse
After detox, how do you stay sober? Complete abstinence from alcohol is the only way to prevent future alcohol withdrawal. This requires more than willpower, as Alcohol Use Disorder (AUD) is a complex disease.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Ongoing support and treatment are essential. Relapse prevention involves:
- Identifying personal triggers (people, places, emotions) that create the urge to drink.
- Developing healthy coping mechanisms for stress, anxiety, and other difficult emotions.
- Building a strong support network.
A comprehensive aftercare plan—including therapy, support groups, or sober living—is your roadmap. While only about 20% of people with AUD maintain long-term abstinence without formal support, your chances improve dramatically with a structured plan.
Post-Acute & Protracted Withdrawal
Even after acute withdrawal ends, your brain is still healing. Many people experience Post-Acute Withdrawal Syndrome (PAWS), which can last for weeks or months. These symptoms are more psychological than physical:
- Unpredictable mood swings
- Anhedonia (inability to feel pleasure)
- Sleep problems (insomnia or exhaustion)
- Cognitive issues like poor concentration or memory
Research shows protracted alcohol withdrawal can persist for a year or more in some people. Understanding that PAWS is a normal and temporary part of brain recalibration can help you persevere without relapsing.
Finding Support for Lasting Sobriety
Recovery is not a solo journey. Surrounding yourself with support is key to success.
- Psychotherapy: Cognitive Behavioral Therapy (CBT) helps change thought patterns that lead to drinking.
- Family Counseling: This helps repair relationships and teaches loved ones how to support your recovery.
- Peer Support Groups: Connect with others who understand. Options include Alcoholics Anonymous, the science-based SMART Recovery, and Al-Anon for families.
National organizations like the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and SAMHSA also offer valuable information and resources. Recovery is about progress, not perfection. You’ve already shown strength by completing detox; now, let’s build on that foundation.
Frequently Asked Questions about Alcohol Withdrawal
When facing alcohol withdrawal, you have urgent questions. Here are straightforward answers to the most common concerns.
How much do I have to drink to experience withdrawal?
There is no single answer, as withdrawal risk is highly individual. It typically develops after weeks or months of heavy drinking. The NIAAA defines heavy drinking as five or more drinks a day (or 15+ per week) for men, and four or more a day (or 8+ per week) for women. However, some people can develop withdrawal at lower consumption levels.
Your personal risk depends on:
- Drinking pattern: How long and how much you’ve been drinking.
- Genetics and body chemistry: A family history of alcohol use disorder can increase susceptibility.
- Overall health: Co-occurring medical conditions, nutritional status, and age are all factors.
- Previous withdrawals: Due to the “kindling” effect, each withdrawal episode can be more severe than the last.
If you are drinking regularly and are concerned about withdrawal, that is reason enough to seek medical advice before stopping.
Can you die from alcohol withdrawal?
Yes, alcohol withdrawal can be fatal. This is not to scare you, but to stress the importance of medical supervision. Severe withdrawal, especially delirium tremens (DTs), is a medical emergency that can cause life-threatening complications:
- Seizures: Uncontrolled seizures can lead to respiratory arrest or brain damage.
- Cardiovascular Collapse: Dangerous fluctuations in heart rate and blood pressure can cause a heart attack or stroke.
- Hyperthermia: An extremely high body temperature can damage vital organs.
- Electrolyte Imbalances: These can trigger fatal heart rhythm abnormalities.
The mortality rate for DTs is 1-5% even with medical care. For those with severe symptoms who do not get treatment, the rate can be as high as 15%. Seeking immediate medical help for alcohol withdrawal is not just a good idea—it can save your life.
How long does alcohol withdrawal last?
The timeline varies, but a general pattern exists.
- Onset: Symptoms typically begin 6 to 24 hours after the last drink.
- Peak Danger: The most dangerous period is 24 to 72 hours after stopping, when the risk of seizures and DTs is highest.
- Acute Phase: For most people, the most severe physical symptoms improve within 5 to 7 days.
- Protracted Withdrawal: Some symptoms can linger for weeks or months. This is known as Post-Acute Withdrawal Syndrome (PAWS) and can include mood swings, anxiety, sleep problems, and cognitive difficulties. These symptoms often come and go in waves as your brain continues to heal, sometimes for a year or more.
The duration and intensity depend on your drinking history, health, and whether you receive medical treatment. This is why ongoing support is so important. At Addiction Helpline America, we help you find the right support for every stage of your journey.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Your Path to a Safe and Sober Future
You now understand a critical fact: alcohol withdrawal is a serious medical emergency that demands professional care. This isn’t about “toughing it out.” When your body has adapted to alcohol, stopping suddenly can trigger a dangerous, and sometimes fatal, cascade of reactions.
Safe, medically supervised detoxification is the essential first step toward recovery. It’s the foundation for building a sober life. Without it, the journey can be cut tragically short.
We know reaching out for help is overwhelming. You may worry about judgment or not know where to start. At Addiction Helpline America, we provide free, confidential, and personalized guidance. We connect you to the right recovery program from our vast network of treatment centers across all 50 states and the District of Columbia.
Long-term sobriety is achievable with the right support. Detox is just the beginning; the therapy, support groups, and rebuilding of your life are where real change happens. You don’t have to do it alone.
Taking the first step is an act of immense strength. Don’t face alcohol withdrawal by yourself. Your path to a healthier, sober future starts with one conversation.
Find help now through our addiction and rehab hotlines
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















