Understanding Your Options for Addiction Treatment Through Medicare
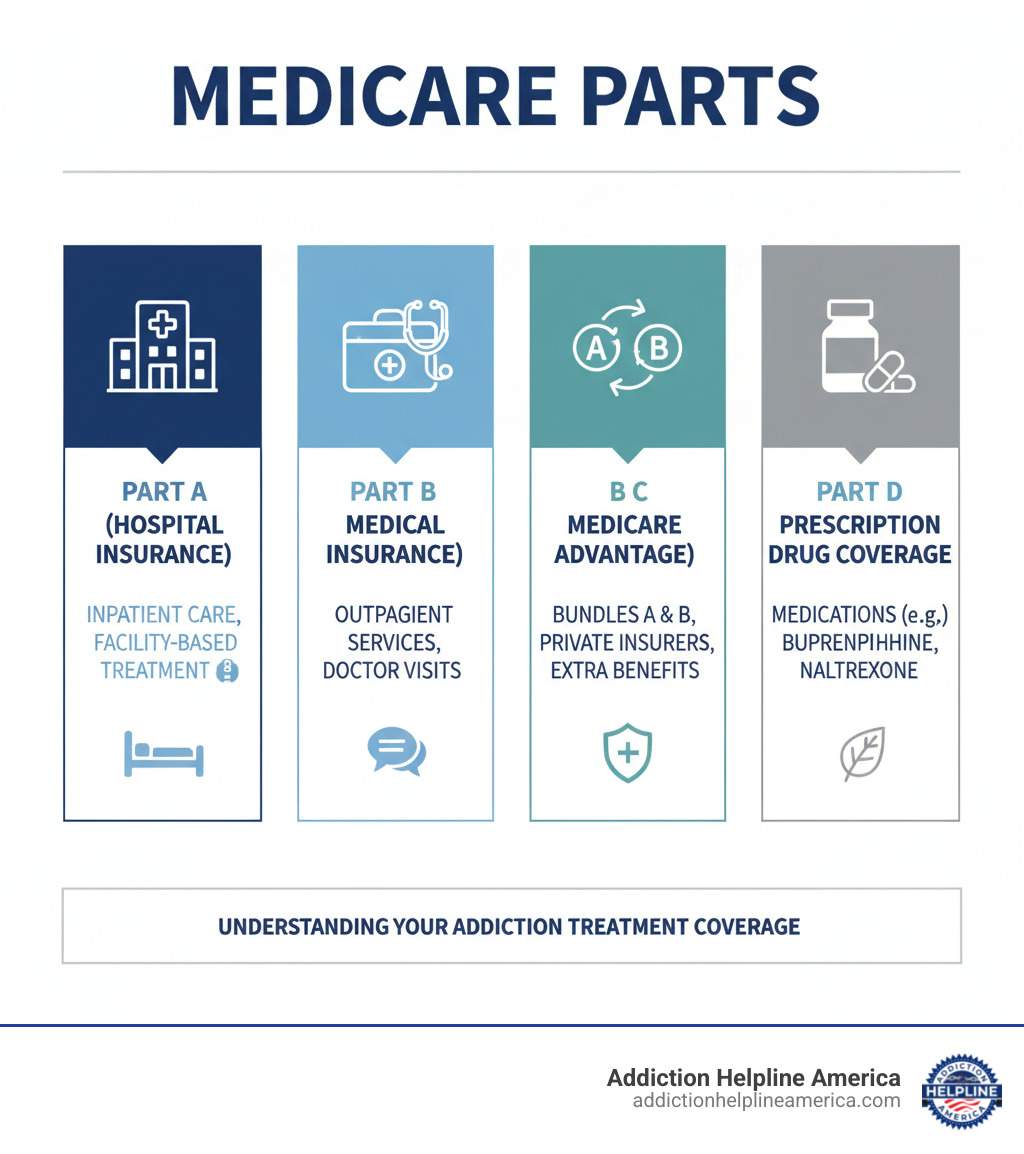
Medicare Insurance Coverage for Drug and Alcohol Rehab includes several important benefits for those seeking help with substance use disorders:
- Medicare Part A covers inpatient hospital stays and residential treatment at psychiatric facilities (up to 190 days lifetime for psychiatric hospitals)
- Medicare Part B covers outpatient services including therapy, counseling, and doctor visits (typically 80% after deductible)
- Medicare Part D covers prescription medications used in addiction treatment, such as buprenorphine
- Medicare Advantage Plans (Part C) bundle these benefits and may offer additional coverage
All services must be deemed medically necessary by your doctor and provided by Medicare-approved facilities.
Addiction is a growing health problem among adults 60 and over, with an estimated 1.7 million Medicare beneficiaries living with a substance use disorder. The good news is that Medicare does cover drug and alcohol rehabilitation.
Many people don’t realize that Medicare treats addiction as a medical condition. If your doctor determines treatment is medically necessary, Medicare will help pay for inpatient rehab, outpatient therapy, medication-assisted treatment, and mental health services. Understanding what’s covered can be overwhelming, but we’re here to help.
At Addiction Helpline America, we guide families through the complexities of Medicare Insurance Coverage for Drug and Alcohol Rehab to help them access care without delay.
Understanding Medicare and Its Role in Addiction Treatment
Medicare is the federal health insurance program primarily for people 65 or older, though some younger people with certain disabilities, End-Stage Renal Disease (ESRD), or ALS also qualify. You can learn more at What’s Medicare?.
Crucially, Medicare treats substance use disorder as a real medical condition. This means that when your doctor determines treatment is medically necessary, Medicare will help cover it, just as it would for diabetes or heart disease. Medicare recognizes that effective treatment must address both the physical and psychological aspects of recovery, which is why Medicare Insurance Coverage for Drug and Alcohol Rehab includes everything from hospital stays to ongoing therapy.
Medicare Part A: Hospital Insurance
Medicare Part A is your hospital insurance. For addiction treatment, Part A covers inpatient care when you need intensive, round-the-clock support in a hospital or inpatient rehab facility. It covers your semi-private room, meals, nursing services, and medications administered during your stay.
There is a 190-day lifetime limit for inpatient care specifically in psychiatric hospitals. Stays in general hospitals for addiction treatment do not count toward this limit.
Medicare Part B: Medical Insurance
While Part A handles hospital stays, Medicare Part B covers the outpatient services that form the backbone of most recovery programs. This includes individual and group therapy, psychiatric evaluations, and preventive services like Screening, Brief Intervention, and Referral to Treatment (SBIRT).
As of January 2024, Medicare expanded its list of approved providers to include licensed professional counselors, mental health counselors, and addiction counselors, giving you more options for finding the right therapist.
Medicare Part C: Medicare Advantage
Medicare Advantage, or Part C, is an alternative to Original Medicare offered by private insurance companies. These plans bundle Part A and Part B, and often include Part D prescription drug coverage. While they may offer extra benefits like dental or vision, they typically require you to use a network of doctors and facilities.
Some plans, called Special Needs Plans (SNPs), are specifically designed for people with conditions like chronic substance dependence, offering more targeted support.
Medicare Part D: Prescription Drug Coverage
Medicare Part D covers your prescription medications, which is crucial for those in recovery. Private companies offer these plans, which may be included in a Medicare Advantage plan or purchased separately.
For opioid addiction, Part D typically covers Medication-Assisted Treatment (MAT) drugs like buprenorphine (Suboxone) and naltrexone. Each plan has a formulary (a list of covered drugs), so you must check that your specific medications are included. Methadone for Opioid Use Disorder is an exception; it is typically covered under Part B when administered at a certified Opioid Treatment Program.
Your Guide to Medicare Insurance Coverage for Drug and Alcohol Rehab
Your Medicare Insurance Coverage for Drug and Alcohol Rehab begins when your doctor confirms that treatment is medically necessary. This allows Medicare to cover various levels of care at Medicare-approved facilities, ensuring you receive quality, evidence-based treatment.
Inpatient and Residential Treatment
When 24/7 care is needed, Medicare Part A covers inpatient and residential treatment in a general hospital, inpatient rehab facility, or psychiatric hospital. Part A covers your semi-private room, meals, nursing services, and therapies. Remember the 190-day lifetime limit for care in a psychiatric hospital. For more details, see Medicare’s guide to Inpatient Rehabilitation Care.
Outpatient Treatment Programs (PHP, IOP, and General Outpatient)
Medicare Part B covers several types of outpatient treatment, allowing you to live at home while receiving structured support. These include:
- Partial Hospitalization Programs (PHP): The most intensive option, with 20+ hours of therapy per week.
- Intensive Outpatient Programs (IOP): A step-down option with 9+ hours of services weekly.
- General Outpatient Treatment: Regular individual or group therapy sessions.
For these services, you typically pay 20% of the Medicare-approved amount after meeting your annual Part B deductible. You can learn more at Mental health & substance use disorders.
Detoxification and Medication-Assisted Treatment (MAT)
Medicare covers detox based on the level of supervision you need. Inpatient detox (Part A) is for severe cases requiring 24/7 medical monitoring in a hospital. Outpatient detox (Part B) is for less severe cases.
Medication-Assisted Treatment (MAT), which combines therapy with medication, is also well-covered. Part D covers take-home prescriptions like buprenorphine (Suboxone) and naltrexone. Part B covers methadone and related therapy administered at certified Opioid Treatment Programs (OTPs).
Co-Occurring Disorders and Mental Health Services
Addiction often co-occurs with mental health conditions like depression or anxiety. Treating both together—known as dual diagnosis or integrated care—is critical for recovery. Medicare Part B covers a full range of mental health services, including psychotherapy, psychiatric evaluations, and medication management, ensuring you receive comprehensive care.
At Addiction Helpline America, we understand that recovery addresses the whole person. Our team can help connect you with facilities that specialize in dual diagnosis treatment, ensuring you get comprehensive care for both your addiction and any underlying mental health conditions.
Navigating Costs and Plan Differences

Even with Medicare, you will likely have some out-of-pocket costs for addiction treatment. Understanding these costs can make planning for treatment less stressful.
Understanding Costs for Medicare Insurance Coverage for Drug and Alcohol Rehab
When exploring Medicare Insurance Coverage for Drug and Alcohol Rehab, you’ll encounter several cost-sharing terms:
- Deductible: The amount you pay before Medicare pays. For 2025, the Part A deductible is $1,676 per benefit period. The 2024 Part B deductible is $240 per year.
- Coinsurance: Your percentage of the cost after the deductible. For Part B, it’s typically 20%. For Part A, it applies to long hospital stays (e.g., $419 per day for days 61-90 in 2025).
- Copayment: A fixed dollar amount for a service, common in Medicare Advantage and Part D plans.
A benefit period for Part A starts when you’re admitted to a hospital and ends after 60 consecutive days without inpatient care. You also have 60 non-renewable lifetime reserve days for hospital stays beyond 90 days.
Original Medicare vs. Medicare Advantage for Addiction Treatment
Choosing between Original Medicare and Medicare Advantage involves a trade-off between flexibility and cost structure.
Original Medicare (Parts A and B) offers the freedom to see any doctor or visit any facility in the U.S. that accepts Medicare, with no referrals needed. This is ideal if you have a specific treatment program in mind. You will need a separate Part D plan for prescription coverage and will typically pay 20% coinsurance for Part B services.
Medicare Advantage (Part C) plans bundle Parts A, B, and usually D through a private insurer. They often have lower upfront costs and may include extra perks like dental or vision. However, these plans almost always require you to stay within their provider network and may require referrals.
The right choice depends on your priorities. Do you value flexibility, or do you prefer bundled benefits and potentially lower costs?
What to Do if Costs Are a Barrier
If you’re worried about affording treatment, several safety nets exist:
- Medicaid: If you have a limited income, you may be “dual eligible” for both Medicare and Medicaid. Medicaid can cover many remaining costs, including deductibles and coinsurance. Contact your State Medical Assistance (Medicaid) office to see if you qualify.
- Extra Help program: This federal program helps people with limited income pay for Part D prescription costs.
- Sliding Scale Fees & Payment Plans: Many treatment centers offer payment options based on what you can afford.
- Medigap Policies: If you have Original Medicare, a private Medigap policy can help cover costs like deductibles and coinsurance.
At Addiction Helpline America, we can help you explore every available option to make treatment affordable.
How to Verify and Use Your Medicare Benefits
Being proactive about verifying your coverage and finding the right facility is key to a smooth start to recovery.
Verifying Your Medicare Insurance Coverage for Drug and Alcohol Rehab
Before beginning treatment, verify your Medicare Insurance Coverage for Drug and Alcohol Rehab to avoid surprises. Here’s how to get clear answers:
- Call the number on your Medicare card for specific details about your plan’s deductibles, coinsurance, and covered services.
- Use the Medicare.gov provider search tool to find facilities and professionals who accept Medicare.
- Ask the rehab facility’s admissions team directly. They can often verify your benefits and estimate your out-of-pocket costs.
For Medicare to cover your treatment, your doctor must confirm that the services are “medically necessary.”
Finding a Medicare-Approved Rehab Facility
Medicare coverage applies to services from Medicare-approved providers. If you have a Medicare Advantage plan, staying in-network is important to keep costs down. Original Medicare offers more flexibility, allowing you to see any provider who accepts Medicare. Use the “Find Providers” tool on Medicare.gov to locate service providers in your area.
When speaking with a potential treatment center, ask these questions:
- “Do you accept Medicare for addiction treatment?”
- “Are you a Medicare-approved facility?”
- “Can you help me verify my benefits and estimate my costs?”
- “What is your state licensing status?”
Always ensure the facility is licensed by the state in which it operates.
Telehealth Services for Addiction and Mental Health
Telehealth offers a wonderfully convenient and private way to access addiction and mental health treatment. Medicare now covers a wide range of telehealth services, making care more accessible, especially for those in rural areas or with mobility challenges.
This means you can receive vital support like individual and group therapy, counseling, and psychiatric evaluations from home using video or phone calls. This expansion helps reduce barriers to getting the care you need. You can learn more about what Medicare covers for these services at Telehealth.
Frequently Asked Questions about Medicare and Rehab
When you’re trying to understand Medicare Insurance Coverage for Drug and Alcohol Rehab, getting straight answers matters. Here are some common questions.
How long will Medicare pay for addiction rehab?
The duration of coverage depends on the type of care. For inpatient care (Part A), Medicare covers up to 90 days per benefit period, with an additional 60 lifetime reserve days. There is a separate 190-day lifetime limit for care in a psychiatric hospital. For outpatient services (Part B), such as therapy, there is no specific time limit as long as your doctor continues to certify that the care is medically necessary.
Does Medicare cover medications for addiction like Suboxone or Methadone?
Yes. Medicare Part D plans typically cover prescription medications used in recovery, such as Suboxone (buprenorphine) and naltrexone. You should always check your specific plan’s formulary (list of covered drugs). Methadone for Opioid Use Disorder is covered differently; Medicare Part B covers the medication and associated counseling when administered at a certified Opioid Treatment Program (OTP).
What should I do if Medicare denies coverage for my treatment?
A denial is not the final word; you have the right to appeal. The first step is to file a “request for redetermination” with your plan. Gather all supporting documents, including your doctor’s notes explaining why treatment is medically necessary. You can find appeal instructions on Medicare.gov or get free, personalized help from your State Health Insurance Assistance Program (SHIP).
At Addiction Helpline America, we understand how discouraging a denial can feel. We can help you explore your options and connect you with facilities that work with Medicare, supporting you through the verification process to avoid surprises.
Start Your Recovery Journey Today
It’s true, figuring out all the details of Medicare Insurance Coverage for Drug and Alcohol Rehab can feel a bit overwhelming, especially when you’re already facing the challenges that come with addiction. But here’s the good news: this guide has shown that Medicare really does offer a lot of help for many types of addiction treatment. This includes everything from getting help with detox and staying in a residential program, to going to outpatient therapy and using special medications.
Recovery isn’t just a dream; it’s a real path forward, especially for older adults and anyone covered by Medicare. The most important thing? Taking that very first step. Whether it’s just looking for information, chatting with your doctor, or reaching out for support, that step can change everything.
That’s where we come in. At Addiction Helpline America, we’re here to offer you free, confidential, and personal guidance. We know all about the ins and outs of Medicare. We can help you check what your benefits cover and connect you with treatment centers that accept Medicare, no matter where you are in the country – from Alabama to Wyoming, and even Washington D.C. Our goal is simple: to help you find the right recovery program that fits your needs.
Don’t let feeling confused or scared stop you from a healthier, happier future. Ready to take that vital step towards lasting recovery? Learn how to get into rehab and verify your benefits today.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.