
Understanding What Happens After Treatment Ends
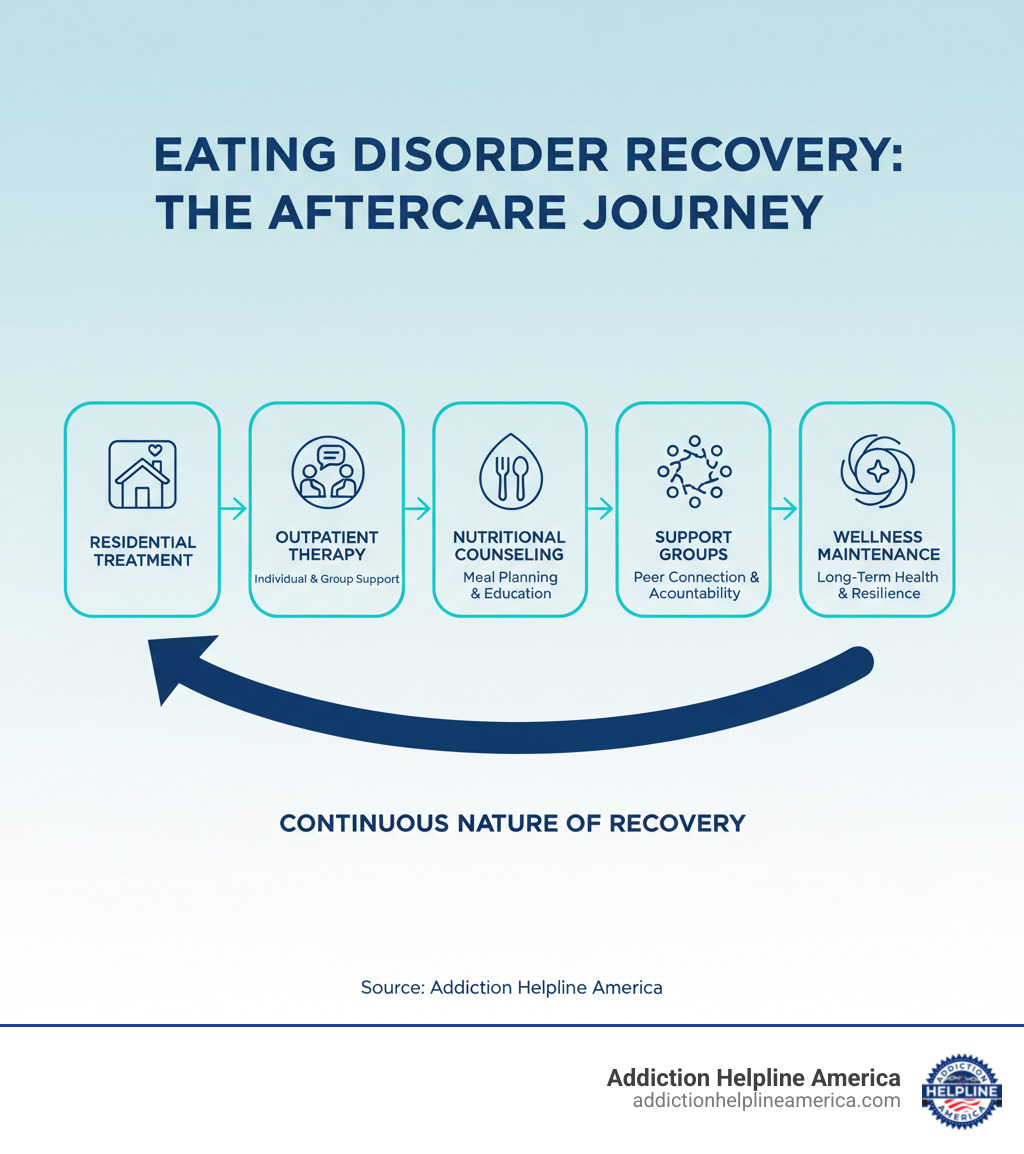
Aftercare for eating disorders is the crucial, ongoing support that begins after completing a formal treatment program. It’s designed to help you maintain recovery, prevent relapse, and build a fulfilling life beyond the eating disorder.
What aftercare typically includes:
- Continued therapy with an eating disorder specialist
- Nutritional counseling with a registered dietitian
- Medical monitoring for physical health concerns
- Support groups (in-person or online)
- A personalized crisis plan for managing triggers
- Regular check-ins with your treatment team
Completing treatment is a huge achievement, but the journey continues. The transition from a structured, 24/7 supportive environment to independent living can be overwhelming. An effective aftercare plan acts as a roadmap, helping you steer real-world triggers and stressors to build a resilient, fulfilling life.
At Addiction Helpline America, we’ve guided countless individuals and families through the complexities of eating disorder recovery, connecting them with vital aftercare resources and support networks. Our team understands that aftercare for eating disorders isn’t just a checklist—it’s a compassionate, ongoing commitment to your wellness.
Why Aftercare is Crucial for Lasting Recovery
Finishing intensive treatment is a victory, but it’s the beginning of your recovery journey, not the end. Aftercare for eating disorders is the essential bridge from the structured support of treatment to the complexities of independent living.
Studies show that aftercare reduces relapse episodes and improves long-term outcomes. People who engage in aftercare services—like therapy or support groups—fare significantly better than those who don’t. Recovery is hard work, and life’s stressors can trigger old patterns. A solid aftercare plan helps you build resilience and apply the coping skills you learned in real-world situations, turning fragile progress into lasting strength.
The Transition from a Structured Environment
Leaving the 24/7 support of residential treatment is a major shift. You’re suddenly responsible for planning meals, navigating triggering environments, and managing daily life without a built-in support system. Feelings of anxiety, loneliness, and being overwhelmed are normal. An aftercare for eating disorders plan provides guidance and accountability during this rocky transition period.
Understanding Relapse as Part of the Process
Recovery is rarely a straight line. The National Eating Disorders Association makes this clear—slips and relapses are common. It’s helpful to distinguish a lapse (a temporary slip) from a relapse (a return to sustained disordered patterns). Neither is a sign of failure.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
A good aftercare for eating disorders plan prepares you for these moments. It treats them as learning opportunities, helping you identify triggers and strengthen your support system without shame or guilt. The goal is progress and resilience, not perfection.
Key Components of an Effective Aftercare Plan for Eating Disorders

An effective aftercare for eating disorders plan is a personal, evolving roadmap you create with your treatment team. It’s a tool for self-empowerment that helps you proactively prepare for challenges. Successful plans include professional support, a strong community, practical coping strategies, and a vision for a fulfilling life in recovery.
Continued Professional Support
Continued professional support is the backbone of effective aftercare for eating disorders. Your team may include:
- A Therapist: For ongoing sessions (using CBT, DBT, etc.) to process challenges and apply skills learned in treatment.
- A Registered Dietitian: To help you rebuild a healthy relationship with food, create flexible meal plans, and steer challenging eating situations.
- A Medical Doctor: For regular check-ups to monitor physical health and address any lingering complications.
- A Psychiatrist: To manage medications for co-occurring conditions like depression or anxiety.
Addiction Helpline America can help you find qualified providers, or you can use national directories to locate mental health services in your area.
Building Your Core Support System
You can’t do this alone. Your core support system is your safety net.
- Identify Key People: Pinpoint supportive parents, partners, or friends who are non-judgmental and committed to your recovery.
- Involve Family: Family therapy can help loved ones understand how to support you effectively and improve communication.
- Connect with Mentors: Individuals further along in recovery can offer invaluable guidance and hope.
- Set Boundaries: It’s crucial to limit contact with people who are critical or unsupportive of your recovery. This is an act of self-respect.
- Ask for Help: Learning to ask for support is a skill. It’s not a burden to others; it’s a gift to let them be part of your healing.
Integrating Positive Coping Skills and Managing Triggers
Aftercare is about putting the coping skills you learned into daily practice.
- Healthy Coping Skills: Use tools like mindfulness, journaling, deep breathing, joyful movement, and creative expression to manage stress and difficult emotions without turning to disordered behaviors. Grounding techniques (like the 5-4-3-2-1 method) can quickly pull you back to the present.
- Identify and Manage Triggers: Know your personal triggers—the situations, emotions, or people that make you vulnerable. Develop proactive strategies to manage them, such as having a pre-planned response or calling a support person.
- Challenge Negative Self-Talk: When the inner critic appears, use the therapeutic techniques you learned to challenge it and remember your inherent worth.
Developing a Balanced Lifestyle for Long-Term Recovery
Recovery is about building a life so meaningful that the eating disorder has no room.
- Establish Routines: Consistent sleep, meal, and self-care schedules reduce anxiety.
- Plan Meals: Work with your dietitian to create flexible, sustainable meal plans that ensure regular nourishment.
- Practice Self-Care: Prioritize adequate sleep, rest, and activities that bring you joy.
- Find Hobbies and Purpose: Reconnect with old interests or find new ones to build an identity separate from the eating disorder. Pursue education, meaningful work, or volunteering.
- Set Achievable Goals: Small recovery-related or personal goals build momentum and confidence. Each success reminds you that you are moving forward.
Navigating Support Systems and Community in Recovery

A powerful realization in recovery is that you are not alone. Connecting with others who have similar experiences is profoundly healing and a core part of aftercare for eating disorders. A supportive community reduces isolation, fosters connection, provides accountability, and offers hope. It transforms recovery from a lonely battle into a shared journey.
The Role of Support Groups in Aftercare for Eating Disorders
Support groups offer something unique: the lived experience of peers. This peer support validates your struggles and provides practical tools.
- In-person groups offer face-to-face connection and a strong sense of community accountability.
- Online communities provide accessibility and anonymity, which can encourage more honest sharing. Research shows that internet and mobile-based aftercare are just as successful as face-to-face support.
The key is finding a good fit. Try different groups to see where you feel most comfortable and supported.
How to Find and Engage with Recovery-Focused Communities
Finding your community is easier than you might think.
At Addiction Helpline America, we work with a vast network of treatment centers and support organizations. We can connect you with resources for your aftercare for eating disorders journey, whether you’re in Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, Virginia, Washington, West Virginia, Wisconsin, Wyoming, or the District of Columbia.
Other resources include:
- Alumni programs from your treatment center.
- National organizations like NEDA and ANAD, which have directories of support groups.
- Local community mental health centers or hospitals.
- Moderated social media groups focused on recovery (use with caution and leave any group that feels harmful).
Preparing for Crises and Maintaining Accountability
Even with a strong aftercare for eating disorders plan, you’ll face tough days. The difference between a setback and a relapse often comes down to preparation. Proactively planning for difficult moments and building in accountability gives you a safety net for your recovery journey.
Creating a ‘911’ Plan for Moments of Crisis
A crisis plan is a smart, protective tool for when you feel overwhelmed or are experiencing intense urges.
- Identify Your Warning Signs: Work with your therapist to recognize the psychological (obsessive thoughts), behavioral (skipping meals, isolating), and social (withdrawing) signs that you’re heading toward a crisis.
- Create a Contact List: Have a list of people to call immediately, including your therapist, dietitian, a trusted friend, and a sponsor. Keep the 988 Suicide and Crisis Lifeline number handy (call or text 988). For life-threatening emergencies, always call 911.
- List Soothing Activities: Create a go-to list of healthy coping skills you can use in the moment, such as listening to a calming playlist, taking a walk, or practicing deep breathing exercises. This helps interrupt the spiral of disordered thinking.
Strategies for Maintaining Accountability in Aftercare for Eating Disorders
Accountability is the daily practice of showing up for yourself. It’s about consistency, not punishment.
- Regular Check-ins: Treat appointments with your therapist, dietitian, and doctor as non-negotiable commitments.
- Recovery Apps: Use mobile apps for meal tracking (if recommended), mood monitoring, or connecting with online support.
- Journaling: Document your thoughts, feelings, and meals to maintain self-awareness and identify patterns for your treatment team.
- Support Groups: Consistent attendance creates accountability through community.
- Review and Adjust: Life changes, and so should your plan. Regularly review your aftercare for eating disorders plan with your support team to assess what’s working and what needs to be adjusted.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Frequently Asked Questions about Eating Disorder Aftercare
We understand that navigating aftercare for eating disorders can bring up many questions. Here are some honest answers to common concerns.
What are the most common warning signs of an eating disorder relapse?
Early warning signs are your internal alarm system. Look for:
- Psychological signs: A return of obsessive thoughts about food or weight, increased anxiety or depression, and tying self-worth to the scale.
- Behavioral signs: Skipping meals, eating alone, returning to food rituals, hiding behaviors from your support team, excessive exercise, or frequent weighing.
- Social signs: Withdrawing from friends and family or avoiding social events involving food.
The National Eating Disorders Association emphasizes that recognizing these signs early is key. If you notice them, reach out for support immediately.
How long does recovery from an eating disorder take?
There is no simple answer or set timeline. Recovery is a process, not a destination, and it looks different for everyone. For some, it takes months; for others, it takes years. Research shows that it’s a long process and setbacks are common, especially during times of stress. The key is to focus on progress, not perfection. Your aftercare for eating disorders plan is there to support you for as long as you need it.
Is full recovery from an eating disorder possible?
Yes, full recovery is absolutely possible. It doesn’t mean you’ll never think about food or your body, but that disordered thoughts and behaviors no longer dominate your life. Research on measuring recovery defines it as achieving physical, behavioral, and psychological health. It’s about building a life where you are free to be yourself, separate from the eating disorder identity. With a strong aftercare for eating disorders plan and consistent effort, a rich, fulfilling life is within reach.
Your Path Forward in Recovery
Choosing to learn about aftercare for eating disorders is an important step in your recovery. This journey is an ongoing commitment to yourself, and it’s one you don’t have to take alone. While recovery can feel isolating, there are people and resources ready to walk alongside you.
At Addiction Helpline America, we believe in your resilience. Our mission is to provide free, confidential guidance, connecting you to the right aftercare resources from our extensive network across the United States. We’re here to help you strengthen your plan and find the support you need.
Every small step forward is a victory. Lean on your support system, use your coping skills, and remember why you started. A life of wellness, peace, and joy is not just a dream—it’s an achievable reality. Your story is just beginning, and the person you’re becoming is worth fighting for.
Get your complete guide to addiction recovery
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















