Finding Hope: Your Path to Recovery Starts With Understanding Your Coverage
Cigna insurance in network drug rehab facilities virginia offer comprehensive treatment options for individuals and families facing addiction. With over 90 centers in Virginia accepting Cigna, you have access to quality care that can significantly reduce your out-of-pocket costs. Here’s what you need to know:
Quick Facts:
- Number of Facilities: 90+ centers in Virginia accept Cigna insurance
- Coverage: Cigna covers detox, inpatient, outpatient, and therapy services
- In-Network Benefits: Lower costs, direct billing, negotiated rates
- Verification: Call the number on your ID card or use the myCigna portal
- Network Types: HMO, PPO, EPO, and POS plans available
When addiction takes hold, it can feel like life is spiraling out of control. The good news is that recovery is possible, and your Cigna insurance can help make treatment affordable.
Finding the right facility can feel overwhelming. Understanding your insurance is crucial, as Cigna plans typically cover medical detox, residential treatment, intensive outpatient programs, and ongoing therapy. The key is finding in-network providers who have contracted rates with Cigna, which means lower costs for you.
At Addiction Helpline America, we’ve guided thousands of individuals through the process of using their Cigna insurance in network drug rehab facilities virginia to access life-saving treatment. Our team understands both the insurance landscape and the urgent need for compassionate, effective care when addiction strikes. We provide free, confidential, and personalized guidance, connecting you to the right recovery program from our vast network of treatment centers.
Find more about cigna insurance in network drug rehab facilities virginia:
Understanding Your Cigna Coverage for Addiction Treatment in Virginia
When you’re ready to seek help for addiction, understanding your insurance coverage shouldn’t add to your stress. The good news is that Cigna offers strong coverage for addiction treatment in Virginia—and it’s not just because they want to help (though they do). It’s actually required by federal law.
The Mental Health Parity and Addiction Equity Act (MHPAEA) changed everything for people seeking addiction treatment. This law says that insurance companies like Cigna can’t treat mental health and substance use disorder benefits differently than other medical benefits. In practical terms, this means your Cigna plan must cover addiction treatment with the same level of support it provides for, say, a broken leg or diabetes management.
The Affordable Care Act (ACA) took things even further by making behavioral health treatment—including substance use disorder treatment—one of the essential health benefits that most health plans must cover. This combination of laws means you have real, meaningful coverage for addiction treatment, not just token benefits.
Cigna also operates through Evernorth health services, which delivers flexible health solutions including addiction treatment coverage. Depending on your specific plan, Evernorth may be the name you see on some of your coverage documents.
Now, here’s something really important: the difference between in-network and out-of-network providers. In-network providers are facilities that have agreements with Cigna. They’ve negotiated specific rates for their services, which means lower costs for you. When you choose Cigna insurance in network drug rehab facilities virginia, you’ll typically pay just your copay or coinsurance after meeting your deductible.
Out-of-network providers don’t have these agreements with Cigna. While some plans offer partial coverage for out-of-network care, you’ll almost always pay significantly more. You might even need to pay the full amount upfront and then file for reimbursement later—adding financial stress when you need it least. That’s why we always recommend starting your search with in-network facilities.
Key Insurance Terms You Need to Know
Insurance jargon can be confusing, but you only need to know a few key terms when looking at addiction treatment:
Your deductible is the amount you pay for covered services before Cigna starts paying. For example, if your deductible is $2,000, you’ll pay that amount first. After that, your insurance begins sharing the costs. Understanding your deductible can help you plan financially.
A copayment (or copay) is a fixed fee you pay for specific services after meeting your deductible, like $25 for a therapy session. It’s a predictable cost.
Coinsurance works differently. Instead of a fixed amount, you pay a percentage of the treatment cost. If your plan has 20% coinsurance and you’ve met your deductible, you’d pay 20% of the allowed amount for services while Cigna covers the remaining 80%.
The out-of-pocket maximum is your financial safety net—the most you’ll pay in a year for covered services. Once you hit this limit, Cigna pays 100% of covered costs for the rest of the year.
If these terms are confusing, Cigna’s glossary of terms provides detailed explanations.
Cigna Plan Types and Tiers
Cigna offers several types of health plans, and knowing which one you have is key to accessing treatment.
HMO plans (Health Maintenance Organization) require you to work through a primary care physician (PCP) for referrals to in-network facilities. Out-of-network care is usually not covered except in emergencies, so staying in-network is essential.
PPO plans (Preferred Provider Organization) give you more freedom, as you don’t need referrals. While you can use out-of-network providers, you’ll save significantly by choosing in-network options. PPOs balance flexibility with cost savings.
EPO plans (Exclusive Provider Organization) are similar to HMOs and only cover in-network care, but you typically don’t need a PCP referral. This offers some flexibility with predictable costs.
POS plans (Point-of-Service) blend HMO and PPO features. You might need a PCP and referrals for in-network care, but you can also go out-of-network if you’re willing to pay more.
Beyond these structures, many Cigna plans fall into “metal tiers” that show how costs are split between you and your insurance:
| Metal Tier | Cigna Pays (Approx.) | You Pay (Approx.) |
|---|---|---|
| Bronze | 60% | 40% |
| Silver | 70% | 30% |
| Gold | 80% | 20% |
| Platinum | 90% | 10% |
Bronze plans have lower monthly premiums but higher costs when you need care. Platinum plans cost more each month but cover more of your treatment expenses. The best choice depends on your situation and anticipated care needs.
Your plan documents have the exact details. At Addiction Helpline America, we help you understand your plan and find the right Cigna insurance in network drug rehab facilities virginia. We’re here to make the process easier for you.
Levels of Care and Therapies Covered by Cigna
When you’re facing addiction, you need treatment that meets you exactly where you are. What works for one person might not work for another. That’s why Cigna doesn’t just offer a single treatment option—they cover a full spectrum of care levels, each designed to address different needs and stages of recovery.
Your Cigna plan recognizes that medically necessary treatment is the standard. This means coverage isn’t arbitrary—it’s based on what clinical professionals determine you need to recover safely and effectively. Many facilities use the American Society of Addiction Medicine (ASAM) Criteria to match you with the right level of care. These evidence-based guidelines help ensure you’re getting neither too little nor too much treatment, but exactly what will serve your recovery best.
One crucial aspect of comprehensive addiction treatment is addressing dual diagnosis or co-occurring disorders. This means treating both your addiction and any mental health conditions—like depression, anxiety, PTSD, or bipolar disorder—simultaneously. These conditions often fuel each other, and treating only one while ignoring the other rarely leads to lasting recovery. Cigna’s coverage extends to dual diagnosis treatment, recognizing that true healing addresses the whole person.
What Levels of Care Does Cigna Cover?
Your recovery journey might start with intensive care and gradually step down, or you might begin at a lower level. Here’s what Cigna typically covers:
Medical Detoxification is often the first step, especially for withdrawal from alcohol, opioids, or benzodiazepines. Medical detox provides 24/7 medical supervision to manage symptoms safely and make you as comfortable as possible. Cigna generally covers medically necessary detox at Cigna insurance in network drug rehab facilities virginia.
Inpatient and Residential Treatment Programs provide a complete break from triggering environments. You live at the facility for 30, 60, or 90 days, immersed in a structured schedule of therapy and wellness activities. This intensive care offers the best chance at building a strong foundation for recovery.
Partial Hospitalization Programs (PHP) are a middle ground. You receive intensive treatment during the day (often 5-7 days a week) but return home or to sober living at night. PHP is ideal for those stepping down from residential care or who need more support than standard outpatient but have a stable home.
Intensive Outpatient Programs (IOP) provide structured treatment while allowing you to maintain daily responsibilities. You attend therapy and group sessions 3-5 days a week for a few hours daily, making it ideal for those who need to continue working or caring for family.
Standard Outpatient Programs (OP) are the lowest intensity level, often involving weekly therapy. Many people use OP to maintain recovery skills after completing a more intensive program while reintegrating into daily life.
Common Therapies and Substances Treated
Cigna covers research-based, effective therapeutic approaches.
Cognitive Behavioral Therapy (CBT) helps you identify negative thought patterns that lead to substance use and develop healthier coping skills. It’s a practical, focused, and highly effective approach in addiction treatment.
Dialectical Behavioral Therapy (DBT) teaches skills in mindfulness, distress tolerance, and emotional regulation. It’s particularly helpful for co-occurring disorders like depression or anxiety.
Medication-Assisted Treatment (MAT) combines therapy with FDA-approved medications like Suboxone, Methadone, or Naltrexone. These medications reduce cravings and ease withdrawal, making it easier to focus on recovery. MAT is the gold standard for opioid use disorder, and Cigna typically covers these services.
Trauma-informed care recognizes that many people with addiction have experienced trauma. This approach creates a safe environment and integrates an understanding of trauma into all aspects of treatment, helping to heal the root causes of addiction.
Cigna insurance in network drug rehab facilities virginia treat the full range of substance use disorders. Whether you’re struggling with alcohol addiction, opioid use disorder (including heroin and prescription painkillers), stimulant abuse (like cocaine or methamphetamine), benzodiazepine dependence (Xanax, Valium, Klonopin), marijuana, or prescription drug misuse—quality treatment is available and covered under your plan. The key is finding the right facility that specializes in your specific needs.
How to Find Cigna Insurance In-Network Drug Rehab Facilities in Virginia
Finding the right treatment center doesn’t have to feel overwhelming. With over 90 facilities across Virginia accepting Cigna, you have options—and we’re here to help you steer them. At Addiction Helpline America, we’ve walked thousands of people through this process, and we know the steps that make it simpler.
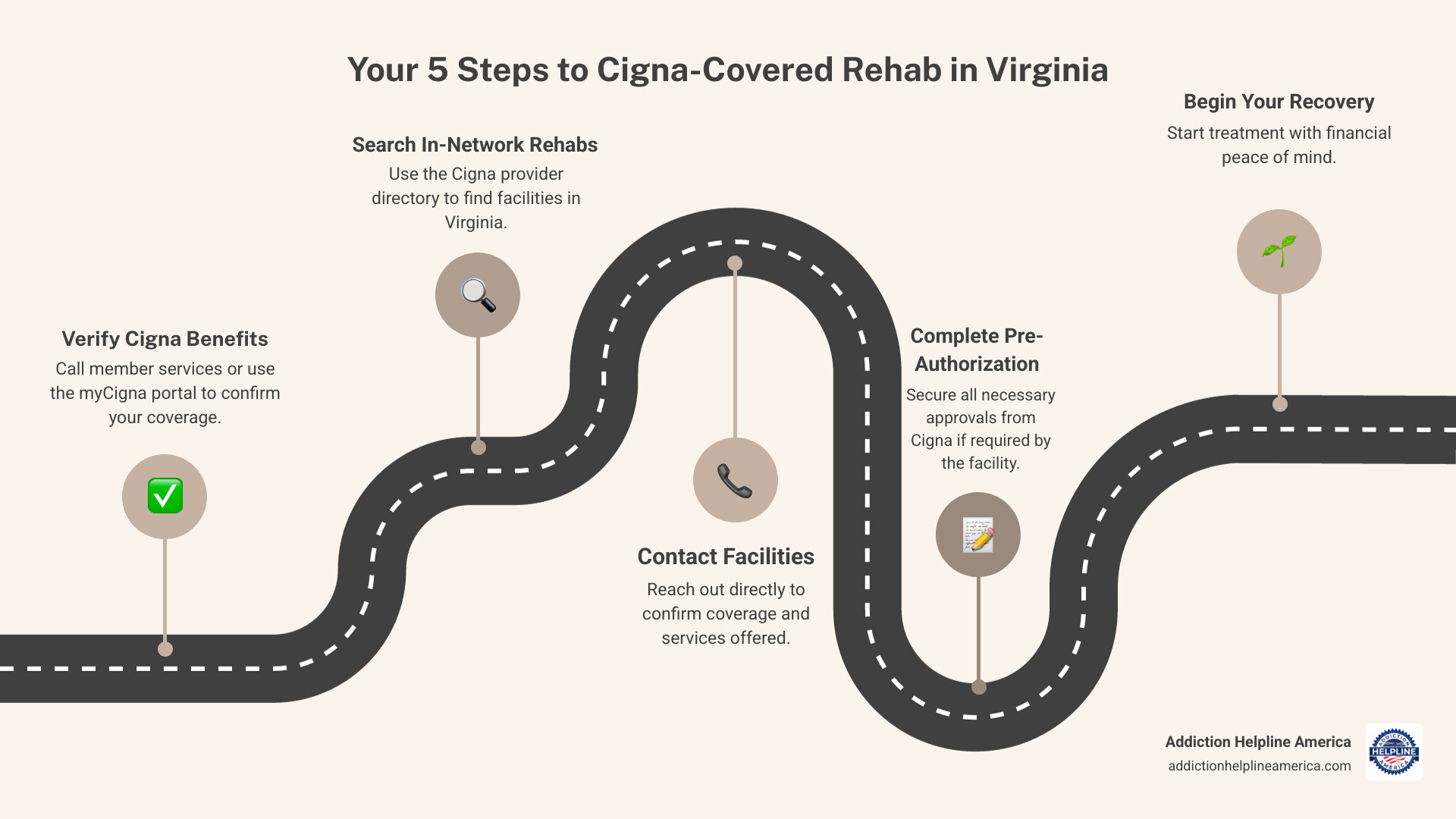
Step 1: Verify Your Cigna Benefits
Before you start calling facilities or browsing directories, you need to understand what your specific Cigna plan covers. Not all plans are identical, and knowing your benefits upfront saves confusion and potential financial surprises later.
The simplest way is to call the number on your ID card. Flip your Cigna card over and look for the member services or behavioral health number. A representative can tell you exactly what addiction treatment services your plan covers, what your deductible is, whether you’ve met it, your copayment or coinsurance amounts, and whether pre-authorization is required.
You can also use the myCigna member portal. If you haven’t set up an online account yet, it’s worth doing. Through your account, you can view your coverage details, check claims, and search for in-network providers—all from your computer or phone.
Here’s another option that many people find easier: ask a treatment center for a confidential verification. Reputable facilities, including those we work with at Addiction Helpline America, offer free insurance verification services. We can contact Cigna on your behalf to determine your exact benefits, explain what you’ll owe, and clarify any authorization requirements. This service is completely confidential and can save you considerable time and stress during an already difficult period.
Step 2: Search for Cigna Insurance In-Network Drug Rehab Facilities in Virginia
Once you understand your coverage, it’s time to find facilities that accept it. The official Cigna provider directory is your primary tool. You can search specifically for substance abuse treatment centers, filter by location—whether you’re looking in Richmond, Norfolk, Virginia Beach, or any other Virginia city—and narrow results by the type of care you need, like inpatient, outpatient, or detox services.
The directory will show you which facilities are in-network, meaning they have contracted rates with Cigna and will result in your lowest out-of-pocket costs. It’s important to confirm this information directly with both the facility and Cigna before making any commitments, as network status can occasionally change.
When you’re researching facilities, look beyond just whether they accept Cigna. Check for accreditation from organizations like The Joint Commission or CARF (Commission on Accreditation of Rehabilitation Facilities). These accreditations aren’t just fancy certificates—they indicate that a facility meets rigorous standards for safety, quality of care, and ethical practices.
Step 3: Choose the Right Facility for Your Needs
Now comes the personal part: finding a facility that’s not just in-network, but truly right for you or your loved one. Consider these important factors as you narrow your choices:
Location matters more than you might think. Some people do better staying close to home where family can visit and provide support. Others find that getting away from their usual environment—away from triggers and old habits—gives them the fresh start they need. There’s no right answer; it depends on your unique situation.
Think about the substances the facility specializes in treating. While most centers treat multiple types of addiction, some have particular expertise with opioids, others with alcohol, and still others with stimulants or prescription drugs. Finding a center experienced with your specific substance can make a real difference in treatment quality.
Look at the therapeutic approaches offered. Does the facility provide evidence-based treatments like CBT, DBT, or MAT? Do they offer holistic therapies like yoga, meditation, or art therapy alongside clinical treatment? The best programs combine proven clinical approaches with supportive therapies that address your whole well-being.
Specialized programs can be crucial for certain populations. If you’re a veteran, you might benefit from a program that understands military culture and service-related trauma. LGBTQ+ individuals often find more comfort and better outcomes in affirming programs designed for their community. Adolescents need age-appropriate treatment that differs significantly from adult programs. If you have co-occurring mental health conditions, seek facilities with expertise in dual diagnosis treatment.
Finally, consider amenities that might support your recovery. While they’re not the most important factor, things like private rooms, quality food, fitness facilities, or even pet-friendly policies can make the challenging work of treatment a bit more manageable. Comfort matters when you’re doing such difficult emotional and psychological work.
At Addiction Helpline America, we understand these nuances personally. We can help you weigh these factors, answer questions about specific Cigna insurance in network drug rehab facilities virginia, and connect you with a program that truly fits your needs and circumstances.
The Admissions Process: From Verification to Your First Day
Once you’ve chosen a facility, the admissions process moves fairly quickly. Understanding what to expect can ease anxiety and help you prepare.
One critical step you need to be aware of is pre-authorization. Many Cigna plans require that the insurance company approve your treatment before you begin, especially for inpatient or residential care. This is called pre-authorization, prior authorization, or precertification—different terms for the same thing. The facility or your doctor submits clinical information to Cigna demonstrating the medical necessity of treatment, and Cigna reviews it and approves (or occasionally denies) coverage. You can learn more about what is preauthorization and why it matters.
Skipping this step can be costly. If you begin treatment without required pre-authorization, Cigna may refuse to pay, leaving you responsible for the full cost. The good news is that most facilities handle this process for you—they’re experienced with insurance requirements and know exactly what documentation Cigna needs.
You’ll work closely with an admissions coordinator from the treatment facility. This person becomes your main point of contact, guiding you through paperwork, gathering medical history, answering questions about the program, and helping with practical matters like transportation to the facility. They’re there to make this transition as smooth as possible.
Your privacy is protected by law. All treatment centers must comply with HIPAA (Health Insurance Portability and Accountability Act), which means they cannot share your healthcare information with anyone without your written permission. Your employer won’t know, your extended family won’t know unless you tell them, and your confidentiality is taken seriously throughout treatment.
As your first day approaches, the facility will provide a list of what to pack for rehab. Generally, you’ll need comfortable, casual clothing, personal toiletries (often alcohol-free versions), any prescribed medications in their original containers, and perhaps some personal items like books, journals, or photos. Most facilities have restrictions on electronics and valuables, so check the specific list carefully. What you really need to bring, though, is an open mind and a willingness to do the work of recovery.
Frequently Asked Questions about Cigna and Virginia Rehab
We hear similar questions from nearly everyone who contacts us about using Cigna for addiction treatment. Here are the answers to what people most want to know:
Does Cigna cover medications for addiction treatment in Virginia?
Yes, and this is important: Cigna plans typically cover medications used in Medication-Assisted Treatment (MAT). These FDA-approved medications—Suboxone, Methadone, and Naltrexone—are proven to reduce cravings, ease withdrawal, and significantly improve recovery outcomes, especially for opioid use disorder.
The specifics of coverage depend on your individual plan. Your plan’s formulary (the list of covered drugs) determines which medications are covered and at what cost to you. Some medications may require prior authorization, and your out-of-pocket cost will depend on your deductible, copayment, or coinsurance.
Cigna provides a helpful tool to check your specific medication coverage: the Cigna “Price a Medication” tool. You can search for specific medications to see if they’re covered, whether they require authorization, and what your estimated cost will be. This transparency helps you plan financially and avoid surprises at the pharmacy.
What is the difference between in-network and out-of-network rehab for Cigna members?
This distinction matters significantly for your wallet. In-network providers have signed contracts with Cigna agreeing to accept negotiated rates for their services. Because of these agreements, Cigna pays a larger portion of the bill, and your out-of-pocket costs—your deductible, copayments, and coinsurance—are lower. The billing is also typically handled directly between the facility and Cigna, making the process smoother for you.
Out-of-network providers have no such agreement with Cigna. They can charge their full rates, and while some Cigna plans (particularly PPOs) may offer partial coverage for out-of-network care, you’ll pay substantially more. You might need to pay the facility upfront and then file a claim with Cigna for reimbursement. Even then, Cigna will only reimburse based on what they consider “usual and customary” rates for your area, which may be less than what the provider actually charged, leaving you to cover the difference.
The bottom line: choosing Cigna insurance in network drug rehab facilities virginia will almost always result in significantly lower costs and less hassle. Always verify network status directly with both the facility and Cigna before you begin treatment to avoid unexpected bills.
How do I find Cigna insurance in-network drug rehab facilities in Virginia if I have an HMO plan?
HMO plans work a bit differently than PPOs, with more restrictions but also more structure. If you have a Cigna HMO, you must use in-network providers—services received out-of-network generally aren’t covered except in true emergencies. This makes finding in-network facilities essential, not optional.
Your HMO plan may also require a referral from your Primary Care Physician (PCP) before you can access addiction treatment services. Not all HMO plans require this, but many do, so check with your PCP and call Cigna to confirm whether a referral is necessary for your specific plan.
The best way to find approved facilities is through the official Cigna provider directory. Filter your search by Virginia, select substance use disorder treatment, and the directory will show you which facilities are in your HMO network. Always confirm this information with both Cigna and the facility before making any commitments, and if a referral is required, make sure you have it in place before beginning treatment.
Take the First Step Towards Recovery Today
Deciding to seek help for addiction is one of the bravest choices you’ll ever make. We know it’s not easy—the fear, the uncertainty, the worry about cost, the concern about what treatment will be like. But here’s what we want you to know: you don’t have to figure this out alone, and with Cigna insurance in network drug rehab facilities virginia, quality treatment is more accessible than you might think.
Cigna offers comprehensive coverage for addiction treatment, backed by federal laws like the Mental Health Parity and Addiction Equity Act and the Affordable Care Act that require insurance companies to treat addiction like any other medical condition. Your plan likely covers everything from medical detox through inpatient treatment, intensive outpatient programs, therapy, and even medications that support recovery. This coverage significantly reduces the financial barrier that keeps too many people from getting help.
Virginia has over 90 facilities that accept Cigna, offering diverse programs, therapeutic approaches, and specialized services to meet different needs. Whether you’re struggling with alcohol, opioids, stimulants, or any other substance—whether you’re dealing with co-occurring mental health conditions or need trauma-informed care—there’s a program designed for your situation.
Finding the right facility involves understanding your specific benefits, searching for in-network providers, and choosing a program that addresses your unique circumstances. It means considering location, treatment approaches, specialized services, and accreditation. It means asking questions and making informed decisions during a time that probably feels chaotic and overwhelming.
That’s exactly why Addiction Helpline America exists. We provide free, confidential, and personalized guidance to help you steer your Cigna benefits and connect with the right treatment program. Our team understands both the insurance landscape and the deeply personal nature of addiction recovery. We’ve helped thousands of people take this step, and we’re ready to help you too.
Your path to recovery starts with a single action. Don’t let confusion about insurance or uncertainty about the process keep you stuck. Reach out today, and let us help you open up your Cigna benefits and begin the healing journey you deserve.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.