Limited Availability: Treatment beds filling quickly. Call now for immediate placement – (844) 561-0606
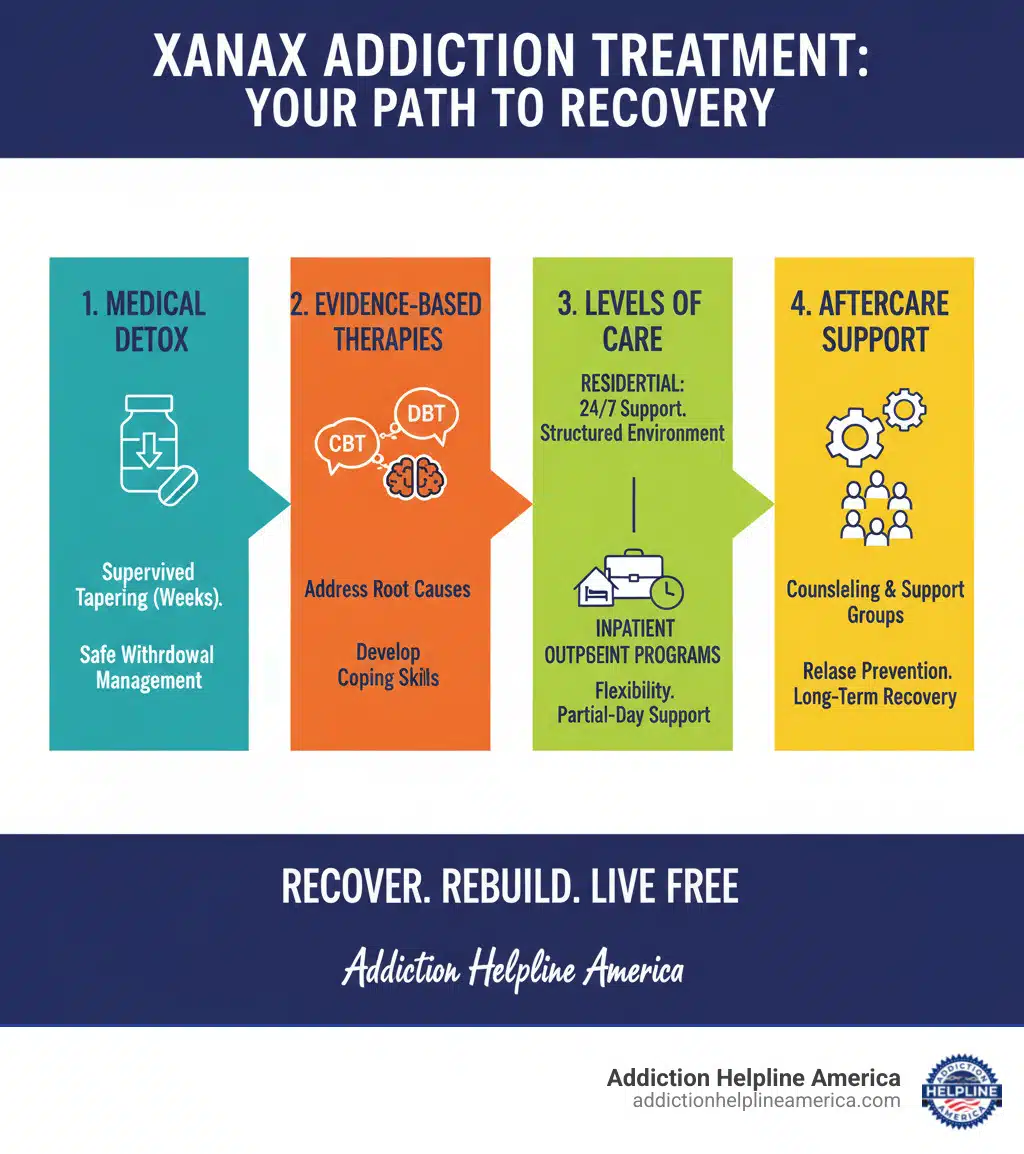
Xanax Addiction Treatment is a structured process to help individuals safely stop using alprazolam and rebuild their lives. Here’s a quick overview:
Xanax (alprazolam) is a commonly prescribed benzodiazepine for anxiety, but it carries a high risk of addiction. In 2020, over 3.4 million people aged 12+ misused alprazolam. The statistics are sobering: overdose deaths involving benzodiazepines have skyrocketed, often due to mixing them with opioids.
But there is hope. Xanax addiction is treatable, and recovery is possible with professional care. This guide will walk you through the signs of addiction, detox, therapy, and long-term recovery strategies.
At Addiction Helpline America, we connect people with the evidence-based care needed to overcome substance abuse. Our specialists provide 24/7 support and treatment referrals, making the process of seeking help as clear and supportive as possible.
Xanax (alprazolam) is a benzodiazepine prescribed for anxiety and panic disorders. It works by enhancing the effects of GABA, a brain chemical that produces a calming effect. This makes it a fast-acting and effective CNS depressant.
Doctors prescribe Xanax for short-term use because its rapid onset and short half-life contribute to a high potential for misuse. The quick relief it provides can be highly reinforcing.
How misuse and addiction develop often begins with a legitimate prescription. Over time, the body develops tolerance, requiring higher doses to achieve the same effect. This can lead to taking more than prescribed, which quickly escalates to physical dependence. When physically dependent, the body needs the drug to function normally, and stopping causes severe withdrawal symptoms like anxiety, insomnia, tremors, and seizures.
It’s important to distinguish between physical dependence and addiction. Dependence is the body’s physiological adaptation. Addiction is a chronic brain disease characterized by compulsive drug-seeking and use despite harmful consequences. It involves a powerful psychological dependence, where you feel unable to cope without the drug.
Several factors increase the risk of addiction. Genetic risk factors account for 40-60% of a person’s vulnerability. Environmental risk factors like trauma, stress, peer pressure, and co-occurring mental health disorders (anxiety, depression, PTSD) also play a significant role. Regular Xanax use alters brain chemistry, making it extremely difficult to quit without professional Xanax Addiction Treatment.
Recognizing the signs of addiction is the first step toward getting help. The DSM-5 uses specific criteria to diagnose a sedative use disorder. Key signs fall into physical, behavioral, and psychological categories.
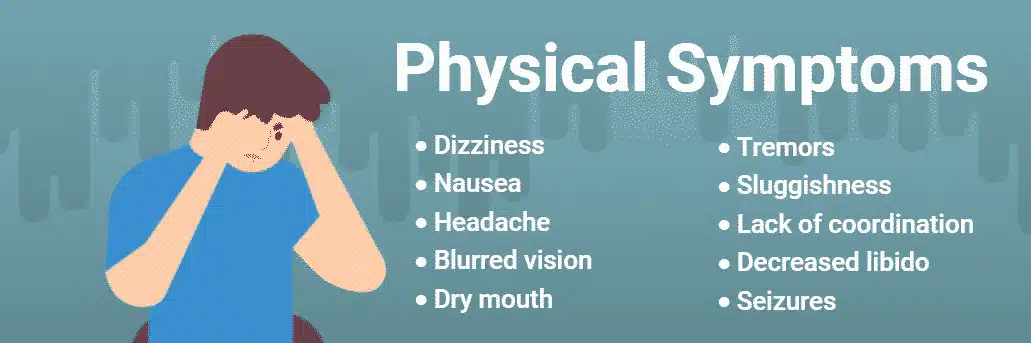
Physical signs include:
Behavioral changes may involve:
Psychological symptoms can manifest as:
If you notice several of these signs, it’s time to seek professional guidance.
The risks of Xanax misuse are severe and can be life-threatening.
Overdose risk is a primary concern, especially when mixing Xanax with other CNS depressants like alcohol or opioids. This combination can cause respiratory depression, where breathing slows to a fatal stop. Data shows that over 92% of deaths involving benzodiazepines also involved opioids. You can learn more about the risks of combining benzodiazepines and opioids from NIDA.
An even greater threat comes from counterfeit pills. Illicitly purchased Xanax is often contaminated with fentanyl, a synthetic opioid 50 times stronger than heroin. The DEA found that 6 out of 10 fake pills contained a potentially lethal dose of fentanyl in 2022. These pills look identical to real Xanax, making every dose a deadly gamble.
Long-term cognitive effects from chronic misuse include significant memory problems, confusion, and difficulty concentrating. Some research suggests a link between long-term benzodiazepine use and an increased risk of dementia. The drug’s sedative effects also dramatically increase the risk of accidents, such as falls and car crashes.
Finally, co-occurring mental health concerns are common. Addiction often exists alongside anxiety, depression, PTSD, and other disorders. Effective Xanax Addiction Treatment must address both the substance use and any underlying mental health conditions for recovery to be successful.
Overcoming Xanax addiction is possible with a professional, individualized treatment plan. At Addiction Helpline America, we use a continuum of care, adapting our approach to your unique situation. The process begins with a thorough assessment to understand your addiction severity, mental health, and personal history, which forms the foundation of your recovery plan.
Professional support is non-negotiable. Quitting Xanax alone is dangerous due to life-threatening withdrawal symptoms. Professional treatment provides medical safety, therapeutic tools, and the support needed for lasting recovery. You can explore treatment options through our network to find what’s right for you.
Medically supervised detox is essential for safely managing Xanax withdrawal.

Why medical detox is essential: Suddenly stopping Xanax can cause a dangerous surge in brain activity. This rebound effect can lead to severe and potentially fatal withdrawal symptoms, including seizures and delirium tremens. Other symptoms include intense anxiety, insomnia, tremors, and hallucinations. The short half-life of Xanax means withdrawal can begin quickly, which is why Xanax withdrawal can be severe.
In a professional detox setting, a medical team uses tapering protocols, gradually reducing your dose over weeks or months to minimize withdrawal risks. You receive 24/7 medical monitoring and medications to manage symptoms and ensure your safety and comfort. The acute withdrawal phase typically lasts 5 to 28 days, and professional support makes this period manageable.
After detox, therapy addresses the root causes of addiction. Combining psychological support with medical care is far more effective than tapering alone. Key behavioral therapies include:
Your plan may also include individual counseling and medications like SSRIs to manage co-occurring anxiety or depression.
The right level of care depends on your addiction severity, mental health, and home environment.
Inpatient residential rehab offers 24/7 structured care in a drug-free facility. It’s ideal for severe addiction or co-occurring disorders, as it removes you from daily triggers and allows for total immersion in recovery. Programs typically last 30, 60, or 90 days.
Outpatient programs provide flexibility, allowing you to live at home while attending treatment. They are suitable for milder addiction or for those with strong support systems. Options include:
Here’s a quick comparison:
| Feature | Inpatient/Residential Rehab | Outpatient Programs |
|---|---|---|
| Intensity | High—24/7 supervised care | Moderate to low—regular sessions, return home daily |
| Environment | Live at facility in a controlled, drug-free setting | Live at home, attend sessions at a facility |
| Cost | Generally higher | Generally lower |
| Ideal Candidate | Severe addiction, unstable home, co-occurring disorders | Mild to moderate addiction, strong support, work/family needs |
| Medical Support | Constant medical and psychiatric oversight | Regular medical check-ups (less intensive) |
| Duration | Typically 30, 60, or 90+ days | Varies from a few hours per week to several hours per day |

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
The right duration depends on your needs, and you can learn more about program lengths at How Long is Rehab?. Our specialists at Addiction Helpline America can help you determine the best level of care for your situation.
Completing a Xanax Addiction Treatment program is a major achievement, but recovery is a lifelong process. Think of addiction as a chronic condition that requires ongoing management. Aftercare and relapse prevention are the tools you’ll use to maintain sobriety and build a fulfilling life.
Ongoing support is critical, as relapse is a common part of the recovery journey for many. A solid aftercare plan dramatically reduces this risk. At Addiction Helpline America, we help you create a personalized strategy. You can explore our resources on Aftercare and Relapse Prevention to learn more.
Key components of a strong aftercare plan include:
Prioritizing a healthy lifestyle through exercise, nutrition, and quality sleep also builds resilience. Recovery is about progress, not perfection. By using these tools and reaching out for support, you can build a meaningful life free from addiction.
Taking the first step toward Xanax Addiction Treatment is a courageous act, and you don’t have to do it alone. Addiction Helpline America is here to guide you through the process.

Recognizing the need for help is the first hurdle. If you’re worried that Xanax is controlling your life, it’s time to talk to someone you trust—a friend, family member, or doctor. If you’re concerned about a loved one, approach them with compassion, using “I” statements to express your worry without judgment.
When you’re ready to explore options, finding a treatment center can be straightforward. Your doctor is a good starting point, or you can use the national SAMHSA Treatment Locator.
For immediate, confidential support, addiction hotlines are an invaluable resource. Our team at Addiction and Rehab Hotlines is available 24/7. A specialist will listen to your story, answer your questions, and help you understand your options—all for free and with no obligation.
Many people worry about cost, but verifying insurance coverage often reveals that treatment is more accessible than you think. The Affordable Care Act requires most plans to cover substance abuse treatment, and many private, Medicaid, and Medicare plans offer coverage as well. Our team can help you understand your benefits and find a program that fits your financial situation. Learn more about your options here: Will My Insurance Cover Drug Rehab?.
At Addiction Helpline America, our mission is to connect you with the right help. We offer free, confidential, and personalized guidance, matching you with a treatment center from our nationwide network that fits your unique needs. Whether you need information or are ready to start treatment, we’re here for you. Contact us to learn about rehabilitation services and take the first step toward recovery.
The path through Xanax addiction is difficult, but it’s a journey you don’t have to take alone. Xanax addiction is a treatable condition, and with the right support, recovery is entirely possible.
Effective treatment follows a clear path: it begins with medically supervised detox for safety, moves into evidence-based therapies like CBT and DBT to address root causes, and offers different levels of care to fit your life. Recovery is sustained through ongoing aftercare and relapse prevention, including support groups and continued therapy.
The prognosis for recovery is positive, comparable to that of other chronic diseases like diabetes or hypertension, as noted by research on addiction treatment outcomes. With sustained effort, long-term recovery is within reach.
If you are ready to take the first step, we are here to help. At Addiction Helpline America, our specialists provide free, confidential guidance 24/7. We will help you understand your options, verify insurance, and connect you with a treatment program custom to your needs.
Hope and healing are waiting. Contact us to learn about rehabilitation services and begin your journey to wellness today.
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.
For anyone seeking help for addiction for themselves or a loved one calls to Addiction Helpline America are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 561-0606. You may also contact us for further assistance.
Calls to any general helpline will be answered or returned by one of the treatment providers listed, each of which is a paid advertiser:
Our helpline is available 24 hours a day, 7 days a week at no cost to you and with no obligation for you to enter into treatment. We are committed to providing support and guidance whenever you need it.
In some cases, Addiction Helpline America charges our verified partner a modest cost per call. This fee helps us cover the costs of building and maintaining our website, ensuring that we can continue to offer this valuable service to those in need.
Identifying the signs of Xanax addiction is crucial for early intervention and treatment. Common indicators include increased tolerance, withdrawal symptoms when not using, and behavioral changes such as neglecting responsibilities or engaging in "doctor shopping" for prescriptions. Understanding these signs can help individuals and their loved ones recognize when professional help is needed.
Physical signs may manifest as persistent drowsiness, slurred speech, or coordination issues, while psychological symptoms can include mood swings, confusion, and heightened anxiety when not using the drug. If you or someone you know exhibits several of these signs, seeking help from a professional can be the first step towards recovery.
Mixing Xanax with other substances, particularly opioids or alcohol, significantly increases the risk of overdose and other serious health complications. This dangerous combination can lead to respiratory depression, unconsciousness, and even death, making it imperative to understand the dangers involved.
Statistics show that overdose deaths involving benzodiazepines like Xanax have surged, often linked to polydrug use. Awareness of these risks is essential for individuals using Xanax and their families, emphasizing the importance of adhering to prescribed dosages and avoiding the use of other depressants.
The detox process for Xanax addiction is a critical step in recovery, designed to safely manage withdrawal symptoms under medical supervision. During this phase, healthcare professionals may implement tapering protocols to gradually reduce dosage, minimizing the risk of severe withdrawal reactions such as seizures and intense anxiety.
Detox typically occurs in a controlled environment where patients receive constant medical support. This structured approach not only ensures safety but also prepares individuals for the subsequent stages of treatment, focusing on the psychological aspects of addiction and the development of coping strategies.
Evidence-based therapies play a vital role in treating Xanax addiction, focusing on addressing the root causes of substance use. Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) are two approaches commonly used to help individuals develop healthier thought patterns and coping mechanisms that reduce the likelihood of relapse.
Research indicates that these therapies can significantly improve treatment outcomes by equipping individuals with the skills needed to manage cravings and stressors effectively. Additionally, incorporating family therapy and group counseling can foster a supportive environment, further enhancing the recovery journey.