Understanding Addiction: What You Need to Know
Addiction is a chronic brain disorder characterized by compulsive substance use or behavior despite harmful consequences. It changes brain function, especially in areas of reward, decision-making, and self-control. Key features include:
- Compulsive behavior – An overwhelming urge to use or engage in behaviors, even when wanting to stop.
- Loss of control – Inability to limit use despite negative effects on life.
- Brain changes – Altered chemistry driving cravings and withdrawal.
- Chronic condition – Requires ongoing management, like diabetes or heart disease.
- Treatable disease – Recovery is possible with proper support.
According to the 2023 National Survey on Drug Use and Health, 48.7 million Americans aged 12 or older had a substance use disorder in the past year. The American Society of Addiction Medicine defines addiction as a primary, chronic disease of brain reward, motivation, and memory. This isn’t a moral failing; repeated substance use rewires the brain, flooding it with dopamine and impairing the prefrontal cortex, which governs judgment and impulse control. This makes stopping without professional help extremely difficult.
At Addiction Helpline America, our specialists, counselors, and advocates help individuals and families steer the complex journey of addiction recovery with compassion and evidence-based support.

Learn more about addiction:
Understanding the Nature of Addiction
Addiction is a complex brain disorder, not a bad habit. It rewires how you think and behave, creating intense, persistent cravings for a substance or behavior despite serious harm to your health, relationships, or life. We approach addiction as a chronic medical condition requiring comprehensive treatment, not judgment.
Defining Addiction: More Than Just a Habit
Clinical addiction, or Substance Use Disorder (SUD), involves compulsively seeking and using a substance despite devastating consequences. The American Psychiatric Association’s DSM-5 outlines criteria for diagnosis, which include:
- Impaired control: Using more than intended, trying unsuccessfully to cut back, spending excessive time on the substance, and experiencing intense cravings.
- Social impairment: Failing to meet responsibilities at work, school, or home; giving up hobbies; and continuing use despite relationship problems.
- Risky use: Using in dangerous situations (like driving) or despite worsening physical or mental health.
- Pharmacological criteria: Developing tolerance and experiencing withdrawal.
These criteria show that addiction is driven by actual changes in brain structure and function, a medical reality detailed in scientific research on drug addiction symptoms.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Types of Addiction: Substance vs. Behavioral
Addiction falls into two main categories:
Substance Use Disorders involve the compulsive use of brain-altering drugs or alcohol.
- Alcohol: The most common substance addiction in the U.S., damaging the brain, liver, and heart.
- Opioids: Prescription painkillers (oxycodone, fentanyl) and heroin carry a high risk of overdose and death.
- Nicotine: Highly addictive, with e-cigarettes becoming a major concern for youth since 2014.
- Stimulants: Cocaine, methamphetamine, and prescription drugs like Adderall create an intense, highly addictive rush.
- Cannabis: Can lead to addiction and dependence despite common misconceptions.
- Sedatives, hypnotics, and anxiolytics: Prescription drugs like Xanax and Valium can be dangerously addictive.
Behavioral addictions involve compulsive activities. The DSM-5 officially recognizes gambling disorder, which is linked to severe outcomes like suicide attempts. Other problematic behaviors include internet gaming (recognized by the WHO in its ICD-11), compulsive shopping, excessive social media use, and problematic sexual behavior, all of which can disrupt daily life.
The Roles of Tolerance and Withdrawal
Tolerance and withdrawal are two forces that trap people in addiction.
Tolerance develops as your body adapts to a substance, requiring you to use more to get the same effect. Your brain chemistry changes to maintain balance, diminishing the substance’s impact over time.
Withdrawal occurs when you stop or reduce use. Symptoms can be psychological (anxiety, depression, anhedonia—the inability to feel pleasure) and physical (nausea, tremors, seizures). To avoid the misery of withdrawal, many people continue using, shifting from seeking pleasure to simply avoiding pain. This cycle of tolerance and withdrawal makes addiction feel inescapable.
Long-Term Consequences
Untreated addiction has devastating, far-reaching consequences. At Addiction Helpline America, we connect people with help to avoid these outcomes:
- Physical Health: Chronic use can lead to liver cirrhosis (alcohol), heart damage (stimulants), lung disease (smoking), infectious diseases like HIV/hepatitis (injection drug use), and cognitive impairment.
- Mental Health: Addiction often co-occurs with or worsens depression, anxiety, and psychosis. Suicide risk increases significantly.
- Relationships: Trust erodes, families are torn apart, and isolation deepens, making recovery harder.
- Financial & Legal Problems: The cost of addiction leads to debt, job loss, and often illegal activities, resulting in arrests and incarceration.
- Overdose: The most tragic risk. In 2023, over 107,000 Americans died from drug-involved overdoses.
These consequences are not inevitable. With treatment, recovery is possible.
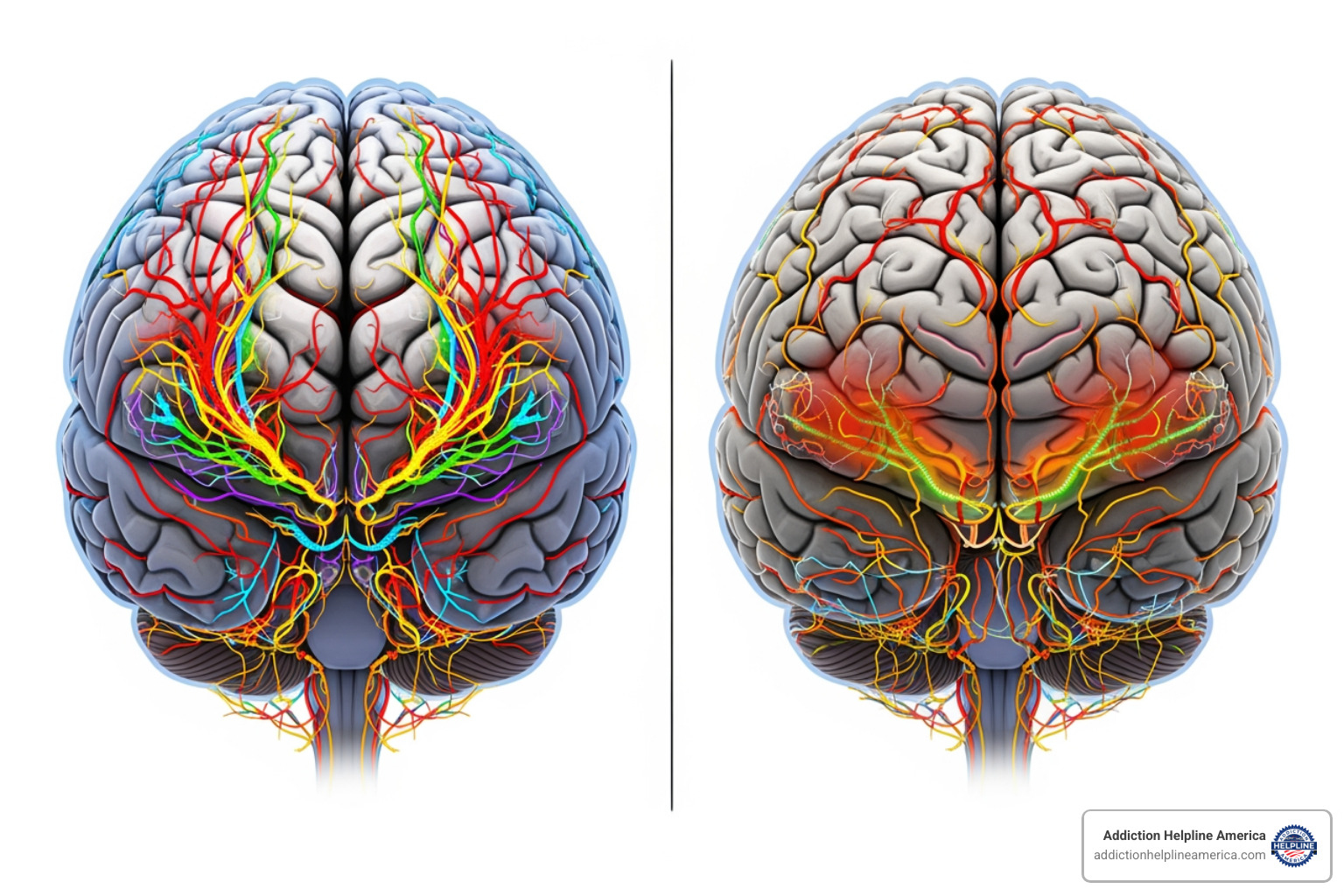
The Science Behind Why Addiction Develops
Addiction develops because substances and certain behaviors hijack the brain’s essential reward system. This system uses the chemical messenger dopamine to motivate survival behaviors like eating and socializing, creating feelings of pleasure. Addictive substances overwhelm this system with dopamine surges two to ten times greater than natural rewards, creating an intense “high.”
How Addiction Hijacks the Brain
When faced with repeated dopamine floods, the brain tries to adapt by reducing its dopamine receptors or natural dopamine production. This process, called desensitization, means everyday pleasures no longer feel rewarding. The person needs the substance just to feel normal.
At the same time, the brain’s learning systems create powerful associations, turning people, places, or situations into triggers that spark intense cravings. Most importantly, the prefrontal cortex—the brain’s center for judgment and impulse control—becomes impaired. This is why someone with addiction continues using despite knowing the harm; the brain’s “brakes” aren’t working properly.
A protein called ΔFosB (DeltaFosB) accumulates with repeated substance use, acting as a molecular switch that causes long-lasting changes in neural pathways, driving compulsive behavior. As the NIDA’s science of addiction guide explains, these changes can persist for years. Addiction rewires the brain through neuroplasticity, teaching it to prioritize the substance above all else.
Key Risk Factors
Not everyone who tries a substance becomes addicted. Risk is determined by a mix of factors:
- Genetics: Account for about 40-60% of a person’s risk for addiction. A family history significantly increases vulnerability. Epigenetics, or how environment affects gene expression, also plays a role.
- Environment: Factors like peer pressure, chaotic home life, abuse, or neglect (Adverse Childhood Experiences or ACEs) increase risk.
- Trauma: Many people with addiction have a history of significant trauma, which is a major risk factor.
- Early Age of First Use: Using substances before age 18 dramatically increases the likelihood of developing addiction, as it disrupts the development of the adolescent brain. Over 90% of people with addiction started using before they were 18.
Co-Occurring Disorders and Dual Diagnosis
About half of people with a mental health condition also experience a Substance Use Disorder, and vice versa. This overlap is called co-occurring disorders or dual diagnosis.
Many people use substances to cope with untreated mental health issues like depression, anxiety, PTSD, or bipolar disorder—a pattern known as the self-medication hypothesis. While substances may offer temporary relief, they ultimately worsen the underlying condition and create addiction.
Conversely, chronic substance use can trigger or intensify mental health problems. Because these conditions are so intertwined, effective treatment must address both simultaneously. This integrated approach is supported by organizations like the Substance Abuse and Mental Health Services Administration (SAMHSA), which provides extensive information on co-occurring disorders.
At Addiction Helpline America, we help you find treatment that addresses all your needs, as this is the key to lasting recovery.
Pathways to Recovery: Effective Treatment for Addiction
Here’s the truth that gives us hope every single day at Addiction Helpline America: addiction is a treatable disease, and recovery is absolutely possible. Millions of Americans have successfully overcome addiction and gone on to live fulfilling lives. We believe in an individualized approach to care because each person’s journey to recovery is unique.

Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Principles of Effective Addiction Treatment
The National Institute on Drug Abuse (NIDA) has identified several principles for effective treatment:
- Treatment must be individualized, as no single approach works for everyone.
- Care should be readily available because when someone is ready for help, timing is critical.
- Effective treatment addresses the whole person, not just their substance use, including medical, psychological, social, and legal problems.
- Staying in treatment long enough is crucial for positive outcomes.
- Behavioral therapies and counseling are the cornerstones of treatment.
- Medications are an important element, especially when combined with therapy.
- Treatment plans must be regularly assessed and modified to meet a person’s changing needs.
- Co-occurring mental health disorders must be treated concurrently with addiction.
- Medically assisted detoxification is only the first stage of treatment, not a cure.
The Role of Behavioral Therapies
Behavioral therapies are where you learn to change the patterns that drive addiction.
- Cognitive-Behavioral Therapy (CBT) helps you identify and change negative thought patterns and behaviors related to substance use, teaching practical coping skills.
- Motivational Interviewing (MI) is a collaborative approach where a therapist helps you resolve ambivalence and find your own internal motivation for change.
- Contingency Management (CM) uses positive reinforcement, like vouchers or prizes, to reward abstinence and treatment participation.
- Family Therapy involves loved ones in the healing process to improve communication and build a supportive home environment. Programs like Al-Anon and Nar-Anon, related to Alcoholics Anonymous and Narcotics Anonymous, offer support for families.
- Support Groups and 12-Step programs like AA and NA provide powerful peer support and a structured path to recovery within a community of people with shared experiences.
Medication-Assisted Treatment (MAT)
MAT combines FDA-approved medications with behavioral therapies to treat substance use disorders, particularly for opioid and alcohol addictions. It is not “replacing one addiction with another,” but is a medically supervised approach to stabilize brain chemistry and support recovery.
- For opioid use disorder, medications like methadone and buprenorphine (Suboxone) reduce cravings and withdrawal symptoms, while naltrexone (Vivitrol) blocks the euphoric effects of opioids to prevent relapse.
- For alcohol use disorder, naltrexone reduces cravings, acamprosate helps with long-term withdrawal symptoms, and disulfiram (Antabuse) creates an unpleasant reaction to alcohol, acting as a deterrent.
- For nicotine addiction, Nicotine Replacement Therapy (NRT) (patches, gum) and medications like bupropion (Zyban) reduce cravings and withdrawal.
MAT addresses both the physical and psychological aspects of addiction, significantly improving the chances of lasting recovery. For more detailed information, we offer a guide on What is Medication-Assisted Treatment?.
Frequently Asked Questions about Addiction
We hear these questions every day at Addiction Helpline America. If you’re wondering about these things, you’re not alone—and asking questions is a powerful first step toward understanding.
What is the difference between substance use disorder and intoxication?
Intoxication is a temporary state caused by a substance’s immediate effects on your brain and body. It fades as the substance leaves your system.
Substance Use Disorder (SUD), or addiction, is a chronic disease defined by a compulsive pattern of use, intense cravings, and continued use despite negative consequences. You can be intoxicated without having an SUD, and a person with an SUD is not always intoxicated, but they are always living with the disease. The distinction is crucial: intoxication is temporary, while SUD is a persistent medical condition requiring treatment.
Is addiction a choice or a disease?
Science confirms that addiction is a disease, not a choice. While the initial decision to use a substance is voluntary, repeated use fundamentally rewires the brain. It hijacks the reward system and impairs the prefrontal cortex, which controls judgment and impulse control.
These brain changes are not a choice. They create a powerful compulsion that makes it incredibly difficult to stop, even for someone who desperately wants to. Like other chronic diseases such as diabetes, addiction requires professional treatment and ongoing management. This medical perspective removes the shame that often prevents people from seeking help, while still emphasizing the personal responsibility required for recovery.
Can addiction be cured?
Addiction is a chronic disease, which means it is typically managed, not “cured” in the way an infection is. Instead of a cure, the goal is remission and long-term recovery. With effective treatment and ongoing effort, people can and do manage the disease so effectively that it no longer controls their lives.
Recovery is a lifelong process. Relapse, or returning to substance use, is common and does not mean treatment has failed. Relapse rates for addiction (40-60%) are similar to those for other chronic illnesses like diabetes or hypertension. A relapse is a sign that the treatment plan may need to be adjusted. The key is to learn from it and continue with a strong support system and ongoing care.
At Addiction Helpline America, we’ve seen countless individuals move from active addiction to thriving in recovery. Seeking help is a sign of courage and strength, not weakness.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Conclusion
If you’ve made it this far, you now understand something profound: addiction isn’t about weakness or moral failure. It’s a chronic brain disease, but recovery is absolutely possible.
It is a treatable medical condition. Every day, people break free from the grip of addiction, rebuild their lives, and find happiness. The science is clear: with the right support and evidence-based treatment, millions of Americans have found their way back to health.
We know that taking the first step can feel overwhelming. You might be scared, ashamed, or uncertain, but seeking help is one of the bravest things you can do. It’s a choice to fight for yourself and a life free from the constant cycle of cravings, use, and consequences.
At Addiction Helpline America, we’ve dedicated ourselves to walking alongside individuals and families on this journey. Our team offers free, confidential support to connect you with personalized treatment options from our trusted network. There is no judgment, only compassionate guidance.
You don’t have to figure this out alone. Whether you’re ready to start treatment today or just need someone to talk to about your options, we’re here. Recovery begins with a single phone call—a decision that can change everything.
Find personalized addiction treatment options today
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















