The Allure of a “Quick Fix” for Opioid Withdrawal
Ultra rapid detox is a controversial medical procedure that promises to eliminate opioid withdrawal symptoms in just hours by using general anesthesia and opioid antagonists to force rapid detoxification. However, medical evidence shows it carries serious risks. A 2013 Centers for Disease Control and Prevention (CDC) report on one UROD program identified a fatality rate over 2% and a total serious adverse event rate of over 9%. Furthermore, studies have shown it is no more effective at preventing relapse than traditional methods, with major medical organizations advising against its use.
Key Facts About Ultra Rapid Detox:
- What it is: A 4-8 hour procedure using general anesthesia while opioid antagonists (like naltrexone or naloxone) force withdrawal, as described in medical literature reviewed by the National Center for Biotechnology Information (NCBI).
- Claimed benefit: Bypassing conscious withdrawal pain.
- Reality: High risk of death, heart attack, pulmonary edema, and aspiration pneumonia, with the CDC reporting serious adverse events in multiple patients.
- Effectiveness: Not proven more effective than traditional detox methods, with studies in journals like JAMA finding no advantage in long-term outcomes.
- Cost: $15,000-$21,000+ out-of-pocket (rarely covered by insurance), with costs reported by government sources and news outlets.
- Medical consensus: Considered experimental and potentially dangerous. The American Society of Addiction Medicine (ASAM), the UK’s National Institute for Health and Clinical Excellence (NICE), and the NYS OASAS Medical Advisory Panel all advise against its routine use.
- Safer alternative: Medically supervised detox using FDA-approved medications like buprenorphine or methadone.
When you’re desperate to escape the grip of opioid withdrawal, the idea of sleeping through the worst of it sounds incredibly appealing. The fear of withdrawal symptoms keeps many people trapped in addiction cycles, making promises of painless, rapid detoxification seem like a miracle solution. But the controversy surrounding ultra rapid detox runs deep, with mounting evidence that this “quick fix” may create more dangers than it solves.
At Addiction Helpline America, we’ve guided countless individuals through the complex landscape of opioid addiction treatment, including helping them evaluate ultra rapid detox against safer, evidence-based alternatives. Our team connects people with vetted treatment programs that prioritize both safety and long-term recovery success.
Quick ultra rapid detox definitions:
What is Ultra Rapid Detox and How Does It Claim to Work?
Ultra rapid detox (UROD), sometimes referred to as Anesthesia-Assisted Rapid Opioid Detoxification (AAROD) or 1-day opiate detoxification, is a method designed to accelerate the physical withdrawal process from opioids. The core idea is to bypass the excruciating pain and discomfort typically associated with opioid withdrawal by having the patient undergo this phase while under general anesthesia or heavy sedation. This process is detailed in clinical reviews, such as those published by Canada’s Drug and Health Technology Agency (CADTH).
The procedure primarily involves administering opioid antagonists, such as Naltrexone or Naloxone, intravenously. These medications work by rapidly binding to the opioid receptors in the brain, effectively “kicking off” any opioids that are currently attached. This sudden displacement forces the body into an immediate and intense withdrawal state. The proposed mechanism is that by being unconscious, the patient avoids the conscious experience of these severe withdrawal symptoms.
The goal is to achieve a faster physical detox timeline, often within a matter of hours, rather than the days or weeks it can take with traditional methods. Proponents suggest that once the patient wakes up, the worst of the physical withdrawal is over, and they can then more quickly transition to naltrexone therapy, a medication used to prevent relapse by blocking opioid effects. This rapid induction onto naltrexone maintenance is often touted as a significant benefit.
The setting for such a procedure is typically an Intensive Care Unit (ICU) due to the high-risk nature of general anesthesia and the intense physiological stress induced by precipitated withdrawal. We understand the desire for a quick solution, and for more information on comprehensive approaches to managing opioid dependence, you can explore our resources on opioid addiction solutions.
The UROD Procedure Explained
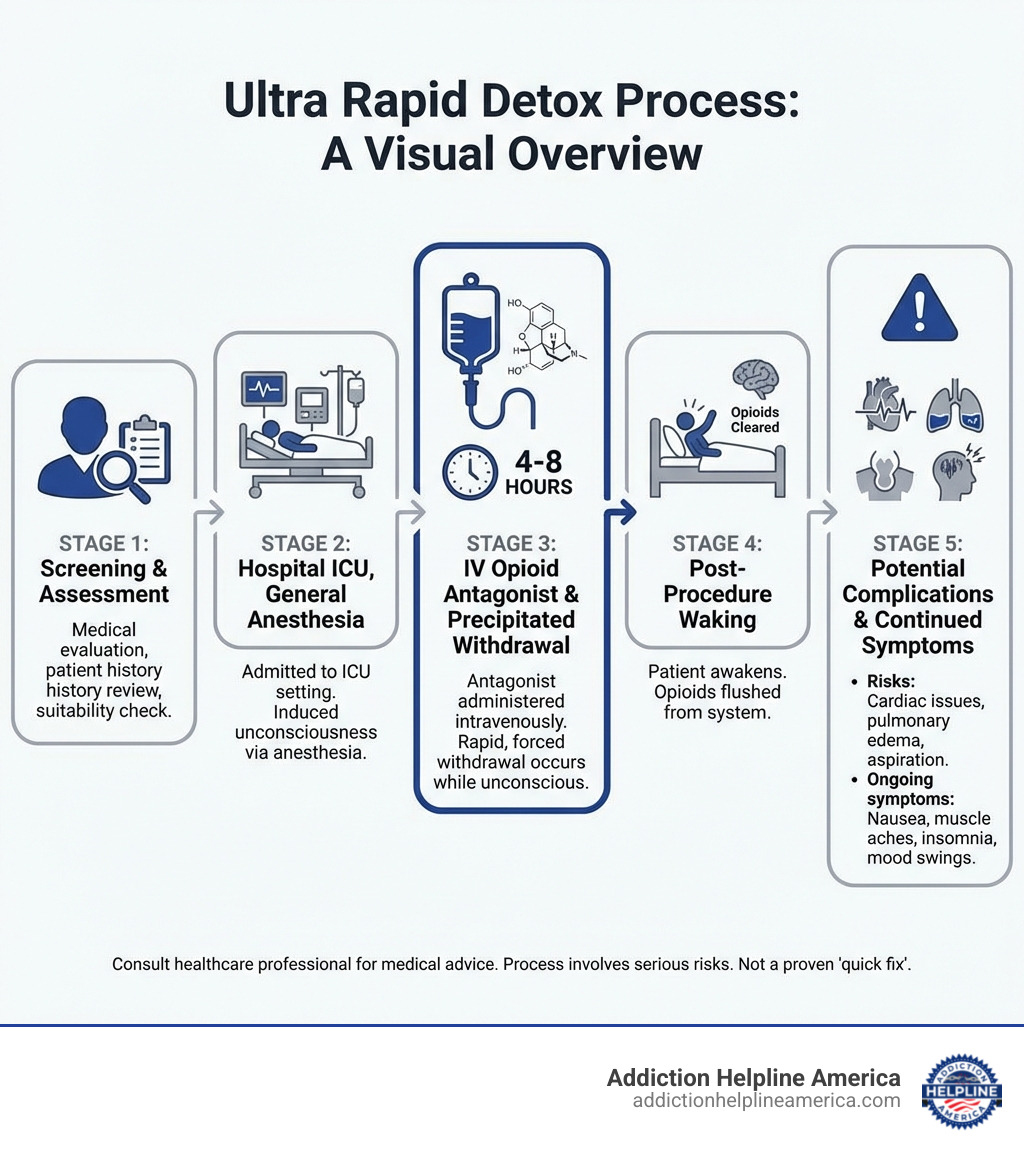
The process of ultra rapid detox is complex and medically intensive, often following a series of steps as outlined by medical guidelines and clinical reviews:
- Patient Screening: Before anything begins, thorough diagnostic criteria confirmation and laboratory testing are crucial. This includes ruling out contraindications such as active psychosis, suicidal ideation, or acute cocaine intoxication. A comprehensive medical and psychiatric evaluation is essential to determine suitability.
- Pre-procedure Preparation: If the patient is on a long-acting opioid like methadone, their addiction might first be transferred to a short-acting opioid (e.g., morphine or hydromorphone) to make the rapid detox more manageable. Patients may also receive a clonidine patch 12 hours prior to suppress sympathetic activity and aspiration prophylaxis (like an H2 receptor blocker) due to the risks of vomiting under anesthesia.
- Administration of General Anesthesia: The patient is placed under general anesthesia, meaning they are completely unconscious and often require mechanical ventilation to breathe. This is typically done in an ICU setting, allowing for constant, close medical supervision.
- Intravenous Opioid Antagonists: While the patient is unconscious, a bolus injection of a high dose of an opiate antagonist, usually naloxone, is administered intravenously. This is followed by a slow infusion of a lower dose. These antagonists work by rapidly forcing opioids off the brain’s receptors.
- Forcing Opioids Off Receptors: This action immediately triggers a rapid and intense opioid withdrawal syndrome, which the anesthesia is meant to mask from the patient’s conscious experience.
- Monitoring Vital Signs: Throughout the procedure, intensive monitoring is critical. This includes continuous EKG, pulse oximetry, blood pressure, core temperature, and urine output. Medical staff constantly watch for signs of excessive withdrawal, such as hypertension, tachycardia, or tachypnea, and manage them with medications like clonidine or beta-blockers.
- Duration of 4-8 hours: The active detoxification phase typically lasts between 4 to 8 hours.
- Post-procedure Observation: After the anesthesia wears off, patients usually require 1 to 2 days of hospitalization for continued observation and management of lingering symptoms.
What are the Proposed Benefits of Ultra Rapid Detox?
The primary allure of ultra rapid detox stems from its promise to circumvent the most feared aspects of opioid withdrawal. Proponents, often the clinics that provide the service, suggest several benefits:
- Reduced Discomfort: The main selling point is the idea that patients “sleep through” the worst of withdrawal, thus experiencing significantly less physical discomfort and psychological distress.
- Faster Physical Withdrawal: The process aims to compress the multi-day or multi-week withdrawal period into a matter of hours, allowing the body to rapidly clear opioids from its system.
- Bypassing the Most Intense Withdrawal Phase: By inducing withdrawal under anesthesia, the patient theoretically avoids the peak intensity of symptoms like severe muscle aches, nausea, vomiting, diarrhea, and extreme anxiety.
- A “Clean Slate” for Recovery: The rapid clearance of opioids is presented as a way to quickly get a patient to a “clean” state, ready to begin the next phase of treatment.
- Quicker Transition to Relapse-Prevention Medication: Because the body is rapidly detoxified, patients can supposedly begin naltrexone maintenance therapy (an opioid blocker) much sooner than with traditional detox methods, which require a period of opioid abstinence before naltrexone can be safely started.
While these proposed benefits sound incredibly appealing, especially to someone desperate for relief, it’s crucial to examine them against the scientific evidence and medical consensus, which we will do next.
The Evidence Uncovered: Major Safety Concerns and Efficacy Questions
Despite the enticing promises of a quick and painless escape from opioid dependence, the medical community has raised significant alarms regarding ultra rapid detox. The consensus among leading medical organizations is largely critical, highlighting a stark contrast between marketing claims and scientific reality. There is a profound lack of robust scientific support for its safety and long-term effectiveness, leading to serious ethical considerations, particularly around patient consent and the potentially misleading marketing of such a high-risk procedure. We believe that an informed decision is the best decision, and a critical look at the evidence is essential. For a broader perspective, you can refer to a review of UROD’s clinical effectiveness and safety guidelines.
Serious Risks and Reported Mortality
The most significant concerns surrounding ultra rapid detox revolve around its safety profile. Undergoing general anesthesia is never without risk, and when combined with the severe physiological stress of antagonist-precipitated opioid withdrawal, the dangers escalate dramatically.
Reported serious adverse events and risks include:
- General Anesthesia Risks: These are inherent to any procedure requiring deep sedation, including respiratory depression, allergic reactions, and complications related to intubation.
- Aspiration Pneumonia: A significant risk when patients vomit while under anesthesia, as stomach contents can enter the lungs.
- Pulmonary Edema: A dangerous condition where fluid accumulates in the lungs, making breathing difficult.
- Severe Metabolic Stress: The body undergoes profound stress as it’s forced into rapid withdrawal. This can lead to significant electrolyte imbalances, cardiac complications, and other systemic issues. The California Society of Addiction Medicine (CSAM) has noted concerns about profound epinephrine release and cardiovascular stimulation during AAROD.
- Cardiac Complications: The intense sympathetic nervous system response during precipitated withdrawal can lead to dangerous heart arrhythmias, increased blood pressure, and other cardiovascular events.
- Death: Tragically, there have been reported fatalities. A study highlighted by the Centers for Disease Control and Prevention (CDC) found that out of 75 patients undergoing rapid detox at one facility, two died and five others experienced life-threatening events. This represents a fatality rate over 2% and a serious complication rate of 9% for that cohort. Given that naturally occurring opioid withdrawal is rarely life-threatening, this statistic is particularly alarming.
We understand the urgency of seeking treatment for opioid dependence, and we strongly advocate for safe and effective options. If you or a loved one are struggling, please explore safe and proven paths to recovery, such as finding a safe heroin addiction treatment program.
Lingering Withdrawal Symptoms and High Relapse Rates
One of the most disheartening realities of ultra rapid detox is that the promise of a “painless” or “complete” withdrawal is often unfulfilled. Many patients still experience significant discomfort and symptoms even after the procedure:
- Post-procedure Withdrawal: While the most acute physical symptoms might be compressed, residual withdrawal symptoms are common. A landmark study published in JAMA found that anesthesia-assisted detox offered no overall benefit in withdrawal symptom severity compared to other methods.
- Insomnia and Muscle Pain: Patients frequently report difficulty sleeping for weeks after the procedure, along with persistent muscle aches and bone pain. This protracted abstinence syndrome can last anywhere from three to ten weeks, characterized by restlessness, irritability, and hypertension.
- Psychological Symptoms and Cravings: Crucially, ultra rapid detox does little to address the psychological components of addiction. Intense cravings, anxiety, depression, and other mental health challenges persist and are often exacerbated. The procedure does not provide the coping mechanisms or therapeutic support needed for long-term sobriety.
- High Relapse Rates: Perhaps the most damning evidence against ultra rapid detox is its poor long-term outcomes. Major studies have failed to show that UROD is any better at preventing relapse than safer, traditional methods. The 2005 JAMA study found no significant difference in the rates of relapse at 12 weeks between patients who underwent UROD and those who used other detox methods. Dr. Eric C. Collins, the study’s lead author, stated, “There was no advantage to the anesthesia-assisted procedure.”
- Increased Overdose Risk: Relapse after any form of detoxification is dangerous, but it’s particularly perilous after ultra rapid detox. The body’s tolerance to opioids is significantly lowered post-detox. If a person relapses and uses the same amount of opioids they did before detox, they are at a much higher risk of overdose, which can be fatal.
The idea that simply clearing the drug from the body cures addiction is a misconception. Addiction is a complex disease involving physical, psychological, and behavioral components that require a holistic and sustained treatment approach.
The Scientific Community’s View on Ultra Rapid Detox
The overwhelming consensus from reputable medical organizations and experts is that ultra rapid detox is not a recommended treatment for opioid use disorder. Their positions are clear and cautious:
- NYS OASAS Medical Advisory Panel: The New York State Office of Addiction Services and Supports (NYS OASAS) Medical Advisory Panel explicitly states that they “do not support ultra-rapid opiate detoxification as a safe and effective modality for the treatment of opiate dependence.” They emphasize the lack of documented long-term benefit and question the risk/benefit ratio. You can find their official statement on Ultra-rapid Opiate Detox.
- American Society of Addiction Medicine (ASAM): ASAM, a leading authority in addiction medicine, does not support the routine use of Anesthesia-Assisted Rapid Opioid Detoxification (AAROD). They recommend AAROD only under strict research conditions with careful informed consent and monitoring, until its safety and efficacy are proven and standardized. They stress that the benefits have not been shown to outweigh the added risks.
- Aetna’s Clinical Policy: Many insurance providers classify ultra rapid detox as “experimental, investigational, or unproven.” For example, Aetna’s clinical policy states that they consider ultra rapid detoxification (UROD) experimental, investigational, or unproven for all indications because its effectiveness has not been established and due to concerns about its safety. This classification means it’s generally not covered by insurance.
- Unacceptable Risk-to-Benefit Ratio: Experts consistently conclude that the significant risks associated with general anesthesia and precipitated withdrawal, coupled with the lack of proven long-term efficacy, create an unacceptable risk-to-benefit ratio for ultra rapid detox. Leading guidelines, such as those from the UK’s National Institute for Health and Clinical Excellence (NICE), have explicitly stated that ultra-rapid detoxification under general anesthesia or heavy sedation must not be offered due to the risk of serious adverse events, including death.
The scientific community views ultra rapid detox as a procedure that carries substantial risks without offering any demonstrated advantage over safer, evidence-based treatment methods in achieving long-term recovery.
The High Cost and Low Coverage of UROD
Beyond the critical safety and efficacy concerns, the financial aspect of ultra rapid detox presents another significant barrier and source of frustration for individuals and families seeking help. This procedure comes with a hefty price tag that is typically not covered by insurance.
- High Out-of-Pocket Costs: Ultra rapid detox is an extremely expensive procedure. On the low end, it may cost around $15,000, but well-established providers can charge significantly more, with some programs ranging upwards of $21,000+. A 2013 CDC report noted costs ranging up to $15,000, and prices have likely increased since. This substantial cost is almost always an out-of-pocket expense for the patient.
- Lack of Insurance Coverage: A major contributing factor to the high out-of-pocket cost is that most major health insurance companies will not pay for ultra rapid detox. As we’ve discussed, medical organizations and insurers like Aetna classify UROD as an “experimental, investigational, or unproven” treatment. Because it lacks established effectiveness and carries significant risks, it is not typically in the interest of insurance companies to cover it. You can review Aetna’s clinical policy on UROD for more details.
- Financial Burden on Patients and Families: This lack of coverage places an immense financial burden on individuals and their families, often at a time when they are already vulnerable and desperate for solutions. The substantial initial cost can also divert funds that would be better spent on comprehensive, long-term treatment, which is crucial for sustained recovery. The NYS OASAS Medical Advisory Panel has pointed out that the “substantial initial cost involved at a time of fiscal constraint could lead to inadequate funds being available for the critical ongoing treatment.”
We at Addiction Helpline America believe that financial considerations should not stand in the way of effective treatment. While we are a free and confidential service, we also help you understand payment options and connect you with programs that work with your insurance or offer financing, ensuring that proven, safe care is accessible.
Safer, Evidence-Based Alternatives to UROD
Given the significant risks, questionable efficacy, and high costs associated with ultra rapid detox, it’s crucial to understand that far safer and more effective evidence-based alternatives exist. We emphasize that detoxification, while an important first step, is rarely a standalone solution for opioid addiction. True recovery requires a commitment to comprehensive care, including long-term rehabilitation, therapy, counseling, and robust aftercare planning.
Medically Supervised Detox: The Gold Standard
Medically supervised detox, also known as medically assisted detox or medical detox, is widely considered the gold standard for safely and comfortably withdrawing from opioids. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), the goal of detox is to safely manage withdrawal symptoms and prepare a person for ongoing substance use disorder treatment. Unlike ultra rapid detox, it prioritizes patient safety and comfort through a gradual, managed process under the care of healthcare professionals.
Here’s how it compares:
| Feature | Ultra Rapid Detox (UROD) | Medically Supervised Detox |
|---|---|---|
| Safety | High risk of serious adverse events, including death, due to general anesthesia and severe precipitated withdrawal. | Low risk; symptoms are managed to avoid severe complications under medical supervision. |
| Efficacy | Not proven more effective than traditional methods; high relapse rates. | Proven effectiveness in managing withdrawal; higher likelihood of transitioning to long-term treatment. |
| Cost | Extremely high ($15,000-$21,000+ out-of-pocket). | Varies, but generally more affordable; often covered by insurance. |
| Insurance Coverage | Rarely covered; considered experimental. | Frequently covered by most major health insurance plans. |
| Long-Term Outcomes | Poor; not shown to improve relapse rates compared to other methods. | Better when followed by comprehensive treatment; addresses both physical and psychological aspects. |
In medically supervised detox, withdrawal symptoms are managed using specific medications to reduce discomfort and cravings. Common medications recommended by the National Institute on Drug Abuse (NIDA) include:
- Buprenorphine: A partial opioid agonist that can significantly reduce withdrawal symptoms and cravings without producing the same “high” as other opioids. It helps stabilize the patient.
- Methadone: A full opioid agonist used in a controlled environment to gradually taper the patient off opioids, managing withdrawal symptoms over a longer period. Methadone maintenance is a well-studied and effective long-term treatment for opioid addiction.
- Clonidine: An alpha-2 agonist that helps alleviate many of the physical symptoms of opioid withdrawal, such as anxiety, muscle aches, sweating, and cramping, by suppressing the overactive sympathetic nervous system.
The focus is on keeping the individual safe and as comfortable as possible while their body naturally clears the opioids. This approach allows for continuous assessment and adjustment of medication, ensuring a smoother transition into the next phase of recovery. To learn more about accessible and safe detox options, we invite you to explore our drug detox treatment centers guide.
The Role of Detox in Long-Term Recovery
It’s vital to reiterate a core principle of addiction treatment: detox is not a cure for addiction. While it’s a critical first step to safely remove substances from the body, it addresses only the physical dependence. Addiction is a chronic disease that affects the brain, behavior, and overall well-being. Therefore, successful long-term recovery necessitates addressing the root causes of addiction.
After detox, the real work of healing begins. This typically involves:
- Behavioral Therapies: Modalities like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Motivational Interviewing help individuals understand their addiction, identify triggers, and develop healthier coping mechanisms.
- Building Coping Skills: Learning to manage stress, cravings, and difficult emotions without resorting to substance use is fundamental.
- Peer Support Groups: Participation in groups like Narcotics Anonymous (NA) provides a supportive community where individuals can share experiences and receive encouragement.
- Creating a Foundation for Lasting Sobriety: Comprehensive rehabilitation programs integrate detox with therapy, education, and aftercare planning to build a strong foundation for a drug-free life.
We are committed to helping you find the right path to this comprehensive care. If you’re looking for support in your area, you can easily find a detox clinic near you through our resources.
Finding the Right Path to Recovery
We’ve digd into the complexities of ultra rapid detox, revealing its significant risks, questionable efficacy, and the medical community’s strong recommendations against its routine use. The allure of a quick fix is understandable, but the reality is that such a procedure carries a high risk of serious complications, including death, and offers no proven advantage in achieving long-term sobriety compared to safer, evidence-based methods. The high relapse rates and substantial out-of-pocket costs further underscore why this approach is not recommended.
At Addiction Helpline America, we firmly believe in guiding individuals towards treatments that prioritize their safety, well-being, and sustained recovery. We advocate for medically supervised detox followed by comprehensive rehabilitation programs that address the multifaceted nature of addiction. Our goal is to help you make an informed and safe decision about your treatment journey.
We connect individuals nationwide to addiction and mental health treatment centers, offering free, confidential, and personalized guidance. Our vast network includes vetted programs that adhere to the highest standards of care. When you reach out to us, you’re not just getting information; you’re getting a partner dedicated to finding the right recovery program for you.
Don’t let the fear of withdrawal or the promise of an unproven “rapid” solution deter you from seeking effective help. Your journey to recovery is unique, and it deserves a personalized, safe, and evidence-based approach. Let us help you steer your options and connect you with the support you need. For more information on safe and effective options, explore our complete guide to drug detox facilities.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.