When Every Moment Counts: Understanding Help for Addiction Now
Help for addiction now is available 24/7 through confidential helplines, online treatment locators, and emergency medical services. You don’t have to wait—support is ready when you need it most.
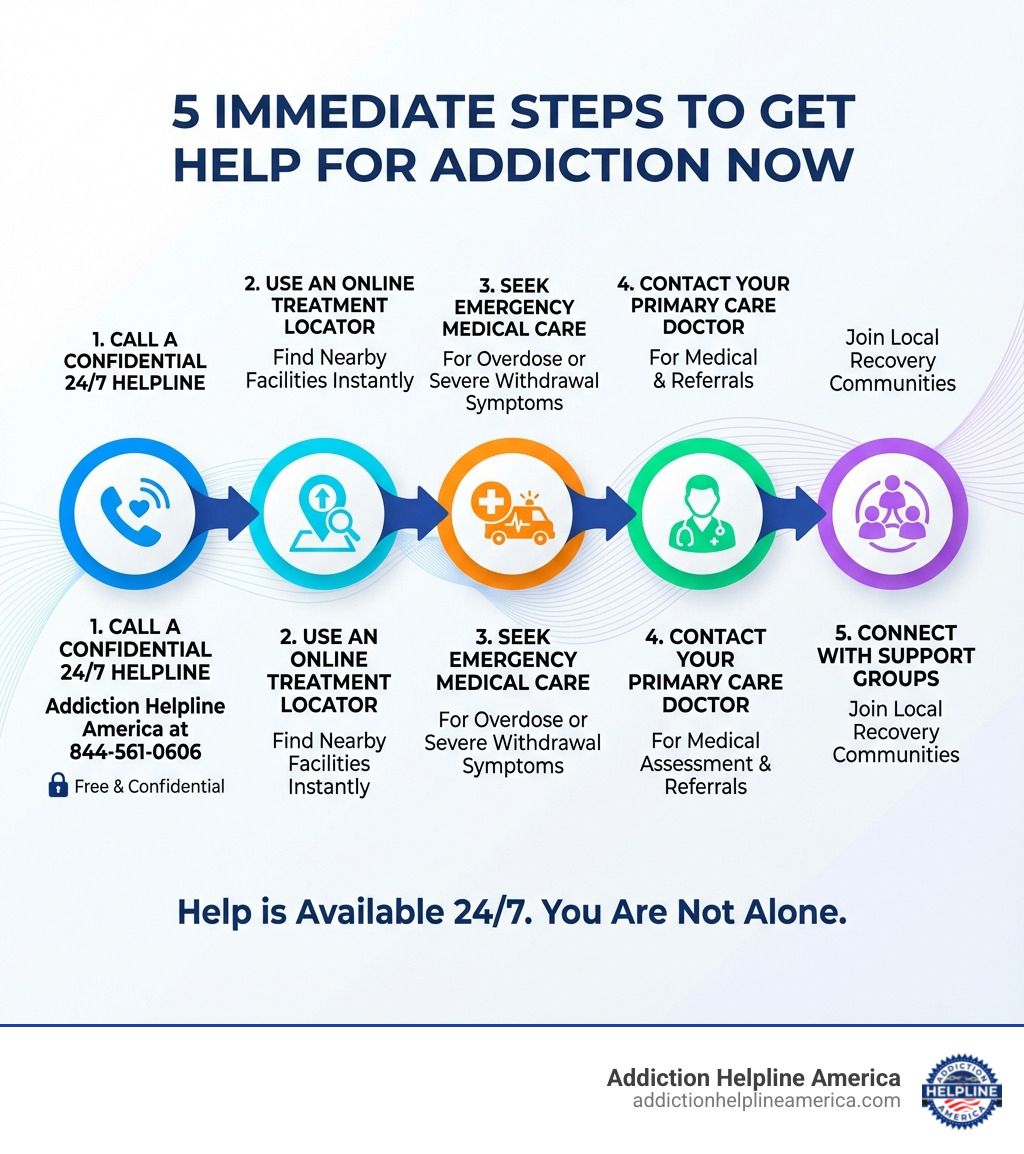
Immediate Resources for Addiction Help:
- Call a 24/7 Helpline – Addiction Helpline America: 844-561-0606 (free and confidential)
- Use an Online Treatment Locator – Find facilities near you instantly
- Seek Emergency Medical Care – For overdose or severe withdrawal symptoms
- Contact Your Doctor – Primary care physicians can provide referrals and medical support
- Reach Out to Support Groups – Connect with others in recovery
Addiction is a brain disease, not a moral failing or lack of willpower. The changes it causes in your brain make it incredibly difficult to stop using substances on your own—and that’s exactly why reaching out for help is one of the bravest and most important decisions you can make.
If you’re reading this, you’ve already taken the hardest step: acknowledging that something needs to change. Whether you’re struggling yourself or worried about someone you love, you are not alone. Millions of Americans face addiction every year, and effective treatment exists.
This guide will walk you through the immediate steps you can take right now to find help, the different treatment options available, and how to build a foundation for lasting recovery. We’ll explain what to expect, answer common questions, and show you that recovery is not only possible—it’s within reach.
At Addiction Helpline America, we’ve spent years connecting individuals and families with the right treatment programs for their unique situations, providing free and confidential support for those seeking help for addiction now. Our trained specialists are available 24/7 to guide you toward the care you need to begin your journey to recovery.
Help for addiction now terms to learn:
Recognizing the Need for Help: Signs It’s Time to Act
Recognizing that you or a loved one needs help is the critical first step towards recovery. Addiction manifests in various ways, affecting a person’s physical health, behavior, psychology, and relationships. It’s not always obvious, and denial can be a powerful barrier. However, understanding the common signs and symptoms can illuminate the path to seeking professional help.
The Mayo Clinic describes drug addiction (substance use disorder) as a disease that affects a person’s brain and behavior and leads to an inability to control the use of a legal or illegal drug or medication. Here are some key indicators:
- Physical Symptoms: These can include changes in appearance (e.g., poor hygiene, weight loss or gain), dilated or constricted pupils, frequent illness, track marks, or unexplained injuries. Increased tolerance, where more of the substance is needed to achieve the desired effect, is a tell-tale sign. The presence of withdrawal symptoms—physical and psychological discomfort when the substance isn’t used—is a strong indicator of dependence.
- Behavioral Changes: You might notice increased secrecy, lying, or evasiveness. There could be a loss of interest in hobbies or activities once enjoyed, neglecting responsibilities at work, school, or home, and engaging in risky or illegal behaviors to obtain or use substances. Financial problems often arise, and legal troubles may follow.
- Psychological Signs: Mood swings, irritability, anxiety, depression, paranoia, and memory problems are common. The individual may become defensive when confronted about their substance use. A pervasive sense of shame or guilt can also be present, driving further isolation.
- Social and Relationship Problems: Addiction often strains relationships with family and friends, leading to conflicts, broken trust, and social isolation. The person may start associating with new friends who also use substances, or withdraw entirely from social circles.
- Neglecting Responsibilities: This includes missing work or school, poor performance, failing to care for children or pets, or neglecting household duties. The substance becomes the priority, overshadowing all other obligations.
- Increased Tolerance: Over time, the body adapts to the presence of a substance, requiring larger doses to achieve the same initial effect.
- Withdrawal Symptoms: When the substance is stopped or reduced, uncomfortable and sometimes dangerous physical and psychological symptoms can occur. These vary depending on the substance but can include nausea, sweating, tremors, anxiety, hallucinations, or seizures.
If these signs resonate with your experience or that of a loved one, it’s a clear signal that professional help is needed.
Understanding Addiction as a Brain Disease
Developing an addiction to drugs isn’t a character flaw or a sign of weakness. Addiction is a complex and chronic brain disease. As the National Institute on Drug Abuse (NIDA) explains, drug abuse can create significant changes in the brain, leading to powerful cravings and compulsions that are incredibly difficult to overcome with willpower alone.
When a person uses substances repeatedly, these drugs alter the brain’s reward system, affecting areas responsible for pleasure, motivation, memory, and decision-making. Over time, the brain adapts to the drug’s presence, requiring it just to feel “normal.” This leads to compulsive drug-seeking and use, despite harmful consequences, and a loss of control over the behavior. This scientific understanding underscores why professional treatment is not just helpful, but often essential for recovery.
When a Loved One is Struggling
Witnessing a loved one struggle with addiction can be heartbreaking and frustrating. Your support can be a powerful catalyst for change, but it’s important to approach the situation effectively. A SAMHSA booklet for families emphasizes the importance of understanding the disease and how to support recovery.
- Observing Changes: Pay attention to the signs listed above. Documenting specific incidents without judgment can be helpful.
- How to Approach the Conversation: Choose a calm, private moment. Express your concerns from a place of love and care, focusing on specific behaviors and their impact, rather than using accusatory language. Use “I” statements (e.g., “I’m worried about you because I’ve noticed…”) instead of “you” statements (“You always…”).
- Expressing Concern Without Judgment: Addiction is a disease. Avoid shaming, blaming, or lecturing. Your goal is to open a dialogue and offer support, not to condemn.
- Setting Boundaries: This is vital for your well-being and to prevent enabling. Clearly communicate what you will and will not tolerate. For instance, you might state you won’t provide money if it’s used for substances, or that you won’t cover for missed responsibilities.
- Avoiding Enabling Behaviors: Enabling means unintentionally allowing the addiction to continue by shielding the person from the natural consequences of their actions. This could involve making excuses, paying their bills, or cleaning up their messes. While born from love, these actions can hinder their motivation to seek help.
- Consider a Professional Intervention: If direct conversations aren’t effective, a professional interventionist can guide family and friends through a structured process to confront the individual and present a clear path to treatment.
Family and friends play a crucial role, not just in encouraging someone to seek help, but also in their long-term recovery journey. Addiction Helpline America is here to support families too, offering guidance on how to steer these challenging situations.
Your First Steps: How to Get Help for Addiction Now
The moment you decide to seek help for addiction now is a pivotal one—a true turning point. It’s often born out of crisis, a moment of clarity, or simply exhaustion from the struggle. Whatever the catalyst, acknowledging this need and taking immediate action is paramount. You don’t need to have all the answers; you just need to take that first step.
This is where your path to recovery truly begins. Overcoming hesitation and reaching out means embracing hope for a better future.
Step 1: Call a Confidential Helpline
When you’re ready for help for addiction now, a confidential helpline is often the fastest and most accessible resource. These helplines are available 24/7, offering free and confidential support from trained specialists. They can provide immediate crisis intervention, offer information about substance use disorders, and, most importantly, connect you with treatment referrals custom to your needs.
At Addiction Helpline America, our dedicated team understands the urgency and sensitivity of your situation. We provide free, confidential, personalized guidance to help you find the right recovery program from our vast network of treatment centers across the United States. Whether you’re in California, Texas, Florida, New York, or any of our locations, we can help you find local support. Don’t hesitate. Call the Addiction Helpline America addiction and rehab hotlines at 844-561-0606 now.
Step 2: Use an Online Treatment Locator
Beyond helplines, online treatment locators are invaluable tools for finding help for addiction now. These platforms allow you to search for facilities based on various criteria, making the process of finding suitable care more manageable.
Our treatment locator tool at Addiction Helpline America is designed to simplify this search for you. You can find a treatment center near you, filtering by the type of addiction, specific services offered, payment options, and even location. This allows you to quickly pinpoint resources in states like Alabama, Arizona, Colorado, Georgia, Illinois, Massachusetts, Michigan, Nevada, North Carolina, Ohio, Oregon, Pennsylvania, Tennessee, and Washington, among others where we have connections. Your search remains anonymous and confidential, protecting your privacy while empowering you with choices. SAMHSA’s FindTreatment.gov is another confidential and anonymous federal resource that can help you locate treatment options for mental and substance use disorders.
Step 3: Consider an Immediate Medical Assessment
In certain situations, immediate medical attention is necessary before beginning long-term treatment. If you or a loved one is experiencing an overdose or severe withdrawal symptoms, an emergency room is the appropriate place to seek help. Medical stabilization is critical in these moments to ensure safety.
For less severe but urgent needs, such as managing uncomfortable withdrawal symptoms or getting a preliminary assessment, urgent care centers or your primary care physician can be valuable resources. They can assess your physical health, provide referrals to specialized detox programs, and offer medical support to make the initial stages of withdrawal safer and more comfortable. Medically-supervised detox is often the first step in treatment, helping to safely purge the body of drugs under professional care. For opioid overdose specifically, having naloxone readily available can be a life-saving measure.
Understanding Your Treatment Options
Once immediate safety is established, understanding the landscape of addiction treatment options is the next crucial step. There is no single “right” path to recovery; instead, successful treatment involves personalized plans custom to an individual’s unique situation, needs, and goals. Evidence-based practices guide these treatments, often incorporating a holistic approach that addresses the whole person—mind, body, and spirit.
Types of Addiction Treatment Programs
Addiction treatment programs vary widely in their structure, intensity, and duration. The right choice depends on the severity of the addiction, co-occurring mental health conditions, and individual circumstances.
- Detoxification (Detox): Often the first step, medical detox helps you safely manage withdrawal symptoms in a supervised environment. This is crucial for substances like alcohol and benzodiazepines, where withdrawal can be life-threatening.
- Inpatient/Residential Treatment: This involves living at a treatment facility for a period, typically 30, 60, or 90 days. It provides an immersive, structured environment with 24/7 support, ideal for those with severe addictions or unstable living situations.
- Outpatient Programs (OP): These programs allow you to live at home while attending treatment sessions at a clinic or facility. They vary in intensity:
- Partial Hospitalization Programs (PHP): The most intensive outpatient option, often involving treatment for several hours a day, five to seven days a week.
- Intensive Outpatient Programs (IOP): A step down from PHP, requiring fewer hours per week but still providing a structured program of therapy and support.
- Sober Living Homes: These are structured, supportive living environments for people who have completed an inpatient program. They help ease the transition back to independent living while reinforcing sober habits.
The Role of Therapy and Counseling in Getting Help for Addiction Now
Therapy is the cornerstone of addiction treatment, helping individuals understand the root causes of their substance use and develop healthier coping mechanisms. Common evidence-based approaches include:
- Cognitive-Behavioral Therapy (CBT): This therapy helps you identify and change negative thinking patterns and behaviors associated with addiction. Research shows CBT is highly effective in preventing relapse.
- Dialectical Behavior Therapy (DBT): DBT is useful for individuals who struggle with intense emotions, teaching skills in mindfulness, distress tolerance, and emotional regulation.
- Family Therapy: Addiction affects the entire family. Family therapy helps repair relationships, improve communication, and create a supportive home environment for recovery.
- Group Therapy: Sharing experiences with peers in a professionally-led group setting provides a sense of community and reduces feelings of isolation.
Medication-Assisted Treatment (MAT)
For some substance use disorders, particularly opioid and alcohol addiction, Medication-Assisted Treatment (MAT) can be a life-saving component of a comprehensive treatment plan. MAT combines behavioral therapies with FDA-approved medications to:
- Reduce cravings
- Relieve withdrawal symptoms
- Block the euphoric effects of opioids and alcohol
Common medications include Buprenorphine (Suboxone) for opioid addiction and Naltrexone for both alcohol and opioid use disorders.
Addressing Co-Occurring Mental Health Disorders (Dual Diagnosis)
It’s very common for addiction to coexist with mental health conditions like depression, anxiety, or PTSD. This is known as a dual diagnosis. For recovery to be successful, it’s crucial to treat both the substance use disorder and the mental health condition simultaneously. An integrated treatment approach addresses the complex interplay between these issues, providing the best chance for lasting wellness. According to the National Alliance on Mental Illness (NAMI), a significant portion of people with substance use disorders also have a co-occurring mental illness.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Help Is Here: Call Our 24/7 Confidential Addiction Helpline
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.