Medicaid and Your Path to Recovery
Facing a substance use disorder (SUD) is incredibly tough. Millions of Americans, including those enrolled in Medicaid, struggle with addiction every day. The good news is that Medicaid covers drug & alcohol rehab for many. This can be a game-changer for those seeking help.
- Yes, Medicaid generally covers drug and alcohol rehab.
- Coverage includes various treatment types, from detox to outpatient care.
- The specifics of coverage can vary by state and individual plan.
- Medicaid is a vital resource for affordable addiction treatment.
Finding affordable and effective treatment is a major concern. Medicaid is a key resource. It helps people access necessary care without huge costs. Thanks to laws like the Affordable Care Act (ACA), Medicaid now plays a bigger role than ever. It ensures that addiction treatment is covered, similar to other medical care. This guide will walk you through how Medicaid can support your recovery journey. We will cover what’s included and how to find the right help.
At Addiction Helpline America, we understand the complexities of Does Medicaid Cover Drug & Alcohol Rehab? and have guided countless individuals toward recovery. Our team of experienced professionals is dedicated to providing compassionate, confidential support and connecting you with vital resources for your journey.
What Addiction Treatments Are Covered by Medicaid?
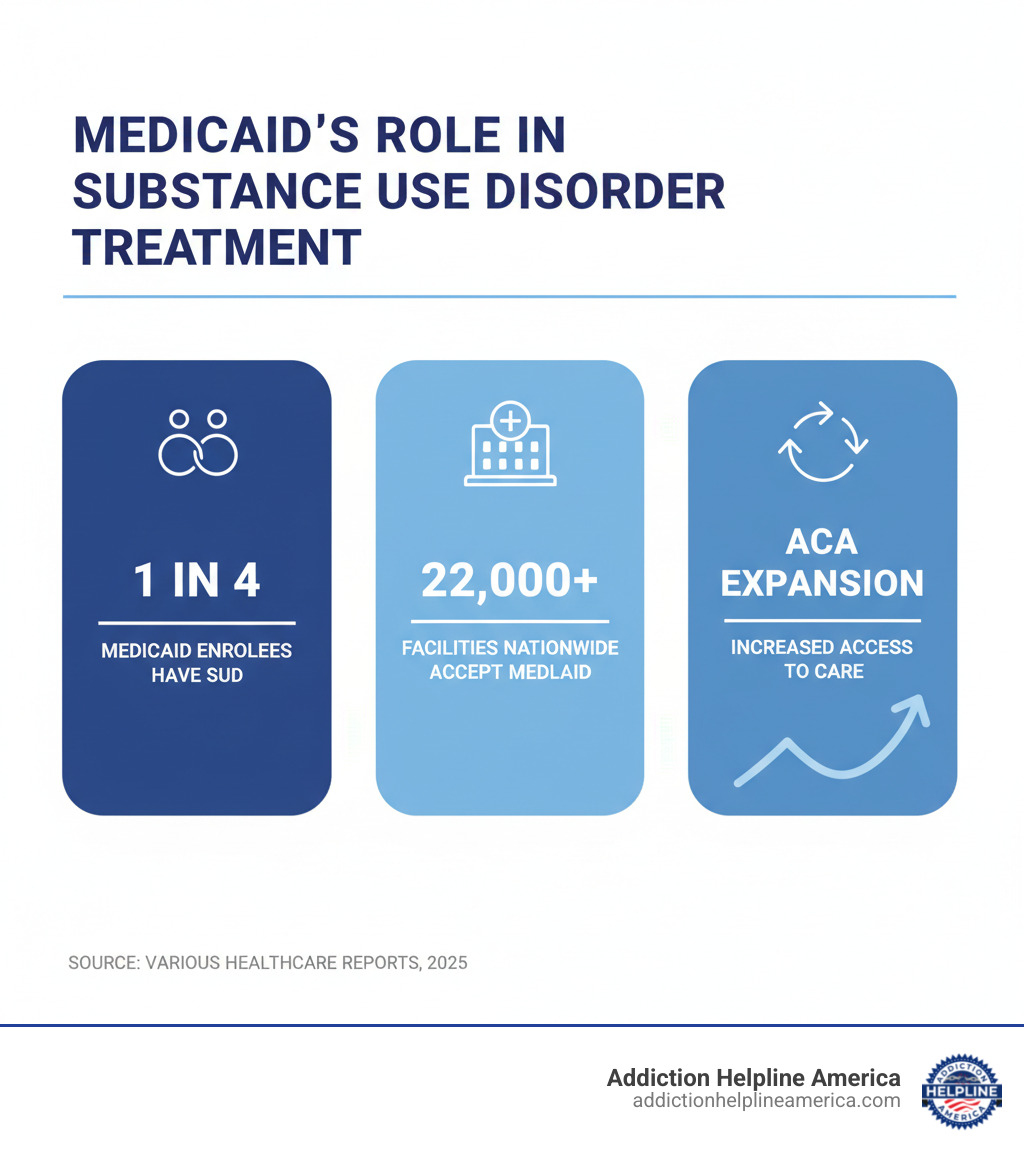
It’s wonderful news that Medicaid is such a powerful force for good in recovery. In fact, it’s the largest single supporter of behavioral health services in the United States! This means millions of people struggling with mental health conditions and substance use disorders (SUDs) can find the help they need. Thanks to the Affordable Care Act (ACA) back in 2010, addiction treatment services are now considered an “essential health benefit.” This means Medicaid, just like other insurance plans, must cover the basic steps toward recovery from drug and alcohol dependency. It’s been a game-changer, opening doors to care for so many.
Medicaid covers a really wide range of services for both mental health (MH) and SUDs – often even more than what other health care programs might include. While the exact services can differ a bit from state to state, federal rules make sure there’s always a comprehensive approach to treatment. At its heart, Medicaid coverage for addiction treatment is guided by “medical necessity.” This simply means that a healthcare professional needs to agree that the services are necessary for you to get better. So, when you ask, Does Medicaid Cover Drug & Alcohol Rehab? The answer is yes, for medically necessary treatment across a full “continuum of care,” offering different “levels of care” as your recovery journey unfolds.
To dive deeper into the many behavioral health services covered, you can always visit Medicaid’s official page on behavioral health services.
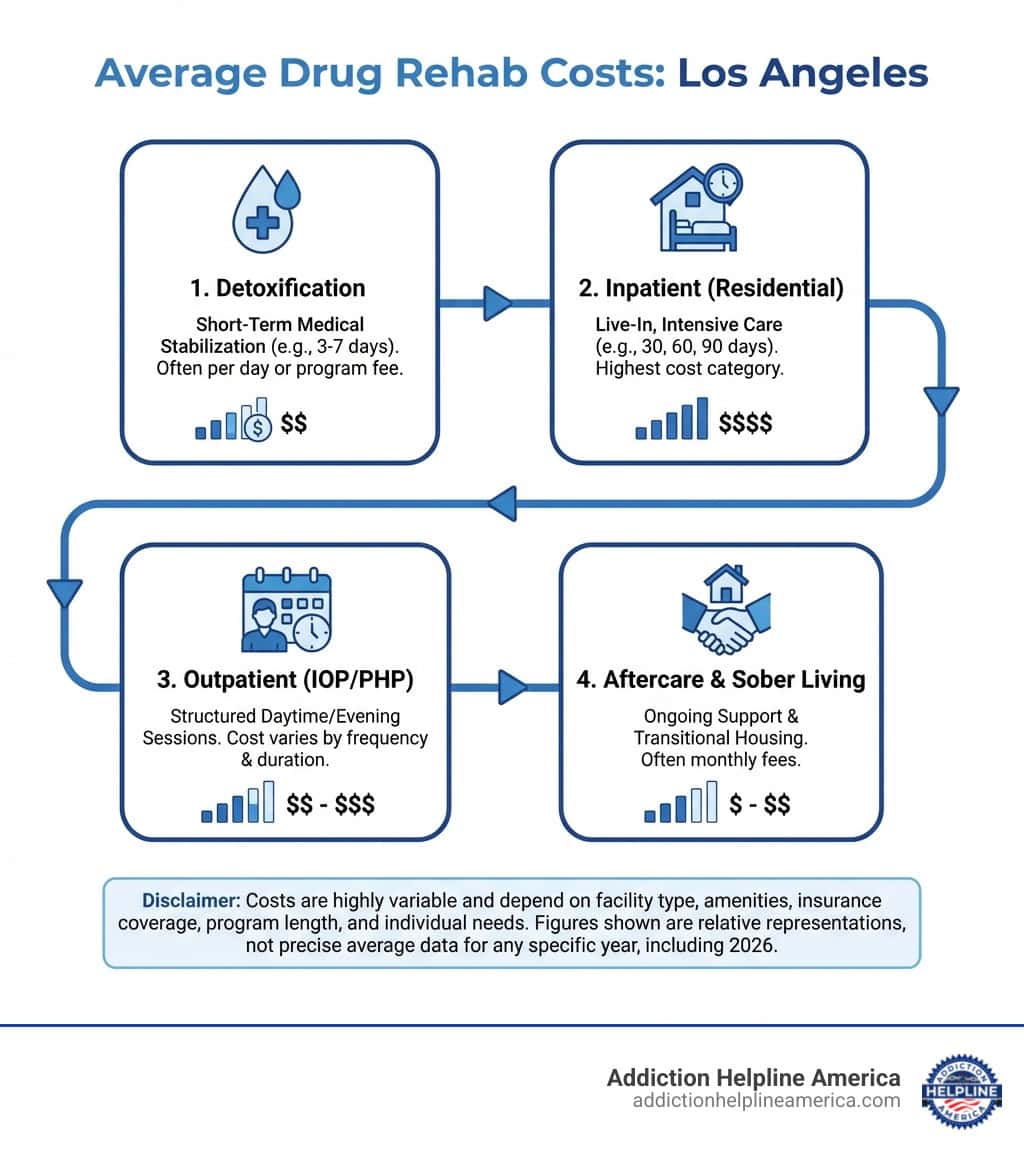
Detoxification (Detox) Services
Taking the first step toward recovery can feel daunting, and often, that first step is detoxification (detox). This is a critical stage where your body safely processes and removes substances after you stop using them. It’s all about managing the physical withdrawal symptoms that can occur. Medicaid generally steps up to cover these essential detox services in most states.
This crucial care can include:
- Medically Supervised Detox: Imagine having medical professionals right there, 24/7, making sure you’re safe and as comfortable as possible during withdrawal. They’re there to monitor you and help manage any severe symptoms.
- Withdrawal Symptom Management: This focuses on easing those often painful or even dangerous symptoms that pop up when you stop using substances like alcohol or opioids.
- Inpatient Detox: This is like a safe haven, often in a hospital or a special facility, where you get the highest level of care and constant supervision.
- Outpatient Detox: If your withdrawal symptoms aren’t too severe and you have a stable, supportive home environment, this option lets you live at home while attending regular medical appointments. It offers flexibility while still providing vital support.
For even more detailed information on detox, we invite you to explore our drug detox treatment centers guide and learn more about alcohol withdrawal symptoms.
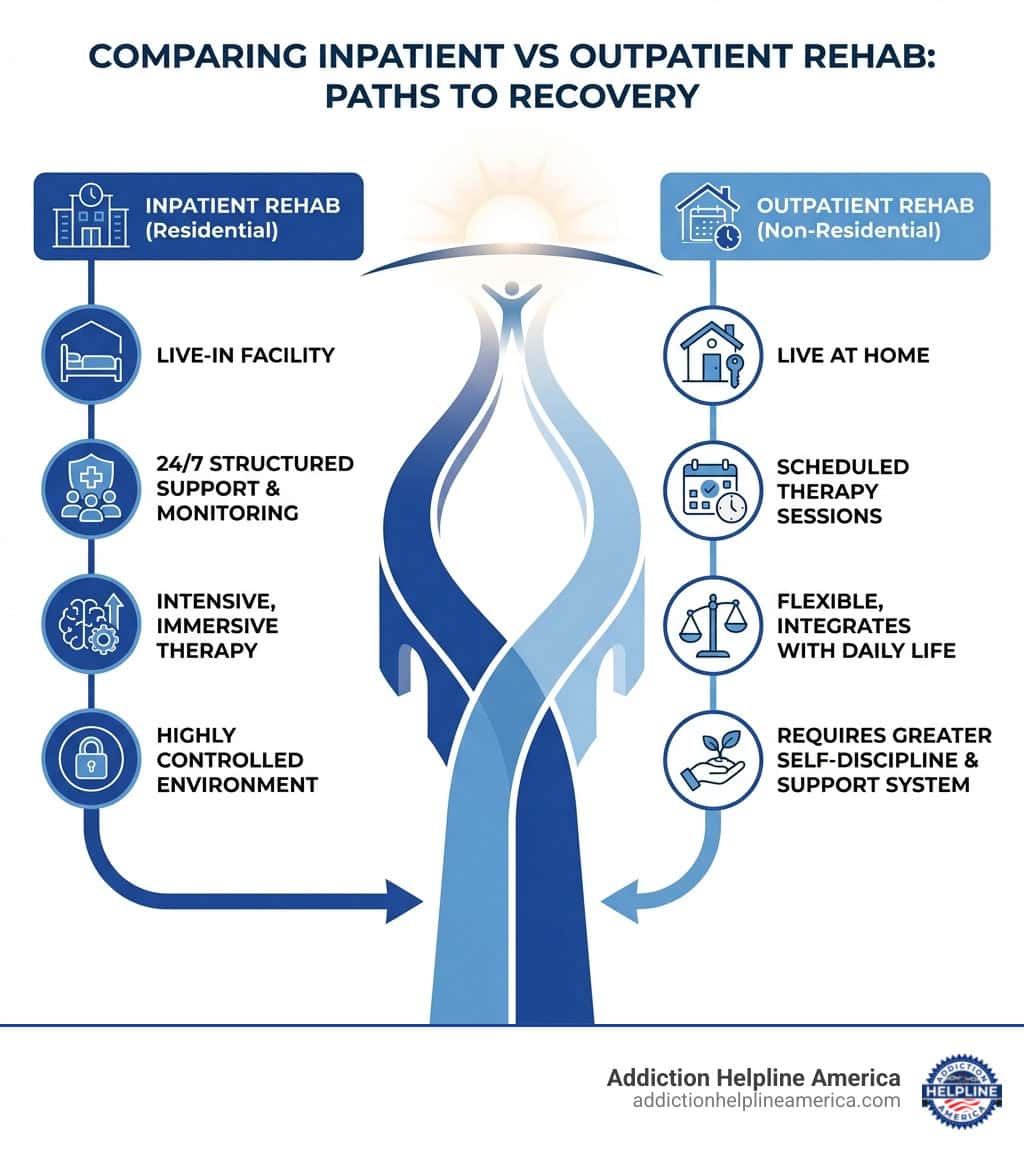
Inpatient and Residential Rehab
Once you’ve completed detox, or if detox isn’t medically necessary for your situation, many people find incredible support in inpatient or residential rehab. Think of these programs as a dedicated time-out from daily life, giving you a structured, supportive environment away from triggers and temptations. Here, you can focus completely on healing with intensive therapy and round-the-clock support.
These programs typically offer:
- 24/7 Medical Care and Supervision: While it’s not as intense as detox, inpatient programs often have medical staff on hand to help with any health needs that arise.
- Structured Environment: Days are filled with purpose, including scheduled therapy, counseling, educational sessions, and even recreational activities. It’s a routine designed to help you build healthy habits.
- Short-Term Rehab: These programs often last around 30 days and provide an intensive introduction to the principles of recovery. If you’re curious, check out our guide to 30-day inpatient programs.
- Long-Term Residential Treatment: For those who need more time to heal and explore deeper issues, these programs can last 60, 90 days, or even longer, offering extended support and a more profound journey into recovery.
It’s important to know that while Medicaid covers drug & alcohol rehab in these settings, the specifics can vary by state. For instance, some states might have limitations on residential care coverage. That’s why it’s always a good idea to verify your specific state’s benefits. If you’re also exploring budget-friendly options, our information on free inpatient rehab might offer some helpful insights.
Outpatient and Virtual Rehab Programs
For many people, balancing recovery with daily life commitments is key. That’s where outpatient and virtual rehab programs shine! These options offer incredible flexibility, allowing you to live at home, keep up with work, school, or family responsibilities, all while attending scheduled therapy sessions and treatment activities.
Medicaid generally covers a variety of these flexible options, including:
- Partial Hospitalization Programs (PHP): Sometimes called “day treatment,” PHPs offer intensive therapy for several hours a day, multiple days a week. It’s like getting inpatient-level care without having to stay overnight.
- Intensive Outpatient Programs (IOP): A step down from PHP, IOPs are still very structured but involve fewer hours of therapy each week, often a few hours a day, a few days a week.
- Standard Outpatient Counseling: This involves regular individual or group therapy sessions on a less frequent basis, perfect for ongoing support or those with less severe conditions.
- Virtual Rehab Options: With technology making healthcare more accessible, many outpatient services are now available online! These programs, like virtual IOPs, can be a lifesaver, especially for those in rural areas or facing transportation challenges. You can explore more about your virtual rehab options.
Thanks to federal guidelines and the Mental Health Parity and Addiction Equity Act, Medicaid ensures that coverage for mental health and SUDs is just as comprehensive as for other medical conditions.
Medication-Assisted Treatment (MAT)
Medication-Assisted Treatment (MAT) is a powerful, evidence-based approach that truly makes a difference. It combines special, FDA-approved medications with counseling and behavioral therapies. This “whole-person” approach is incredibly effective for treating substance use disorders, especially opioid use disorder (OUD) and alcohol use disorder (AUD).
Medicaid’s coverage of MAT has been significantly strengthened by federal mandates. In fact, the Consolidated Appropriations Act, 2024 (CAA, 2024), made it a permanent mandatory benefit for Medicaid to cover medications for opioid use disorder (MOUD), along with the necessary counseling and behavioral therapies. This means states must cover all FDA-approved drugs for OUDs, making access easier than ever before.
Common MAT medications that Medicaid covers include:
- Methadone: Often used for OUD and typically administered in specialized clinics. You can learn more with our guide to methadone clinics.
- Buprenorphine (often combined with naloxone as Suboxone): Also for OUD, this can be prescribed in office-based settings, offering more flexibility.
- Naltrexone (Vivitrol, ReVia): Used for both OUD and AUD, it works by blocking the effects of opioids and reducing cravings for alcohol.
- Acamprosate and Disulfiram: These medications are primarily used to help reduce alcohol dependence.
And there’s more good news: all states cover the life-saving opioid reversal medication Naloxone, a critical tool in preventing overdose deaths. The federal government has made it abundantly clear that Medicaid plays a vital role in addressing the opioid crisis, actively pushing states to increase access to MAT. You can review the official guidance on mandatory Medicaid coverage for MAT.
Dual Diagnosis: Mental and Behavioral Health Services
It’s very common for people struggling with addiction to also experience co-occurring mental health conditions. This is what we call a dual diagnosis. Medicaid truly understands how important it is to treat both aspects at the same time for effective and lasting recovery. In fact, Medicaid is the largest payer for mental health services in the U.S., and its role in covering substance use disorder treatment is growing rapidly.
Does Medicaid Cover Drug & Alcohol Rehab when mental health is also a factor? Absolutely! Medicaid covers a wide array of mental and behavioral health services right alongside addiction treatment, ensuring a holistic approach to your well-being. These services can include:
- Individual Therapy: One-on-one sessions with a compassionate therapist to explore personal issues, develop coping mechanisms, and build strong recovery strategies.
- Group Therapy: Sessions with peers who are facing similar challenges. This creates a powerful sense of community, support, and shared experience.
- Cognitive Behavioral Therapy (CBT): An evidence-based therapy that helps you identify and gently shift negative thought patterns and behaviors into healthier ones.
- Psychiatric Care: This involves evaluation, diagnosis, and medication management for mental health conditions, all under the guidance of a medical professional.
- Case Management: Assistance in coordinating your care and connecting you with any other necessary services, making sure all your needs are met.
Treating dual diagnosis is absolutely crucial, and Medicaid ensures that these integrated services are available to you. For more comprehensive information, be sure to consult our mental health and substance abuse treatment guide and learn about anxiety disorder treatment centers if that’s relevant to your situation.
Navigating the Process: How to Use Medicaid for Rehab
If you’re wondering how to actually use your Medicaid benefits for drug and alcohol rehab, you’re not alone. Many people feel overwhelmed when they first start this journey. But here’s the truth: while the process has several steps, each one is manageable. We’re going to walk through this together, breaking it down so you know exactly what to do next.
Step 1: Confirming Your Medicaid Eligibility
Before you can use Medicaid for treatment, you need to confirm you’re actually eligible. This is your starting point. Since Medicaid is a joint federal and state program, the rules can shift a bit depending on where you live. But don’t worry—the basic guidelines are pretty consistent.
Income is the main factor. Your eligibility is tied to something called the Federal Poverty Level (FPL). Thanks to the Affordable Care Act, states that expanded Medicaid cover adults earning up to 138% of the FPL. The good news? Many states have expanded, including the ones where we work at Addiction Helpline America.
Your household size matters too. A family of four has a different income threshold than a single person. And there are some specific categories that can help you qualify, even if your income is a bit higher. These include pregnant women, children under 19, people receiving Supplemental Security Income (SSI), and individuals with qualifying disabilities.
To check the current FPL guidelines, visit Healthcare.gov’s FPL information. For official details on Medicaid eligibility, head to Medicaid.gov. We always recommend checking your state’s specific Medicaid website or calling your state’s Medicaid agency directly. They’ll have the most accurate information for your situation.
Step 2: Applying and Gathering Documentation
Once you know you’re likely eligible, it’s time to apply. You can usually do this through your state’s Medicaid agency or through the Health Insurance Marketplace at Healthcare.gov. The application itself isn’t too complicated, but you will need to gather some paperwork.
Think of it like preparing for a big trip—you need the right documents to get where you’re going. You’ll need proof of income, like pay stubs or tax returns. You’ll also need proof of residency, which could be a utility bill or lease agreement. Don’t forget your identification—a driver’s license, state ID, or passport works. And if you’re applying based on a disability or health condition, have your medical records ready.
The approval timeline varies. Depending on your state, how busy they are, and how complete your application is, it typically takes 45 to 90 days. Here’s something important that many people don’t know: benefits can often be covered retroactively for up to three months before your application date. This means if you needed care before you applied, you might still get coverage for it. That can be a huge relief.
Step 3: Finding a Rehab Center That Accepts Medicaid
With Medicaid coverage in hand, your next step is finding a treatment center that accepts it. This is where Does Medicaid Cover Drug & Alcohol Rehab? becomes a practical question. While not every facility accepts Medicaid, many do. In fact, in 2020, 71% of drug and alcohol treatment facilities nationwide accepted Medicaid. In California alone, there are 215 centers that work with Medicaid.
Your state behavioral health department is a great starting point. They keep lists of contracted facilities and can point you in the right direction. Another excellent resource is the Substance Abuse and Mental Health Services Administration (SAMHSA). They offer a national helpline and an online locator to help you find treatment facilities—visit SAMHSA’s official website to access these tools.
If you’re enrolled in a Medicaid Managed Care Organization (MCO), check their provider directory for in-network rehabs. Sometimes the simplest approach is the best: call treatment centers directly and ask if they accept your specific Medicaid plan. And remember, our team at Addiction Helpline America can help you find facilities within our network that accept Medicaid. That’s what we’re here for.
Step 4: Getting Prior Authorization
Here’s where things can get a little more technical, but stay with us. For certain services—especially more intensive ones like inpatient rehab or specific medications—Medicaid may require something called “prior authorization.” This basically means your healthcare provider needs to get approval from your Medicaid plan before you start treatment.
Your doctor or the treatment facility will assess your condition and provide documentation to Medicaid. They’re demonstrating that the proposed treatment is medically necessary for your recovery. Often, this requires a healthcare provider referral—a recommendation from a doctor or mental health professional.
The good news is that you usually don’t have to handle the paperwork yourself. The treatment center or your provider’s office typically submits all the documentation to Medicaid on your behalf. Then Medicaid reviews the request based on their criteria. It’s crucial that all the information is accurate and complete to avoid delays.
This step ensures that the treatment aligns with Medicaid’s guidelines and your medical needs. Taking the first steps to recovery often involves understanding and navigating these administrative requirements. We know it can feel like a lot, but we’re here to help simplify that process every step of the way.
Does Medicaid Cover Drug & Alcohol Rehab? Understanding State-by-State Differences
Does Medicaid Cover Drug & Alcohol Rehab? The answer is yes—but the details matter. Medicaid isn’t a one-size-fits-all program. It’s a partnership between the federal government and individual states, which means that while federal guidelines set a baseline, each state administers its own program. This leads to real variations in coverage, eligibility, and service delivery, especially when it comes to drug and alcohol rehab services.
Think of it this way: Medicaid is like a recipe with core ingredients that every state must include, but each state can add its own flavors and adjust the portions. This flexibility helps states tailor programs to their populations’ needs, but it also means your experience with Medicaid coverage can differ dramatically depending on where you live.
Right now, Medicaid covers approximately 83 million low-income people across the United States. This vast network highlights just how critical the program is for public health, especially for those seeking addiction treatment. For many Americans, Medicaid is the only realistic path to getting the help they need to overcome substance use disorders.
How Does Medicaid Coverage for Drug & Alcohol Rehab Vary by State?
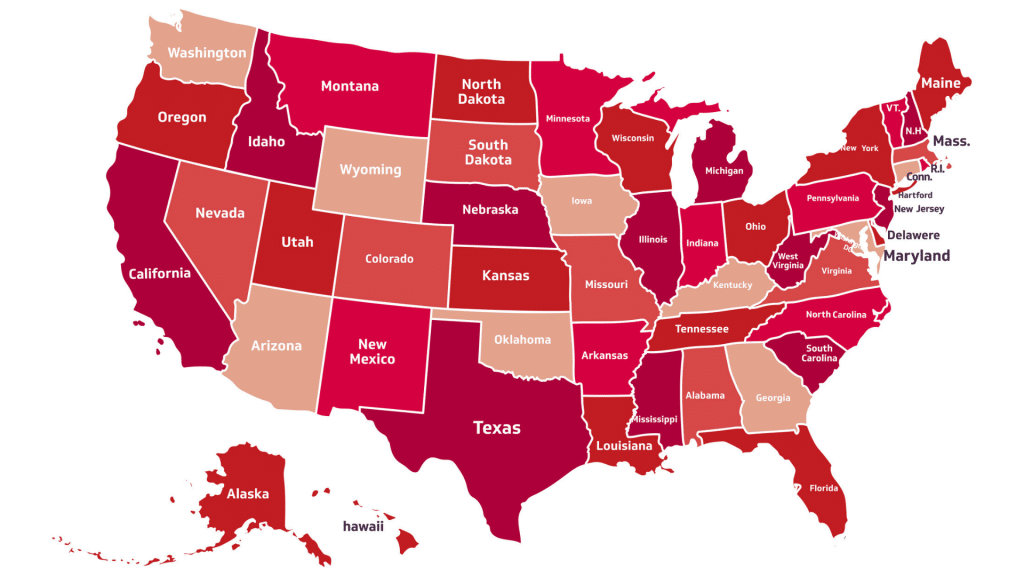
The biggest factor influencing how much coverage you’ll get is whether your state expanded its Medicaid program under the Affordable Care Act (ACA). All states where Addiction Helpline America operates—including Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, Virginia, Washington, West Virginia, Wisconsin, Wyoming, and the District of Columbia—have either expanded Medicaid or have alternative programs that provide similar coverage.
Medicaid expansion states generally offer broader coverage for low-income adults, extending eligibility to those earning up to 138% of the Federal Poverty Level (FPL). This expansion has demonstrably increased access to substance use services, giving more people the opportunity to get treatment without facing financial ruin.
Even among expansion states, though, the specific details can differ. While federal law now mandates coverage of essential health benefits—including addiction treatment—the scope and duration of these services can vary. For instance, some sources suggest that roughly one in ten states may not cover intensive outpatient treatment, one in eight states may not cover short-term residential care, and one in three states may not cover long-term residential care. These gaps highlight why it’s so important to verify your specific state’s benefits.
The provider networks available to you can also vary significantly by state. Some states have robust networks with many facilities accepting Medicaid, while others—particularly in rural areas—might have fewer options. This can affect how quickly you can access care and how far you might need to travel for treatment.
Every state has different rules for Medicaid eligibility and treatment coverage, and these rules change annually. For a deeper dive into how states deliver and administer behavioral health care, you can read this KFF study on state behavioral health delivery. To find your state’s specific Medicaid program name and information, visit Healthcare.gov’s Medicaid program names page.
Key Requirements and Limitations to Know
Even with Medicaid coverage, there are specific requirements and limitations you should understand before starting treatment. These aren’t meant to discourage you—they’re just practical realities that help you plan ahead and avoid surprises.
In-network providers are your best bet. Medicaid typically requires you to use approved providers within its network. If you go to an out-of-network provider without special prior authorization, you might end up paying the full cost yourself. Always confirm that a facility accepts your specific Medicaid plan before beginning treatment.
When it comes to copayments and out-of-pocket costs, most Medicaid recipients pay little to nothing for addiction treatment. Many states have eliminated copays for these services entirely, recognizing that financial barriers shouldn’t stand between someone and recovery. Still, it’s wise to confirm this with your specific plan or provider to avoid any confusion.
Length of stay limits are another consideration. Most Medicaid programs set limits on how long you can stay in inpatient or residential rehab. These limits are based on medical necessity—the idea that treatment should be intensive enough to be effective but not longer than clinically required. If you need an extended stay beyond the initial authorization, your treatment team will need to request re-authorization, demonstrating why continued care is medically necessary.
Some specific services or alternative therapies may not be covered in all states or may require special approval. For example, Medicaid typically does not cover sober living homes, as they’re not considered part of the formal continuum of care by government programs. However, many other evidence-based treatments—from medication-assisted treatment to intensive outpatient programs—are widely covered.
The key takeaway? Don’t be afraid to ask questions. Clarify these details with your state’s Medicaid agency or your chosen treatment provider before you start. Understanding what’s covered upfront helps you avoid unexpected costs and ensures you can focus on what really matters: your recovery.
Medicaid vs. Other Insurance for Rehab
Understanding how Medicaid compares to other insurance options can help you make informed decisions about treatment. Here’s a straightforward comparison:
| Feature | Medicaid | Private Insurance |
|---|---|---|
| Primary Costs | Minimal or no upfront fees for eligible individuals; most recipients pay little to nothing for addiction treatment | Varies widely; typically involves premiums, deductibles, copayments, and coinsurance |
| Eligibility | Based primarily on income and household size; some states extend coverage to certain categories like pregnant women or individuals with disabilities | Based on employment status, ability to purchase individual plans, or qualifying life events |
| Provider Network | Network size varies by state; some areas have robust networks while rural areas may have fewer options | Often larger networks in urban areas; may offer more facility choices, including some luxury or specialized centers |
| Covered Services | Comprehensive coverage of medically necessary addiction treatment, including detox, inpatient, outpatient, MAT, and dual diagnosis services | Similar comprehensive coverage required under the ACA, but specifics depend on the plan; some plans may have more restrictive authorization processes |
| Out-of-Pocket Maximum | Typically very low or none for addiction treatment services | Varies by plan; can be several thousand dollars annually |
| Authorization Requirements | Prior authorization often required for intensive services like inpatient rehab | Prior authorization commonly required; some plans have stricter requirements than Medicaid |
The bottom line? Medicaid offers excellent coverage for addiction treatment with minimal out-of-pocket costs, making it an invaluable resource for those who qualify. Private insurance may offer a wider choice of facilities in some areas, but often comes with higher costs that can be prohibitive for many families.
If you’re wondering Does Medicaid Cover Drug & Alcohol Rehab? and how it stacks up against your other options, our team at Addiction Helpline America can help you steer these comparisons and find the best path forward for your unique situation.
Frequently Asked Questions about Medicaid and Rehab
We know you probably have more questions about Does Medicaid Cover Drug & Alcohol Rehab? and how it all works. That’s perfectly normal! Taking charge of your health and understanding your options is a big step. Here are some of the most common questions we hear, answered to help you feel more confident on your path to recovery.
Does Medicaid cover out-of-state rehab?
Generally speaking, Medicaid programs are designed to serve residents within their specific state. Think of it like this: your state’s Medicaid is funded and managed to support its own citizens. So, as a rule, Medicaid does not cover out-of-state rehab. You’ll typically need to seek treatment in the state where you are enrolled in Medicaid.
However, life isn’t always straightforward, and there can be a few rare exceptions. If you face a true medical emergency while you’re out of state, your Medicaid might cover those emergency services, which could include emergency detox. In very specific, uncommon situations, some states might have special agreements for certain services, but this is usually not the case for full, comprehensive addiction treatment programs.
It’s also extremely difficult to get prior authorization for out-of-state treatment. This would only happen if a very specific, medically necessary service was absolutely unavailable in your home state, and even then, it’s a long and challenging process. For the smoothest and most reliable coverage, your best bet is always to find a treatment center within your Medicaid-enrolling state.
Are there free rehab options if I don’t qualify for Medicaid?
Yes, absolutely! We believe that financial challenges should never stand in the way of life-saving care. If Medicaid isn’t an option for you, or if your plan doesn’t cover a specific service you need, please know that there are still many pathways to recovery at little to no cost.
Many states fund or operate rehab centers directly. These state-funded programs use government money, often boosted by federal grants, to provide addiction treatment. Eligibility usually depends on your income, where you live, and whether you have other insurance. While sometimes there might be a waiting list, these programs often prioritize vulnerable groups, like pregnant women.
You can also look into non-profit organizations and charitable groups. They often offer free or very low-cost treatment, supported by donations and grants. Additionally, some treatment centers use a sliding scale fee structure, meaning the cost of treatment is adjusted based on what you can realistically afford to pay. The Substance Abuse and Mental Health Services Administration (SAMHSA) also provides grants to states to help uninsured or underinsured individuals access treatment. Your state’s behavioral health agency can be a great resource for finding these programs.
For more detailed information on these vital resources, you can explore our guide to free alcohol rehab.
What if my chosen rehab center doesn’t accept Medicaid?
It’s a common situation to find a rehab center that feels right, only to find they don’t accept your Medicaid plan. Don’t let this discourage you! While not every facility takes Medicaid, many excellent ones do. If you encounter this, here’s what you can do:
- Find an In-Network Provider: The most straightforward path is to look for an alternative treatment center that does accept your specific Medicaid plan. You can use resources like your state’s behavioral health department, SAMHSA’s online treatment locator, or your Medicaid Managed Care Organization’s (MCO) directory. Our team at Addiction Helpline America is also here to help you find facilities within our network that accept Medicaid.
- Ask About Payment Plans or Financing: Even if a facility doesn’t accept Medicaid, they might offer in-house payment plans or be able to connect you with third-party financing options to help manage costs. It’s always worth asking!
- Inquire About Referrals: Sometimes, the facility you initially contacted can be a great help. They might be able to refer you to a reputable center in their network that does accept Medicaid, ensuring you still get quality care.
- Advocate for Single-Case Agreements: This is very rare, but in highly specific circumstances, if the treatment you need is truly unique and only available at a particular facility, your Medicaid plan might consider a single-case agreement. This would require a strong case for medical necessity and a lot of documentation, so it’s not a common solution.
We always recommend having an open conversation with the treatment provider about all payment options before starting treatment. This way, you can ensure your care is covered and focus on what truly matters: your recovery.
Taking the First Step Towards Recovery
It’s completely normal to feel overwhelmed when you’re looking for help with a substance use disorder. It’s a big step, and navigating all the healthcare details can feel like a maze. But here’s the really important thing to remember: hope for recovery is always real, and even if money worries are on your mind, they don’t have to stop you.
The good news is that Medicaid covers drug & alcohol rehab for so many people across America. This means a clear path to healing could be right in front of you, taking a huge financial worry off your shoulders.
If you or someone you care about is struggling, please know this: you absolutely don’t have to go through it alone. Reaching out for help is one of the bravest and strongest things you can do. It’s the very first step toward building a healthier, happier life.
That’s where Addiction Helpline America comes in. We’re here to offer you free, confidential, and truly personalized guidance. Our main goal is to connect you with the right addiction and mental health treatment centers from our huge network across the country. We want to make sure you find a program that not only fits your unique needs but also accepts your insurance, including Medicaid.
Don’t let any lingering questions about coverage or what comes next hold you back from getting the support you deserve. Take that important first step today. Let us help you find the perfect insurance-covered rehab program for you.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.