Ever stared at the Medicaid application form and wondered if it actually covers rehab, only to feel a knot of anxiety tighten?
You’re not alone. Many families in the United States hit that exact moment—trying to balance love, fear, and a mountain of paperwork—while hoping to get the right help for a loved one battling addiction.
What we’ve seen over the years at Addiction Helpline America is that the biggest hurdle isn’t the treatment itself; it’s figuring out whether Medicaid will foot the bill. The good news? In most states, Medicaid does include a range of addiction‑treatment services, from inpatient detox to outpatient counseling, but the specifics can feel like a maze.
Think about it this way: Medicaid is like a safety net woven from federal and state threads. Federal rules set the baseline—covering medically necessary services for people who qualify—while each state adds its own flavor, deciding which programs are covered, what prior authorizations look like, and how much you might still pay out of pocket.
So, does Medicaid cover rehab? The short answer is yes, but the long answer depends on where you live, what kind of rehab you need, and whether you meet eligibility criteria. For example, someone aged 65 or older might qualify through Medicare, which works hand‑in‑hand with Medicaid for low‑income seniors. Meanwhile, a younger adult could tap into state Medicaid plans that include both residential and outpatient services, provided the provider accepts Medicaid.
Here’s a quick reality check: If you’re searching for a center, make sure the facility lists Medicaid as an accepted payer. It saves you the heartache of getting a great program only to discover the costs aren’t covered.
And remember, navigating this landscape isn’t a solo mission. Our directory lets you filter by Medicaid‑accepting centers, and our team is ready to walk you through the steps—from confirming eligibility to gathering the right documentation.
Ready to take the next step? Let’s break down the key pieces you’ll need to verify coverage, so you can focus on healing instead of paperwork.
TL;DR
Yes—Medicaid can cover rehab, but the exact services, eligibility rules, and out‑of‑pocket costs vary by state and by whether you qualify for Medicaid alone, Medicare, or a combined program. Use our directory to filter Medicaid‑accepting centers, confirm coverage, and get step‑by‑step help so you can focus on recovery instead of paperwork.
Understanding Medicaid Eligibility for Rehab
When you first hear that Medicaid might foot the bill for rehab, a mix of relief and confusion often shows up. You’re thinking, “Will I actually qualify?” and “What paperwork will I need?” Let’s untangle the eligibility web together.
Medicaid isn’t a single, nationwide program; it’s a partnership between the federal government and each state. That means the baseline rules are the same—cover medically necessary addiction treatment for eligible individuals—but the details can differ dramatically from Alabama to Wyoming.
Eligibility usually hinges on three pillars: income level, disability or medical need, and citizenship or residency status. If your household income falls at or below 138 % of the federal poverty level, you’re generally in the Medicaid pool. Some states also extend coverage to people with certain disabilities, even if they earn a bit more.
But there’s a twist: many adults qualify through the Medicaid expansion created by the Affordable Care Act. Those states that adopted the expansion opened the door for anyone under 65 whose income is up to 138 % of the poverty line, regardless of disability status. If you live in a non‑expansion state, you might still qualify if you’re pregnant, a parent of a minor child, or enrolled in a state‑run program like TennCare or MassHealth.
The next piece of the puzzle is the type of treatment you need. Medicaid covers a spectrum—from medically supervised detox (the first 24‑48 hours) to residential inpatient programs, intensive outpatient, and even after‑care counseling. However, each state decides which services are “medically necessary” and may require prior authorization.
So how do you prove you meet those criteria? First, gather recent pay stubs, tax returns, or a benefits statement that shows your household income. Second, have a doctor or licensed therapist sign a letter that outlines the medical necessity of rehab for your condition. Finally, be ready to fill out the state’s Medicaid application—most of them can be completed online, but some still require a paper form.
If you’re not sure where to start, our directory can save you a lot of headaches. By filtering for “Medicaid‑accepting” facilities, you instantly see which centers have already cleared the insurance hurdle—just like our Does Insurance Cover Rehab: 2025 Ultimate Guide explains. It’s like having a shortcut through the paperwork maze.
Now, a quick checklist you can print out or save on your phone:
- Proof of income (pay stubs, tax return)
- Doctor’s or therapist’s medical‑necessity letter
- Completed state Medicaid application
- Confirmation that the rehab center accepts Medicaid
- Prior‑authorization request (if required)
Now, a word about out‑of‑pocket costs. Even when Medicaid covers the bulk of treatment, you might still be on the hook for small copays, especially for outpatient visits. Those amounts vary by state—some charge as little as $5 per session, others might ask for a modest sliding‑scale fee.
A common question we hear is whether Medicaid will also cover ancillary services like medication‑assisted treatment (MAT) or wellness coaching. The answer is usually yes—MAT, including buprenorphine and naltrexone, is considered a core component of addiction care and is reimbursed in most state plans. For extra wellness support, you might explore programs like XLR8well’s proactive health programs, which some providers can integrate as supplemental services.
Below is a short video that walks through the Medicaid enrollment steps.
Take notes as you watch—those forms are the same ones you’ll fill out later.
While you’re watching, think about the support network you’ll need once treatment starts. Family, friends, and even community groups can make the difference between a smooth recovery and a relapse. Our platform lets you connect with local peer‑support groups that accept Medicaid funding.

Finally, remember you’re not alone in this maze. If you hit a snag, give us a call or chat with one of our advisors. They can help you verify a center’s Medicaid status, double‑check your paperwork, and even reach out to the provider on your behalf. And if you’re curious about complementary wellness options, consider learning about ORYGN’s metabolic wellness supplements, which some patients discuss with their doctors as part of a holistic recovery plan.
What Types of Rehab Programs Are Covered by Medicaid?
When you finally get past the paperwork maze, the next question that pops up is: “What kind of treatment actually gets paid for?” Trust me, you’re not the only one wondering if Medicaid will foot the bill for inpatient detox, residential stays, or outpatient counseling. The short answer is yes—Medicaid does cover a spectrum of rehab services—but the details can feel like a jigsaw puzzle.
Inpatient Detox and Residential Care
Most states consider medically supervised detox a “medically necessary” service, so Medicaid will cover the initial withdrawal period. After detox, many programs transition you into a residential rehab unit, where you get 24/7 support, therapy, and often medication‑assisted treatment (MAT). For example, in Indiana a client with an MRO package received a 30‑day residential stay with all costs covered, plus a tiny co‑pay that was later waived once the annual cap kicked in.
Tip: ask the admissions coordinator if the center’s residential unit is Medicaid‑certified. If it isn’t, you might end up paying out‑of‑pocket for a portion of the stay.
Intensive Outpatient Programs (IOP) and Standard Outpatient Therapy
Once you’re stable enough to leave a live‑in setting, Medicaid usually picks up intensive outpatient programs. IOPs typically involve 3‑5 days a week of therapy, group counseling, and sometimes medication management. A real‑world scenario from North Carolina shows that over 300 centers accept Medicaid for IOP, offering everything from CBT to family therapy.
We’ve seen families in Tennessee who moved from a 14‑day inpatient detox straight into a Medicaid‑covered IOP, saving them thousands of dollars while still getting the structure they needed.
Medication‑Assisted Treatment (MAT)
MAT—think buprenorphine, naltrexone, or methadone—has become a cornerstone of modern addiction care. Federal guidelines require Medicaid to cover MAT when it’s prescribed by a licensed provider. In Nevada, Medicaid reimburses for both the medication and the accompanying counseling sessions, as long as the provider is in‑network.
Actionable step: ask your prescriber to submit a prior authorization for MAT. It’s a quick paperwork step that can prevent a surprise bill later.
Partial Hospitalization (PHP) and Day Treatment
PHP sits between inpatient and outpatient: you spend most of the day at a treatment center but go home at night. Many states, including Ohio and Illinois, list PHP as a covered service under their Medicaid Behavioral Health packages. It’s a solid option if you need more intensity than standard outpatient but can’t commit to a full residential stay.
Pro tip: check if the PHP program offers “wrap‑around” services like childcare or transportation vouchers—some states bundle those into Medicaid benefits.
Specialized Programs
Some Medicaid plans go the extra mile and cover niche programs: pregnant‑and‑postpartum mothers, veterans, or youth‑focused residential homes. For instance, a women‑only residential program in North Carolina that offers on‑site childcare is Medicaid‑approved, letting a single mom stay focused on recovery without worrying about her child’s care.
And if you’re dealing with co‑occurring mental health issues, look for a dual‑diagnosis program. Medicaid often requires that mental health and SUD services be integrated, meaning you can get both in one place.
How to Verify Coverage
- Call your state Medicaid helpline and ask for the specific code (e.g., “MRO” or “Behavioral Health”) that covers rehab.
- Ask the treatment center to provide a written estimate that shows what Medicaid will pay and what, if anything, you’ll owe.
- Use our Drug And Alcohol Rehabilitation Centers: New 2025 Hope guide to filter for Medicaid‑accepting facilities in your area.
Remember, every state writes its own rules, so what’s covered in Alabama might look different in California. The key is to line up the right level of care with the right Medicaid code.
Beyond the core services, many people wonder about the “extra” stuff that can make recovery smoother—like nutrition counseling, fitness programs, or wellness coaching. That’s where supplemental resources come in. XLR8well offers proactive health coaching that some Medicaid plans can bundle as a wellness benefit, while ORYGN provides metabolic‑wellness supplements that patients sometimes discuss with their providers as part of a holistic recovery plan.
Bottom line: Medicaid’s coverage is broader than many assume, spanning detox, residential rehab, outpatient therapy, MAT, and even specialized programs for specific populations. By confirming the program’s Medicaid status, checking for any co‑pay caps, and leveraging resources like our directory, you can turn the question “does Medicaid cover rehab?” into a confident “yes, and here’s how.”
How to Apply for Medicaid Rehab Coverage
Okay, you’ve figured out that Medicaid does cover rehab – that’s a win. Now comes the part that feels like you’re assembling IKEA furniture without the instructions: actually getting the coverage approved. The good news? It’s a series of small, doable steps, not a marathon.
1. Confirm the program’s Medicaid status before you sign anything
Pick a handful of facilities that look right for your loved one. Call the admissions office and ask, “Is this program Medicaid‑certified for the specific code you need (MRO, Behavioral Health, etc.)?” If they’re not sure, ask for the name of the billing contact who can verify it. A quick email confirmation can save you weeks of back‑and‑forth later.
2. Gather the core paperwork
Most state Medicaid portals let you upload documents, but having a ready‑to‑go folder on your phone speeds things up. You’ll need:
- Photo ID (driver’s license or passport)
- Proof of residence – a recent utility bill or lease agreement
- Income proof – recent pay stubs, a W‑2, or a benefits statement (SSI, SNAP, etc.)
- Medical documentation – a physician’s note or a formal diagnosis of a substance‑use disorder
- Any prior authorizations the treatment center already secured
Tip: label each file clearly (e.g., “ID.pdf”, “PayStub_Jan2025.pdf”) so the caseworker can find them in a second.
3. Fill out the Medicaid application
Every state has its own portal, but the flow is similar:
- Log in or create an account on your state’s Medicaid website.
- Select the “Apply for New Benefits” or “Renew Existing Benefits” option.
- Enter personal information exactly as it appears on your ID – no nicknames.
- Upload the documents you gathered in step 2.
- Answer the health‑condition questions. When they ask about a substance‑use disorder, be honest; the system flags it for the “rehab” benefit line.
- Submit and note the reference number. You’ll need it for any follow‑up calls.
If the online form trips up, you can call the state Medicaid helpline. Have your reference number handy and ask them to walk you through the fields you’re unsure about.
4. Get a prior‑authorization (PA) from the treatment center
Most rehab programs can’t start until the Medicaid PA is approved. Here’s how to make it painless:
- Ask the center’s billing specialist to fill out the PA form. They know the exact code (e.g., “MRO‑01”) the state expects.
- Provide the specialist with the diagnosis note and any assessment results (ANSA, ASAM level of care, etc.).
- Submit the PA directly to your state Medicaid office – many centers do this electronically.
- Follow up after 48 hours. A quick call saying, “Just checking on the status of my PA” often nudges the process.
Real‑world example: Maria in Indiana’s rural county called her center’s billing team, who sent the PA within an hour. She called her Medicaid caseworker two days later, got a “approved” email, and moved into a 30‑day residential program the same week.
5. Verify any co‑pay or cost‑share details
Even when Medicaid says “covered,” some states still charge a modest co‑pay until you hit an annual cap. Ask the center: “What will I owe out‑of‑pocket before Medicaid takes 100 %?” Write down the amount and the cap threshold. If the co‑pay seems high, you can request a waiver – many caseworkers grant them for families facing financial hardship.
6. Keep a paper‑trail of every interaction
Save every email, note the date and name of each person you speak with, and take screenshots of portal confirmations. If something falls through, you’ll have a clear audit trail to present to a supervisor.
7. Use a trusted resource to double‑check your choices
When you’re juggling phone calls and forms, a reliable guide can be a lifesaver. Our Alabama Medicaid rehab cost guide breaks down typical fees, co‑pay caps, and state‑specific quirks, so you can compare what you’re seeing in the field with what the official numbers say.
Bottom line: applying for Medicaid rehab coverage feels like a checklist, but each item is a small win that gets you closer to treatment. Grab your documents, confirm the program’s code, push the prior‑authorization, and keep notes. Before you know it, you’ll have that green light and can focus on the real work – healing.
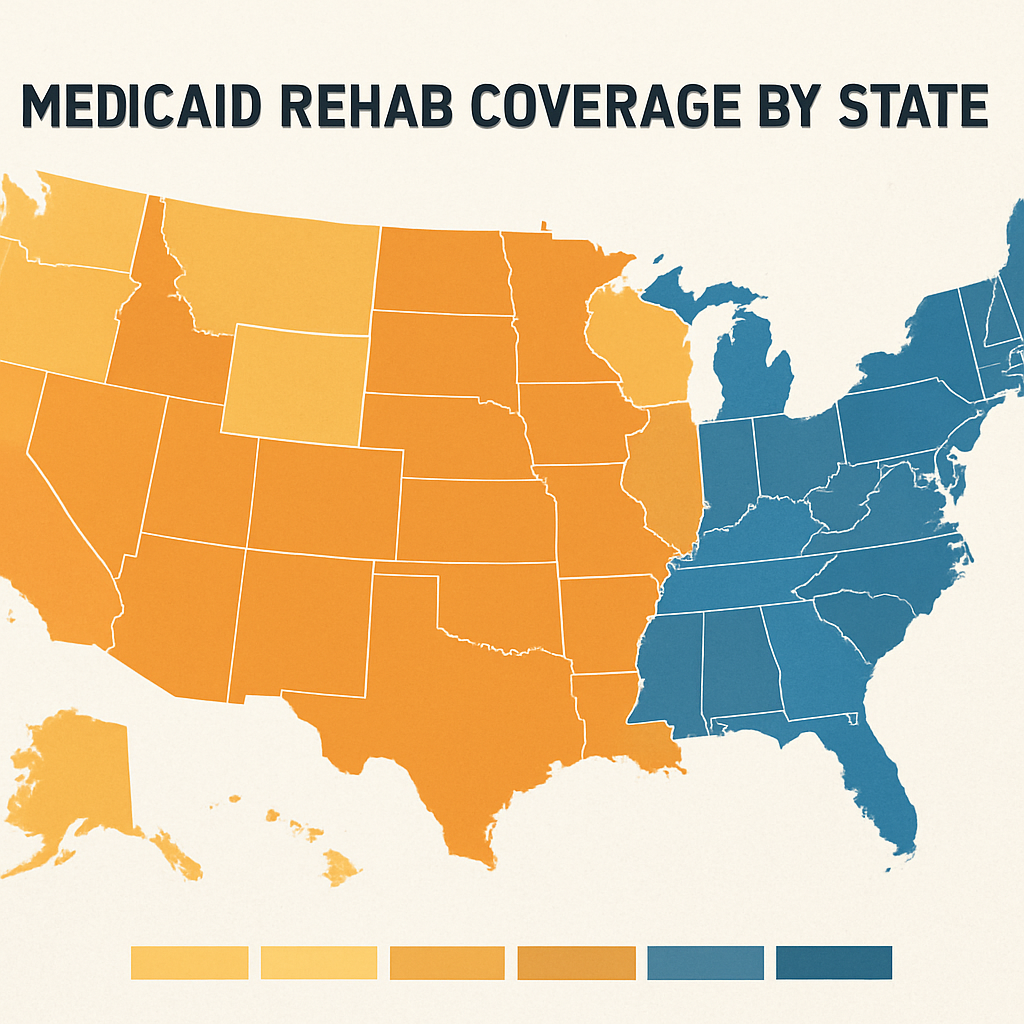
State‑by‑State Coverage Variations
When you ask yourself “does Medicaid cover rehab?” the answer almost always starts with “it depends” – and the “depends” is usually the state you live in. I’ve spoken with dozens of families across the country, and the biggest surprise is how wildly the rules change from Alabama to Alaska.
Think about the last time you ordered a pizza. You check the menu, see what toppings are available, and then call the place to confirm they have what you want. Medicaid works the same way: each state publishes its own “menu” of covered services, co‑pay caps, and prior‑authorization codes. The federal baseline guarantees a minimum package – medically necessary detox and counseling – but every state adds its own flavor.
Key variables that differ state‑to‑state
- Covered levels of care: Some states, like California and New York, pay for both inpatient detox and 30‑day residential rehab. Others, such as Texas, limit coverage to outpatient counseling unless you qualify for a waiver.
- Prior‑authorization requirements: In Illinois, the Medicaid Behavioral Health (MBH) code triggers an automatic approval for accredited facilities, while in Mississippi you’ll often need a physician’s letter and a detailed treatment plan before the claim is processed.
- Co‑pay caps: Indiana caps co‑pays at $100 per year for addiction services; Florida sets the cap at $75 but only after you’ve met a $25 deductible.
- Specialized programs: Some states offer Medicaid‑funded programs for pregnant mothers, veterans, or youth. For example, Massachusetts’ MassHealth covers on‑site childcare at certain residential centers, and Tennessee’s TennCare includes a “Family Support” add‑on for parents of teens in treatment.
So how do you turn that patchwork into a clear path forward? Here are three concrete steps you can take right now.
Step 1 – Pull the latest state Medicaid handbook
Every state posts a PDF or web page that lists covered SUD services, the relevant billing codes, and any out‑of‑pocket limits. Look for sections titled “Substance Use Disorder Treatment” or “Behavioral Health Services.” If the language feels dense, copy the table into a spreadsheet and highlight the rows that match the level of care you need (detox, residential, IOP, etc.).
Tip: The handbook often mentions a phone line for “coverage verification.” Give them a call and ask, “Can you confirm that Medicaid will cover an 28‑day residential program under code MRO‑01 for my zip code?” Write down the name of the representative and the reference number they give you.
Step 2 – Verify the rehab center’s Medicaid status
Even if your state’s handbook says the service is covered, the center itself must be Medicaid‑certified. A quick way to double‑check is to use our directory and filter by the state you’re researching. For example, our Illinois Alcohol Rehab: Top Affordable Options 2026 guide lists every facility that currently accepts Illinois Medicaid, along with the specific codes they bill.
When you call the admissions office, ask for the exact Medicaid billing code they use and request a written estimate that shows the portion you’ll owe before the annual cap kicks in.
Step 3 – Prepare a short “coverage checklist”
- State Medicaid handbook URL and page number where your service is listed.
- Center’s Medicaid certification number.
- Required prior‑authorization form (often a one‑page PDF).
- Co‑pay cap amount and any waivers you might need.
- Contact info for your state’s Medicaid helpline.
Having this checklist on hand makes the phone calls feel less like a guessing game and more like a structured interview.
Real‑world example: Maria in Indiana was told her local clinic didn’t accept Medicaid. After pulling the Indiana Medicaid handbook, she discovered a separate “MRO” program that covered exactly what she needed. She called the clinic’s billing manager, quoted the code, and got the prior authorization approved within 48 hours. The result? A fully covered 30‑day residential stay with a $0 co‑pay because she hit the state’s $100 cap early in the year.
Another case: A family in Nevada thought Medicaid wouldn’t cover medication‑assisted treatment (MAT). By reviewing Nevada’s Medicaid Behavioral Health guide, they learned that buprenorphine is covered when paired with counseling under code “MAT‑01.” After confirming the clinic’s certification, the family secured both the medication and weekly counseling without any out‑of‑pocket cost.
These stories illustrate a simple truth: the more you know about your state’s specific rules, the more leverage you have when talking to providers.
Finally, remember that Medicaid isn’t the only piece of the puzzle. Many states allow you to combine Medicaid with state‑run scholarship funds or grant programs that cover the remaining co‑pay. A quick search for “[Your State] Medicaid rehab scholarship” can reveal extra dollars you didn’t know existed.
And if you’re curious about complementary therapies that many people explore during recovery – like CBD for anxiety or sleep – you might want to learn about reputable sources. Iguana Smoke CBD products are one option that some families consider, though they’re not covered by Medicaid and would be an out‑of‑pocket purchase.
Costs You May Still Be Responsible For
Even when Medicaid says “covered,” you’ll still see line items that make you pause. It’s like ordering a pizza with “all the toppings” and then getting a surprise charge for extra cheese. Below we break down the most common pockets where you might still pay out‑of‑pocket, and what you can do about each one.
1. Co‑pay caps and annual limits
Most states set a yearly cap on how much you owe for addiction‑treatment services. Before you hit that ceiling, you could be asked to pay a modest co‑pay per visit – $5, $10, sometimes $20. Once the cap is reached (often $75‑$100), Medicaid steps in and covers 100 % of the remaining charges.
Tip: ask the admissions office for the exact co‑pay amount and the cap number before you sign any paperwork. Knowing the ceiling helps you budget and avoid surprise bills.
2. Services Medicaid doesn’t list as “medically necessary”
Things like nutrition counseling, fitness classes, or holistic therapies (yoga, acupuncture) often feel essential to recovery, but many Medicaid plans classify them as optional. If you want those extras, you’ll usually have to cover them yourself.
One workaround is to see if your state’s Medicaid handbook mentions “wellness benefits” – some programs bundle a limited number of wellness visits into the overall coverage.
3. Transportation, childcare, and ancillary costs
Getting to a treatment center isn’t free. Gas, public‑transit fares, or even a ride‑share can add up, especially if you’re attending an intensive outpatient program (IOP) three times a week. A single parent might also need childcare while they’re in a residential stay.
Some states offer vouchers or reimbursements for these ancillary costs, but you have to request them upfront. Call your state Medicaid helpline and ask, “Do you provide transportation or childcare assistance for rehab services?”
Below is a quick side‑by‑side look at the typical out‑of‑pocket items you might see and how you can mitigate them:
| Cost Category | Typical Amount | How to Reduce / Avoid |
|---|---|---|
| Co‑pay per visit | $5‑$20 | Ask for the annual cap; once reached, payments stop. |
| Non‑covered therapies (yoga, nutrition) | $50‑$200 per month | Check if your state’s Medicaid includes “wellness benefits” or use community resources. |
| Transportation / childcare | $0‑$150 per month | Request vouchers or reimbursements from the state Medicaid office. |
And remember, not every extra cost is a dead end. Many local charities, faith‑based groups, or state grant programs offer supplemental funds that can plug those gaps. A quick Google search for “[Your State] rehab transportation assistance” often uncovers a hidden resource.
We also like to point folks to our Paying For Addiction Treatment guide. It walks you through every financial nook – from sliding‑scale fees to scholarship programs – so you can match the right help to your budget.
Now, let’s watch a short video that walks through a typical Medicaid billing flow. Seeing the steps on screen can make the whole process feel less like a mystery.
After the video, take a moment to list the three cost categories that apply to you. Write them down, then call your Medicaid helpline and ask specifically about each one. Turning a vague worry into a concrete question often speeds up the answer.
Bottom line: Medicaid can cover the bulk of rehab, but you’ll likely still see co‑pays, optional therapies, and logistical expenses. By asking the right questions up front, you can keep those extra dollars from sneaking up on you and stay focused on what truly matters – the recovery journey.
Tips for Maximizing Your Rehab Benefits
Feeling a little overwhelmed after learning that Medicaid can cover most of the rehab bill? You’re not alone. The paperwork, the co‑pays, the “what’s actually covered?” questions can feel like a maze. Below are practical, down‑to‑earth tips that turn confusion into confidence, so you can focus on healing instead of hunting receipts.
1. Confirm the exact Medicaid code your program uses
Every state has its own billing codes – MRO‑01 for intensive residential care, MBH‑02 for outpatient counseling, and so on. Ask the admissions office, “Which Medicaid code will you bill for my loved one’s level of care?” Write that code down, then call your state’s Medicaid helpline and repeat it. When you speak the same language, the representative can pull the precise coverage rules and tell you if any prior‑authorizations are needed.
2. Get a written estimate before you sign anything
Ask the center to provide a line‑item estimate that shows what Medicaid will cover, what you’ll owe per visit, and where the annual co‑pay cap sits. A clear number prevents surprise bills later. In our experience, families who have that paper (or PDF) in hand can negotiate a waiver if the co‑pay looks higher than the state’s published limit.
3. Track every interaction in a simple spreadsheet
Create a three‑column sheet: Date, Contact (name & phone), and What Was Said. Snap a photo of every email or portal screenshot and attach it. When a claim is denied, you’ll have a ready audit trail to bring to a supervisor – and you’ll feel less like you’re shouting into the void.
4. Use the state’s pharmacy prior‑approval list for medication‑assisted treatment
Medicaid often requires a pre‑approval for buprenorphine, naltrexone, or methadone. North Carolina, for example, publishes a detailed list of approved drugs and the criteria you must meet here. Check that list early, ask your prescriber to submit the paperwork, and follow up within 48 hours. Getting that green light early avoids a treatment gap that could derail progress.
5. Ask about ancillary benefits you might not know exist
Transportation vouchers, childcare stipends, and wellness visits are often tucked into the fine print. One family in Indiana discovered that the state’s “Family Support” add‑on covered bus passes for their teen’s IOP sessions. Call the Medicaid helpline and say, “Do you offer transportation or childcare assistance for my rehab plan?” Write down the answer and the claim number.
6. Leverage community scholarships or grant programs
Many states run supplemental scholarship funds that plug any remaining co‑pay after you hit the annual cap. A quick Google search for “[Your State] rehab scholarship” can surface a one‑time grant that covers things like nutrition counseling or after‑care groups. Even a modest $200 grant can offset a month of non‑covered therapy.
7. Schedule a “benefits check‑in” every three months
Medicaid rules change, and so do your needs. Set a calendar reminder to call your caseworker, confirm that your current code still matches your level of care, and ask whether new services (like tele‑health counseling) have become eligible. A brief 10‑minute call can save you weeks of paperwork down the road.
Bottom line: maximizing Medicaid rehab benefits is all about asking the right questions, documenting every step, and staying proactive about the hidden resources that states already offer. Grab your checklist, make those calls, and let the coverage do the heavy lifting while you focus on recovery. Remember, every small step adds up to a smoother journey.
FAQ
Does Medicaid cover inpatient rehab?
Yes, most states consider medically supervised detox and a full residential stay medically necessary, so Medicaid will pay for the core services. You’ll usually need a physician’s assessment or an MRO (Medicaid Rehabilitation Option) code to trigger the coverage. The exact amount covered can vary – some programs require a small co‑pay until you hit the state‑wide annual cap, after which everything is 100 % covered.
What outpatient programs are covered by Medicaid?
Medicaid typically covers Intensive Outpatient Programs (IOP) and standard outpatient counseling once you’re stable enough to leave a live‑in setting. The coverage includes group therapy, individual counseling, and often medication‑assisted treatment (MAT) if it’s prescribed by an in‑network provider. Check your state’s specific code – it might be listed as MBH‑02 or a similar behavioral health identifier – to confirm the level of care you’ll receive.
Are co‑pays required and how do annual caps work?
Most states set a yearly co‑pay limit for addiction services, usually somewhere between $75 and $100. You’ll pay a modest amount per visit (often $5‑$20) until the cap is reached, then Medicaid covers 100 % of any further services. Ask the admissions office for the exact co‑pay amount and the cap number before you sign anything, so you can budget and avoid surprise bills.
How do I find a Medicaid‑approved treatment center?
Start by using a trusted directory that filters facilities by Medicaid acceptance – that’s where we see the most reliable results. Call the center’s admissions team and ask for the specific Medicaid billing code they use (e.g., MRO‑01, MBH‑02). Request a written estimate that shows what Medicaid will pay and what, if anything, you’ll owe. Verifying the certification number with your state’s Medicaid helpline adds an extra layer of confidence.
What paperwork do I need to get Medicaid rehab coverage?
Gather a photo ID, proof of residency (utility bill or lease), recent pay stubs or a benefits statement, and a medical note confirming a substance‑use disorder diagnosis. Some states also want an assessment report like an ANSA or ASAM level‑of‑care sheet. Upload everything to your state’s Medicaid portal or email the documents to your caseworker. Keeping each file clearly labeled (e.g., “ID.pdf”, “PayStub_Jan2025.pdf”) speeds up the review.
Can Medicaid help with transportation or childcare?
Many states include ancillary benefits such as bus vouchers, ride‑share reimbursements, or childcare stipends for families in treatment. The key is to ask the right question: call your state Medicaid helpline and say, “Do you provide transportation or childcare assistance for my rehab plan?” Write down the representative’s name, the claim number they give you, and any eligibility criteria you need to meet.
What should I do if my Medicaid claim is denied?
First, get the denial letter in writing and note the specific reason – it might be a missing code, an incomplete prior‑authorization, or a documentation gap. Contact the billing department at the treatment center; they can often resubmit the claim with the correct code or add the missing paperwork. If the center can’t fix it, appeal the decision through your state’s Medicaid appeals process, keeping a detailed spreadsheet of every call, email, and date.
Conclusion
So, after wading through the codes, checklists, and phone calls, you might still wonder—does Medicaid cover rehab? The short answer is yes, but the details depend on your state, the level of care, and a few paperwork steps.
We’ve seen families turn a confusing maze into a clear path by confirming the exact Medicaid code, grabbing a written estimate, and keeping a simple spreadsheet of every call. Those three moves alone can stop surprise bills before they even appear.
Remember, co‑pay caps usually sit around $75‑$100 per year, and once you hit that limit Medicaid picks up 100 % of the remaining costs. If your state offers transportation vouchers or childcare stipends, ask for them now—many people miss out simply because they never asked.
A quick final tip: set a reminder to touch base with your caseworker every few months. Rules shift, and a brief 10‑minute call can save you weeks of paperwork later.
In the end, the biggest hurdle is often just getting started. Use the tools and checklists we’ve shared, lean on directories like Addiction Helpline America to verify Medicaid‑approved facilities, and keep your documentation tidy. You’ve already done the hardest part—knowing that Medicaid can fund the care you need. Now it’s time to move forward and focus on recovery.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.