Understanding Barbiturate Overdose: A Critical Overview
A barbiturate overdose is a life-threatening medical emergency that occurs when someone takes too much of these powerful sedative drugs. Recognizing the signs early can save a life.
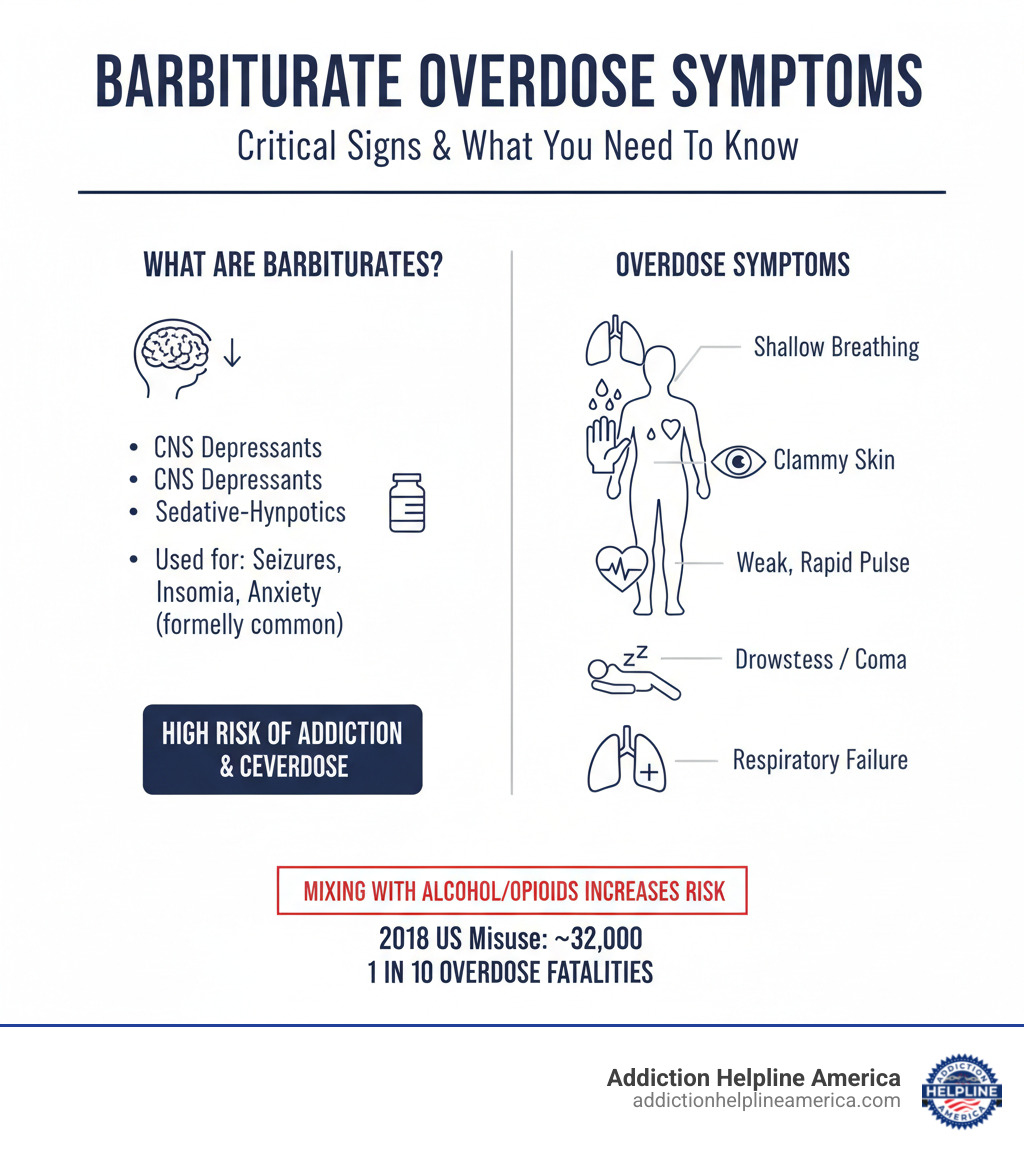
Here are the critical signs of a barbiturate overdose:
- Shallow breathing: Breathing becomes very slow or stops.
- Clammy skin: Skin feels cold and damp.
- Dilated pupils: Pupils look larger than usual.
- Weak, rapid pulse: Heartbeat is fast but faint.
- Drowsiness progressing to coma: The person becomes unresponsive.
- Respiratory failure: The lungs stop working properly.
Barbiturates are central nervous system (CNS) depressants (sedative-hypnotics) once commonly prescribed for seizures, insomnia, and anxiety. Due to their high risk of addiction and overdose, their use has declined, with only a few types like phenobarbital still in use today.
Despite reduced medical use, barbiturates remain a significant danger. Their narrow therapeutic index means a small dose increase can lead to toxicity, a risk that skyrockets when mixed with other depressants like alcohol or opioids. In 2018, about 32,000 Americans aged 12 and older reported misusing barbiturates. Tragically, around 1 in 10 people who overdose on barbiturates or mixtures containing them will die, often from heart and lung problems. Recent Australian data also shows two-thirds of barbiturate toxicity hospitalizations are related to suicide attempts.
At Addiction Helpline America, we’ve seen the devastating impact of barbiturate overdose and addiction. Our team of experienced specialists is dedicated to guiding individuals and families through these challenging times.
What Are Barbiturates and How Do They Work?
Barbiturates are a class of medicines in the central nervous system (CNS) depressant category. Think of them as “slow-down” drugs. Also known as sedative-hypnotics, they can help you relax, ease anxiety, and even make you sleep. But how do these powerful substances create such a strong impact on our bodies and minds?
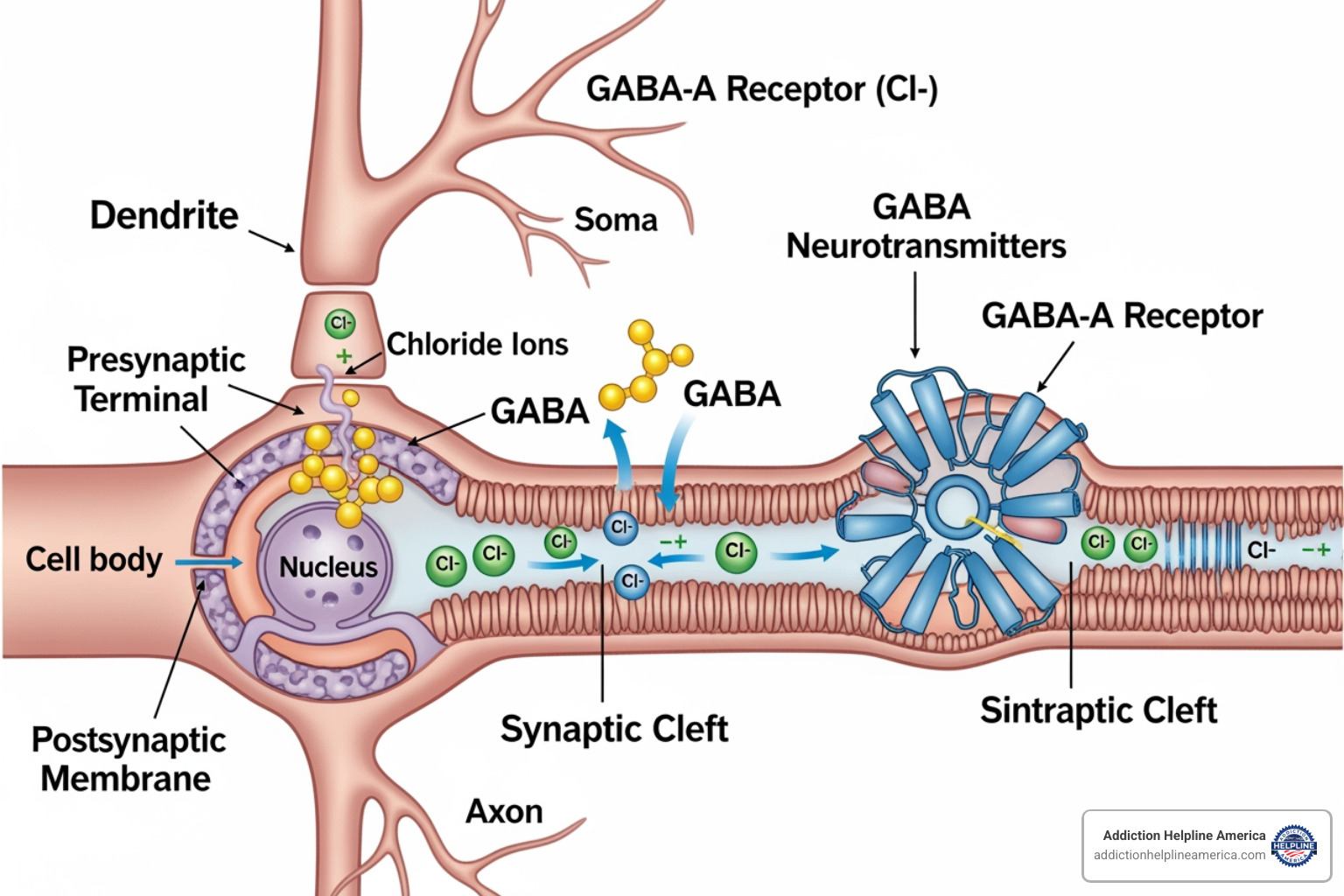
The secret behind barbiturates lies in how they talk to your brain. Your brain uses tiny chemical messengers called neurotransmitters to send signals. One very important messenger is called GABA (gamma-aminobutyric acid). GABA’s job is to slow things down in the brain. Barbiturates step in and make GABA even more effective. They do this by attaching to specific spots on your brain cells called GABA-A receptors. When a barbiturate connects to this receptor, it opens a tiny gate that lets more negatively charged particles (chloride ions) rush into the cell. This makes the brain cell less likely to fire off signals. The end result? A general calming effect and a slowdown of brain activity, leading to that sedative and sleep-inducing feeling.
It’s important to know that while barbiturates quiet the brain, they do so differently than another common group of depressants: benzodiazepines (like Valium or Xanax). Both types of drugs work on those GABA-A receptors, but barbiturates keep the chloride gates open for longer, while benzodiazepines make them open more often. This might sound like a small detail, but it’s a big deal when it comes to safety! That’s why benzodiazepines are often seen as safer and have largely taken the place of barbiturates in many medical uses.
| Feature | Barbiturates | Benzodiazepines |
|---|---|---|
| Mechanism | Increase duration of chloride channel opening | Increase frequency of chloride channel opening |
| GABA-A Receptor | Bind to distinct sites, improve GABA efficacy | Bind to distinct sites, improve GABA potency |
| CNS Depression | Potent, dose-dependent, can lead to profound depression | Generally less profound, safer therapeutic index |
| Overdose Risk | High, narrow therapeutic index, severe respiratory depression | Lower, wider therapeutic index, less severe respiratory depression alone |
| Addiction/Dependence | High risk, severe withdrawal symptoms | Moderate risk, significant withdrawal symptoms |
Medical and Non-Medical Uses
Long ago, barbiturates were considered groundbreaking medications. Doctors used them for all sorts of reasons. Medically, they were prescribed to:
- Help treat seizure disorders, with drugs like phenobarbital being a longtime choice.
- Calm insomnia (trouble sleeping), though we now have safer options.
- Reduce anxiety before surgery.
- Help induce anesthesia for operations.
- In very critical cases, induce a coma to protect the brain, for example, when there’s too much pressure inside the skull.
However, over time, we learned more about the serious downsides of barbiturates. Their high risk of addiction and the danger of barbiturate overdose meant that their medical use has greatly decreased.
Despite less use in hospitals and clinics, some people still misuse barbiturates. They might seek them out for a powerful “high,” or to try and self-medicate feelings of anxiety or stress. This non-medical use is very risky and leads to many cases of barbiturate overdose. As important scientific research on sedative misuse shows, the abuse of prescription sedatives, including barbiturates, remains a serious health problem.
Common Types of Barbiturates
Not all barbiturates are the same! They come in different varieties, and each one works for a different amount of time. Knowing this is key, as it changes how quickly you’d feel their effects and how long they might stay in your system. This also affects how likely they are to be misused or lead to an barbiturate overdose.
Here are some of the more common types you might hear about:
- Phenobarbital: This is a long-acting type, often used for seizures.
- Amobarbital: An intermediate-acting barbiturate.
- Secobarbital: This one is short-acting.
- Butalbital: You might find this in some combination pain medications.
- Pentobarbital: Another intermediate-acting type, sometimes used in hospitals for specific needs.
We often group barbiturates by how long their effects last:
- Long-acting: These can stay in your system for more than 40 hours. Phenobarbital is a good example.
- Short-acting and intermediate-acting: These work much faster and don’t last as long, usually less than 40 hours. Because they get into your brain quickly, they tend to have a more rapid and intense effect.
Recognizing a Barbiturate Overdose: Signs, Symptoms, and Dangers
Understanding how to recognize a barbiturate overdose is incredibly important because it’s a life-threatening emergency that needs immediate help. Barbiturates are tricky drugs because they have what’s called a “narrow therapeutic index.” This simply means there’s only a tiny difference between a dose that helps you and a dose that can be toxic, or even deadly.
This inherent danger, along with how easily someone can become addicted and quickly build up a tolerance, makes barbiturates very risky. When someone uses these drugs regularly, their body starts to get used to the effects. They might need more and more to feel the same way they did before. This is tolerance. But here’s the critical part: while tolerance to the drug’s “feel-good” effects grows, tolerance to its deadly effects, like slowing down your breathing, doesn’t grow as quickly. This gap dramatically increases the chance of an accidental barbiturate overdose.
From Intoxication to Overdose
It’s helpful to understand the journey from simply taking too much (intoxication) to a full-blown, life-threatening barbiturate overdose.
When someone is just intoxicated by barbiturates – meaning they’ve taken more than they should, but not necessarily a lethal amount – you might notice several signs. They could seem quite drowsy or have slurred speech, almost like they’ve had too much to drink. Their movements might be clumsy or poorly coordinated, leading to stumbling or a wobbly walk. You might also notice their judgment isn’t quite right, and they could even become irritable or combative. Sometimes, their eyes might make rapid, involuntary movements (called nystagmus), and they might feel dizzy or have vertigo.
As the dose gets higher, or if the person is very sensitive to the drug, these signs can quickly get much worse and turn into a severe barbiturate overdose. At this critical stage, their level of consciousness changes, ranging from being very confused and difficult to wake up (stupor) to being completely unresponsive (a profound coma). Their breathing becomes dangerously shallow or even stops altogether – this is often the most dangerous symptom and can lead to death. Their heart might beat very weakly and rapidly, struggling to pump blood, which can lead to shock. You might also notice their pupils are dilated and don’t react to light. Their skin can feel cold, pale, and damp (clammy skin), and their body temperature might drop dangerously low (hypothermia). In severe cases, you might even see barbiturate blisters, which are specific blister-like spots on the skin, often at pressure points like the hands or knees. The body’s systems can shut down, leading to respiratory failure (when the lungs stop working) and cardiovascular collapse (when the heart and blood vessels fail).
The Compounded Risk of Polydrug Use
The dangers of a barbiturate overdose become far, far greater when these drugs are mixed with other substances that also slow down the central nervous system. This practice, known as “polydrug use,” is a very common and tragic factor in serious overdoses and deaths.
Barbiturates create what we call “additive effects” when combined with other depressants. This means their individual sedative powers don’t just add up; they multiply, making the effects much more intense and dangerous.
Here are some common substances that are incredibly dangerous to mix with barbiturates:
- Alcohol: Alcohol is also a powerful CNS depressant. When you combine barbiturates with alcohol, the sedative effects are severely amplified. This can lead to profound respiratory depression and coma at doses much lower than if either drug were taken alone. Many overdoses involve a mix of substances, and alcohol is a frequent co-ingestant.
- Opioids: Drugs like heroin, fentanyl, and prescription painkillers (such as oxycodone) are also depressants, especially affecting your breathing. Mixing them with barbiturates sends the risk of fatal respiratory arrest soaring.
- Benzodiazepines: While chemically different, benzodiazepines (like Xanax or Valium) are also sedative-hypnotics. Using them together with barbiturates can lead to extremely dangerous levels of CNS and respiratory depression.
Combining barbiturates with alcohol, opioids, or benzodiazepines is extremely risky. These combinations worsen each other’s depressive effects on the brain, heart, and lungs, making a deadly outcome far more likely.
Emergency Response and Medical Treatment
When facing a barbiturate overdose, every moment counts. This is a life-threatening situation that demands immediate action. Unlike some other types of overdoses, there is no specific “antidote” to reverse the effects of barbiturates. This means medical treatment focuses on “supportive care.” The goal is to keep the person’s body functioning, especially their breathing and circulation, while their system works to eliminate the drug.
Immediate Steps for a Suspected Barbiturate Overdose
If you ever find yourself suspecting a barbiturate overdose, your swift actions can make all the difference. Here’s what you need to do right away:
First and foremost, call 911 immediately. Please don’t hesitate. When you call, try to have as much information as possible ready for the operator. Things like the person’s age, what they took (if you know the name and strength), how much they swallowed, and when it happened are all incredibly helpful. Even if you don’t have every detail, still call! Getting professional help on the way is the most critical step.
While waiting for help to arrive, quickly check for breathing and pulse. If the person isn’t breathing or you can’t find a pulse, the 911 operator will guide you through what to do, which might include performing CPR. If they are unconscious but still breathing, gently place them in the recovery position. This means rolling them onto their side. It’s a simple move that can prevent them from choking if they vomit. Whatever you do, do not try to make them vomit. This can be incredibly dangerous, especially if their consciousness is lowered, as they could inhale the vomit into their lungs. Once first responders arrive, provide them with all the information you’ve gathered. Every piece of information helps them provide the best possible care.
For more detailed information on what to do in an overdose situation, reputable resources like MedlinePlus offer valuable guidance.
In-Hospital Treatment and Management
Once someone experiencing a barbiturate overdose arrives at the hospital, the medical team immediately shifts into high gear to stabilize their condition. The focus remains squarely on comprehensive supportive care.
Their first priority is always the ABCs: Airway, Breathing, and Circulation. If the person’s breathing is too shallow or has stopped, doctors will secure their airway, often by placing a tube down their windpipe (called intubation), and connect them to a machine that breathes for them (mechanical ventilation). To support blood pressure and prevent the body from going into shock, they’ll also administer intravenous (IV) fluids and sometimes medications called vasopressors.
Another tool doctors might use is activated charcoal. If given early enough, especially for longer-acting barbiturates, this charcoal can bind to the drug in the stomach and intestines, stopping it from being absorbed into the bloodstream. Sometimes, multiple doses are needed. For very severe cases, doctors might turn to more advanced methods to help the body get rid of the drug faster. One powerful technique is hemodialysis, which acts like an artificial kidney to filter the blood and remove the barbiturates. While other methods like urinary alkalinization were once used, they’re generally not recommended anymore for barbiturate toxicity due to being less effective and having potential risks. Beyond these, medical teams will address any other symptoms that arise, such as dangerously low body temperature (hypothermia) or imbalances in the body’s chemicals.
If you or someone you care about is struggling with barbiturate misuse, getting professional help is a vital step toward recovery. Our network includes many compassionate Medical Detox Centers Near Me that are ready to provide the medically supervised support needed during this challenging time.
Beyond the Crisis: Withdrawal, Recovery, and Prevention
Surviving a barbiturate overdose is an incredibly brave and crucial first step on a much longer journey. While the immediate danger might be over, the path to lasting recovery stretches far beyond that emergency room. Barbiturates are truly tricky customers; they lead to both physical dependence (where your body gets used to the drug) and psychological addiction (where your mind craves its effects). Understanding both sides of this challenge is key to finding your way to long-term healing. If you’re curious to learn more about how addiction works, we encourage you to explore the Signs and Symptoms of Addiction.
The Dangers of Barbiturate Withdrawal
Here’s the tough truth: stopping barbiturates cold turkey can be incredibly dangerous. It’s not just uncomfortable; it can be life-threatening if you try it without medical help. For those who’ve used barbiturates regularly, severe withdrawal symptoms can kick in surprisingly fast—sometimes within just 8 to 15 hours after the last dose.
Imagine feeling incredibly agitated and restless, with your heart pounding from profound anxiety and even panic attacks. Your hands might start to shake with tremors, and sleep becomes a distant dream, replaced by insomnia and nightmares. Other tough symptoms include a high body temperature, sweating, nausea, and vomiting. But the really scary part? The risk of potentially life-threatening seizures. These grand mal seizures often show up between the third and seventh day of withdrawal. And to top it off, some people experience delirium, a severe state of confusion and disorientation, usually starting between the fourth and sixth day.
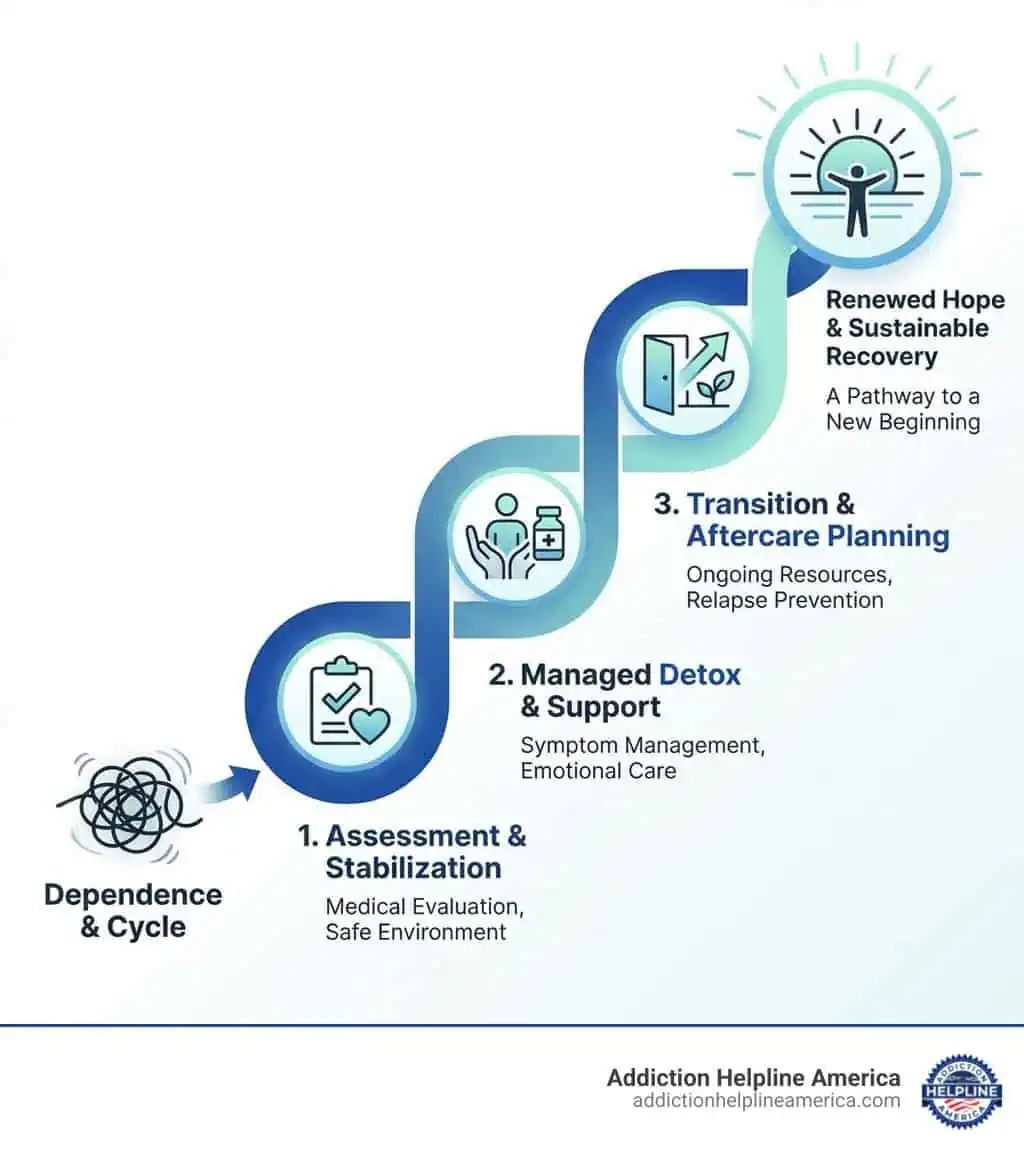
Because of these serious risks, especially seizures, barbiturate withdrawal absolutely needs to happen in a medically supervised detox setting. This isn’t just about comfort; it’s about safety. Here, you’ll have 24-hour monitoring and medical support to help you through this challenging period safely.
Long-Term Treatment and Prevention
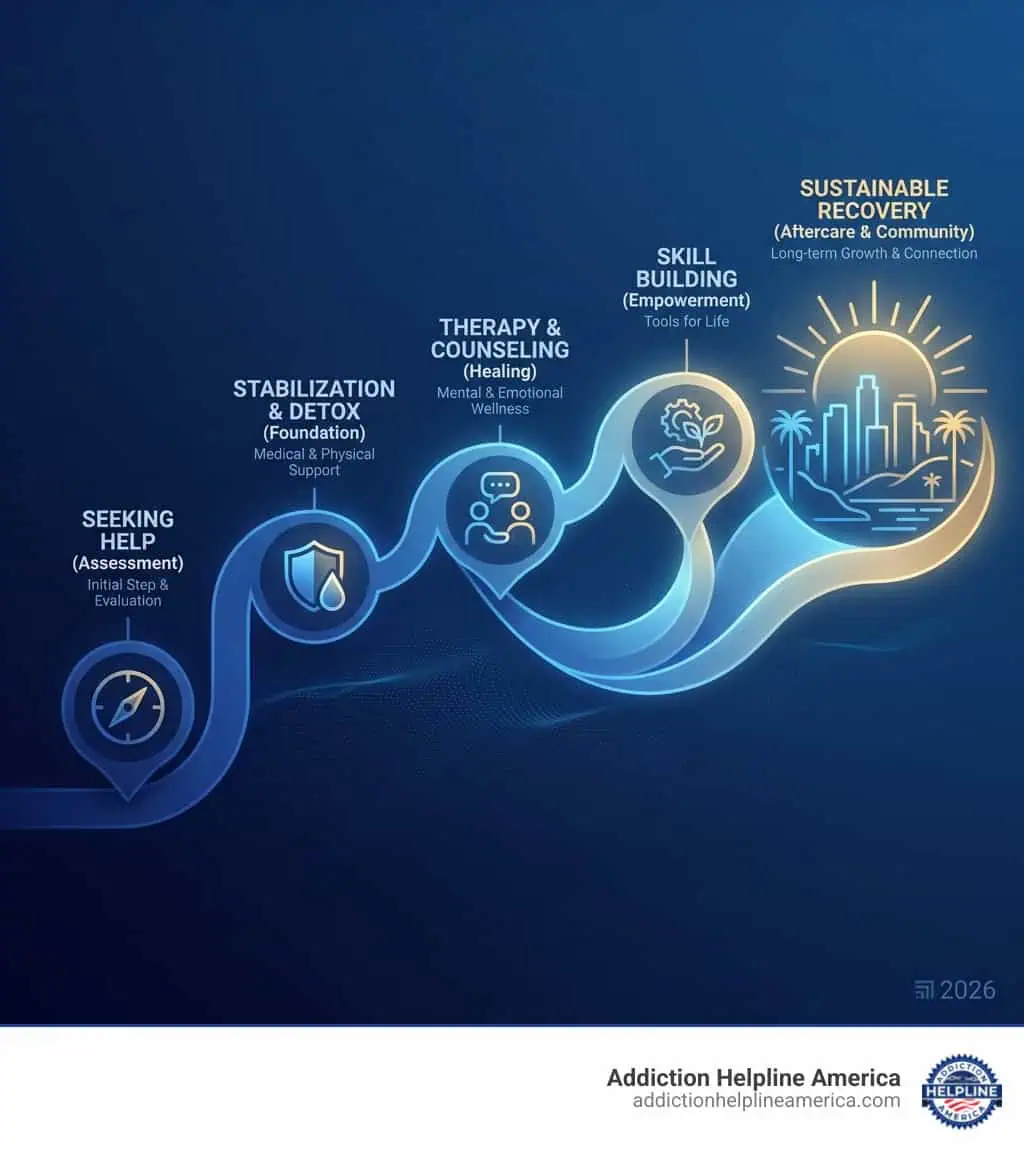
Getting back on your feet and staying sober after a barbiturate overdose and dependence requires a thoughtful, ongoing plan. It’s not a quick fix, but a journey with many supportive stops along the way.
First up in a medical detox is often tapering dosages. This means doctors slowly reduce the amount of barbiturate you take over time. Sometimes, they’ll switch you to a longer-acting barbiturate like phenobarbital. This helps make the withdrawal process smoother and safer, reducing those uncomfortable ups and downs.
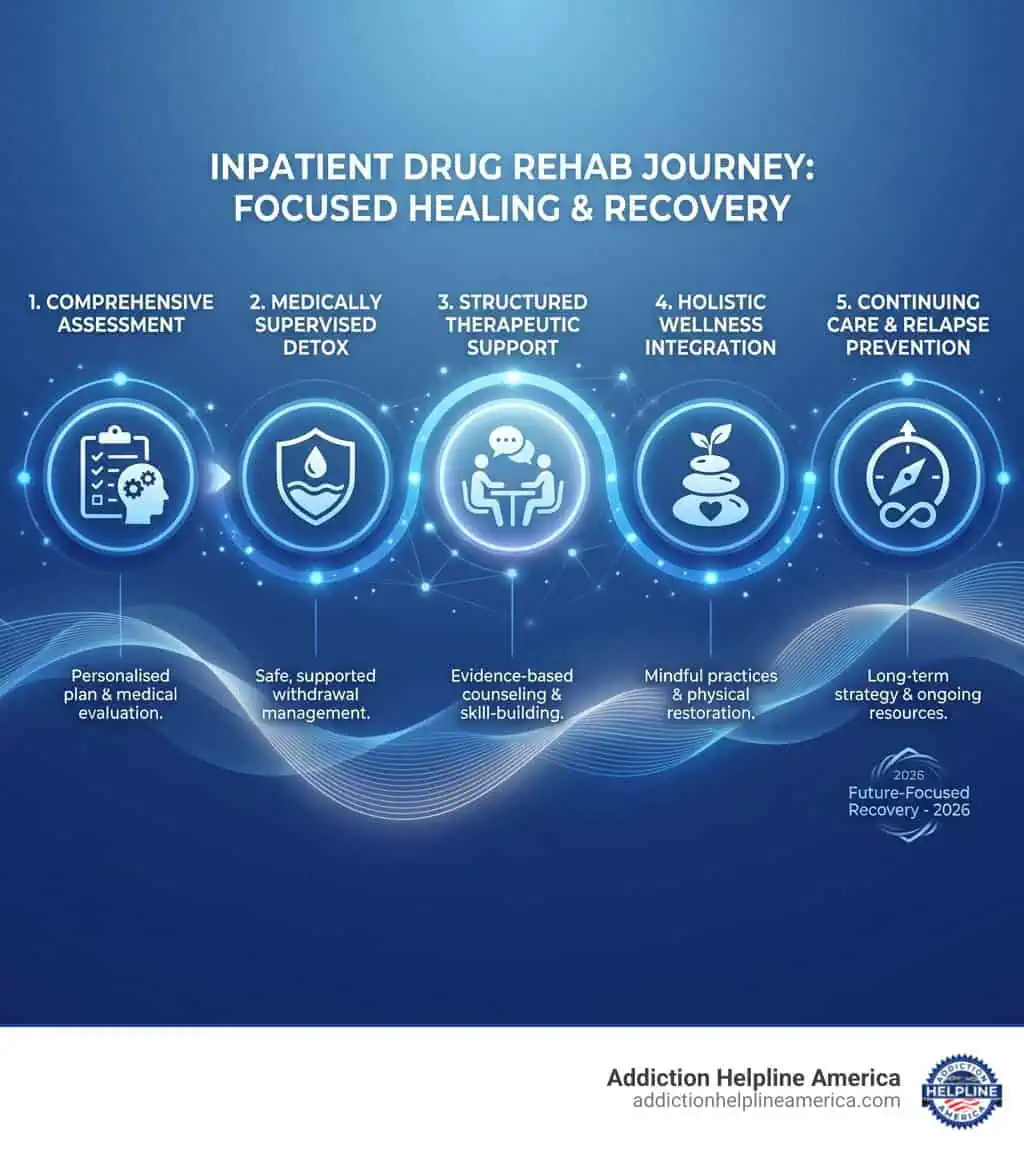
After detox, many people find incredible support in structured Inpatient Rehab Programs Complete Guide. These programs offer around-the-clock care in a safe environment, along with intensive therapy designed just for you. Here, you can dive into effective approaches like Cognitive Behavioral Therapy (CBT), which helps you spot and change unhelpful thought patterns and behaviors that might have led to drug use. Another helpful tool is Contingency Management (CM), which uses positive rewards to encourage healthy, sober choices.
Don’t underestimate the power of connection! Support groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) offer a wonderful community where you can share experiences and find strength with others who understand what you’re going through.
On a broader scale, there are also important prevention strategies in place to help reduce barbiturate overdose and misuse. For instance, Prescription Drug Monitoring Programs (PDMPs) are state databases that track controlled substances. These help stop “doctor shopping” and ensure safer prescribing. Public health education also plays a huge role, teaching both doctors and the public about the real risks tied to barbiturates. And let’s not forget strict regulations, like the Controlled Substances Act, which have greatly tightened control over these powerful medications. These measures all work together to make our communities safer.
Frequently Asked Questions about Barbiturate Overdose
It’s natural to have questions about a topic as serious as barbiturate overdose. We’re here to provide clear, compassionate answers to some of the most common inquiries, helping you understand this critical issue better.
Can naloxone (Narcan) reverse a barbiturate overdose?
This is a really important question, and understand the answer clearly. No, naloxone (Narcan) cannot reverse a barbiturate overdose on its own. Naloxone is a fantastic medication, but it’s specifically designed to be an opioid antagonist. Think of it like a very specific key that only open ups opioid receptors in the brain, blocking the effects of drugs like heroin, fentanyl, or prescription painkillers.
Barbiturates, however, work in a completely different way, by interacting with GABA receptors in your brain. Because their mechanism of action is so distinct from opioids, naloxone simply won’t have any effect on a barbiturate overdose if barbiturates are the only drug involved.
Now, here’s where it can get a little tricky: if someone has taken both barbiturates and opioids, then naloxone might be given. In that situation, it would help reverse the dangerous effects of the opioids, particularly the slowed breathing. But please remember, even if naloxone helps with an opioid component, it won’t touch the barbiturate effects. For a pure barbiturate overdose, the focus remains on essential supportive care to help the body recover.
How deadly is a barbiturate overdose?
To put it simply, a barbiturate overdose can be incredibly deadly. These powerful medications have a very narrow window between a therapeutic dose and a toxic one, making them inherently risky. Our research and clinical experience sadly show that about 1 in 10 people who overdose on barbiturates, or a mixture including them, will not survive.
The main reasons for these tragic outcomes often involve severe problems with the heart and lungs, most notably profound respiratory depression, which means breathing becomes too slow or stops altogether. Even with the best possible medical care in a hospital, the mortality rate for barbiturate overdose still ranges from 0.5% to 2%.
Beyond the immediate risk to life, a severe barbiturate overdose can lead to serious, long-lasting complications. These can include:
- Aspiration pneumonia: This happens if someone vomits and accidentally inhales the contents into their lungs.
- Myocardial infarction: A heart attack, as the body struggles under the strain.
- Cerebral edema: Swelling of the brain, which is incredibly dangerous.
- Pulmonary edema: Fluid buildup in the lungs, making breathing even harder.
- Multiorgan failure: When several vital organs begin to shut down.
- Prolonged coma: A state of deep unconsciousness that can last for an extended period.
- Permanent brain damage: Caused by a lack of oxygen to the brain during the overdose.
These severe consequences highlight just how critical it is to get immediate medical help if you suspect a barbiturate overdose.
Why are barbiturates prescribed less often today?
If you’re wondering why you don’t hear about barbiturates being prescribed as much as they used to be, there are several very good reasons for this significant shift in medical practice.
The biggest factor was the development of safer alternatives. In the 1960s, a new class of drugs called benzodiazepines (think Valium or Xanax) came onto the scene. These medications offered similar sedative and anxiety-reducing effects to barbiturates but with a much wider “therapeutic index.” This means there’s a much larger gap between an effective dose and a dangerous, toxic dose, making them considerably safer in overdose situations.
Another major concern with barbiturates is their high risk of dependence and overdose. Their narrow therapeutic window means that even a slightly higher dose than prescribed can quickly become life-threatening. This inherent danger made them a less desirable choice for routine treatment.
The severe withdrawal symptoms associated with barbiturates also played a huge role. As we’ve discussed, stopping barbiturates can be not only incredibly uncomfortable but also medically complex and potentially fatal, requiring intensive medical supervision. This made them a difficult drug to manage long-term.
Finally, strict regulations were put in place as the medical community and public became more aware of their dangers. Laws like the Controlled Substances Act significantly tightened control over how barbiturates could be prescribed and accessed. This was a direct response to a worrying trend; for instance, sales of barbiturates soared from 100 tons in 1939 to a staggering 2000 tons by the mid-1960s, fueling a growing crisis.
So, while a few barbiturates like phenobarbital still have specific, limited uses (like treating certain seizure disorders), their widespread use has largely been replaced by drugs that offer a much better safety profile.
Finding Help and Hope for Barbiturate Addiction
When it comes to a barbiturate overdose, remember this: it’s a medical emergency that needs help right away. If you or someone you know shows signs of an overdose, please don’t wait. Call 911 immediately. Getting help fast can truly save a life.
Beyond that immediate crisis, there’s a path forward. Recovery from barbiturate addiction is absolutely possible. It takes courage, but with professional help and a real commitment to getting better, a healthier future is within reach.
One of the most important steps in this journey is medically supervised detox. Because barbiturate withdrawal can be so severe, even deadly, trying to quit on your own is incredibly risky. A safe, controlled environment where medical professionals can look after you around the clock is not just a good idea—it’s essential for your safety and well-being.
At Addiction Helpline America, we truly understand how overwhelming barbiturate addiction and the fear of overdose can feel. We’re here to offer a helping hand, providing free, confidential, and personalized guidance. Think of us as your friendly guide, connecting you to the right recovery program from our large network of treatment centers all across the United States. Whether you’re in California, Florida, Texas, New York, or anywhere else, we can help you find support nearby.
Our goal is to ensure you find a program that treats the whole person. This means getting help that looks after both your body’s needs during detox and recovery, and your mind’s journey to overcome addiction. We believe in a comprehensive approach that addresses all aspects of addiction, paving the way for lasting sobriety and a much brighter future.
If you’re ready to take that crucial next step towards recovery, we’re here to help you get started. You can easily Find a barbiturate inpatient rehab program through us. You don’t have to face this challenge alone—we’re here to support you every step of the way.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.