
Does Anthem Cover Drug and Alcohol Rehab?
When facing addiction, the cost of treatment is a major concern. The good news is that Anthem Insurance Coverage for Drug and Alcohol Rehab is generally available. Due to federal laws like the Affordable Care Act (ACA) and the Mental Health Parity and Addiction Equity Act (MHPAEA), most Anthem plans must cover substance use disorder (SUD) treatment as an essential health benefit, on par with medical care.
This means your Anthem plan likely covers:
- Medically supervised detox
- Inpatient (residential) rehab
- Outpatient programs (PHP, IOP)
- Medication-assisted treatment (MAT)
- Treatment for co-occurring mental health disorders
However, coverage specifics, costs, and requirements like prior authorization vary by plan. Choosing in-network providers is the best way to minimize your out-of-pocket expenses.
Navigating insurance while dealing with addiction can be overwhelming. At Addiction Helpline America, we guide individuals and families through the complexities of Anthem Insurance Coverage for Drug and Alcohol Rehab, providing compassionate support and resources to help you access effective treatment.

Anthem is legally obligated to offer coverage for drug and alcohol rehab, but the specifics depend on your individual plan. Anthem BlueCross BlueShield offers a variety of plans, including individual, family, Medicare, Medicaid, and employer-sponsored plans, each with a unique benefit structure. For instance, as of January 1, 2024, Empire BlueCross BlueShield in New York rebranded to Anthem Blue Cross and Blue Shield (Anthem), continuing to offer comprehensive coverage under the new name.
What Levels of Care Does Anthem Cover?
Anthem’s coverage extends across a full spectrum of care to meet different needs. The types of addiction treatment Anthem generally covers include:
- Medical Detox: The safe, supervised management of withdrawal symptoms. Anthem typically covers medically necessary detox to prepare you for further treatment.
- Inpatient Rehab: Also known as residential treatment, this involves living at a facility 24/7 for intensive therapy. Anthem plans may cover inpatient stays when a high level of care is needed.
- Partial Hospitalization Programs (PHP): A structured, high level of care where patients return home in the evenings. Anthem typically covers PHP for those who need intensive treatment without 24-hour supervision.
- Intensive Outpatient Programs (IOP): Flexible programs with multiple therapy sessions per week, allowing you to maintain work or family life. Anthem usually covers IOPs as a vital part of sustained recovery.
- Outpatient Therapy and Counseling: This includes individual, group, and family therapy sessions to support ongoing recovery.
- Medication-Assisted Treatment (MAT): An evidence-based approach combining FDA-approved medications (like Suboxone) with therapy. Anthem typically covers MAT, though pre-authorization may be required.
Your specific plan will detail the exact coverage amounts. For more on these options, see our Types of Addiction Treatment Programs guide.
Does Anthem Cover Co-Occurring Disorders?
Yes, Anthem generally covers treatment for co-occurring disorders (or dual diagnosis), where addiction exists alongside conditions like depression, anxiety, or PTSD. Treating both conditions simultaneously is a best practice for long-term recovery.
Anthem’s mental health benefits are designed to provide integrated care, covering behavioral therapy, medication management, and other services for conditions listed in the DSM-5. This holistic approach is aligned with the MHPAEA, ensuring mental health coverage is comparable to physical health coverage.
For more information, explore our Behavioral Health and Dual Diagnosis guide or visit Anthem’s behavioral health support page.
Navigating Your Specific Anthem Plan for Rehab
While Anthem covers rehab, your specific plan determines the details. Understanding your plan—whether it’s from an employer, the marketplace, Medicare, or Medicaid—is key to managing costs. Key factors include your plan type, network status, and out-of-pocket responsibilities.
One of the most important distinctions is between in-network and out-of-network providers. In-network facilities have pre-negotiated rates with Anthem, which means lower costs for you. Going out-of-network can result in significantly higher expenses or no coverage at all.
Your out-of-pocket costs are what you pay directly. These include deductibles, copays, and coinsurance, which we’ll break down below.
How Anthem Plan Types Affect Your Coverage
Anthem offers various health plans, and their structures affect your Anthem Insurance Coverage for Drug and Alcohol Rehab. Here are the main types:
- HMO (Health Maintenance Organization): These plans often have lower premiums but require you to use in-network providers. You’ll also typically need a referral from your Primary Care Physician (PCP) to see a specialist, including an addiction treatment provider.
- PPO (Preferred Provider Organization): PPO plans offer more flexibility, allowing you to see both in-network and out-of-network providers without a referral. However, your out-of-pocket costs will be higher if you choose a provider outside the network.
Marketplace plans are categorized into Bronze, Silver, Gold, or Platinum tiers, which indicate how costs are shared:
- Bronze: Lowest monthly premiums, highest out-of-pocket costs (you pay ~40%).
- Silver: Moderate premiums and out-of-pocket costs (you pay ~30%).
- Gold: Higher premiums, lower out-of-pocket costs (you pay ~20%).
- Platinum: Highest premiums, lowest out-of-pocket costs (you pay ~10%).
For more on these tiers, see this guide to understanding metal tiers.
- Employer-sponsored plans: Coverage varies widely depending on the plan your employer has chosen.
- Medicaid plans: If you qualify for an Anthem Medicaid plan, rehab services are generally covered with very low or no out-of-pocket costs.
- Medicare Advantage (Part C) plans: These plans bundle Medicare benefits and typically include coverage for substance use disorder treatment.
Explore all Anthem plan options on their official site.
Here’s a quick look at how HMO vs. PPO plans stack up for rehab:
| Feature | HMO Plans | PPO Plans |
|---|---|---|
| Network Rules | Must use in-network providers | Can use in-network or out-of-network providers |
| Referral Needs | Often requires PCP referral for specialists | Typically no referral needed for specialists |
| Out-of-Network | Not covered (except emergencies) | Covered, but at a higher cost to you |
Understanding Your Potential Out-of-Pocket Costs
Even with good coverage, you will likely have some out-of-pocket costs. Here are the key terms to know:
- Deductible: The amount you must pay for covered services before your Anthem plan starts paying.
- Copay: A fixed fee (e.g., $30) you pay for a specific service, like a therapy session, after meeting your deductible.
- Coinsurance: A percentage of the cost you pay for a service after your deductible is met. For example, with 80/20 coinsurance, Anthem pays 80% and you pay 20%.
- Out-of-pocket maximum: The absolute most you will have to pay for covered services in a plan year. Once you hit this limit, Anthem pays 100% of covered costs for the rest of the year, providing a crucial financial safety net.
These amounts vary based on your specific plan. To better understand the financial side of treatment, read our guide on How Much Does Drug Rehab Cost?.
The Process: How to Use Your Anthem Insurance Coverage for Drug and Alcohol Rehab
Accessing your Anthem Insurance Coverage for Drug and Alcohol Rehab involves a few clear steps. Following this process will help you get the care you need without unnecessary stress.
Step 1: Verify Your Specific Anthem Insurance Coverage for Drug and Alcohol Rehab
First, confirm the exact benefits and limitations of your personal Anthem plan. This will clarify your potential costs and treatment options.
Here’s how to verify your coverage:
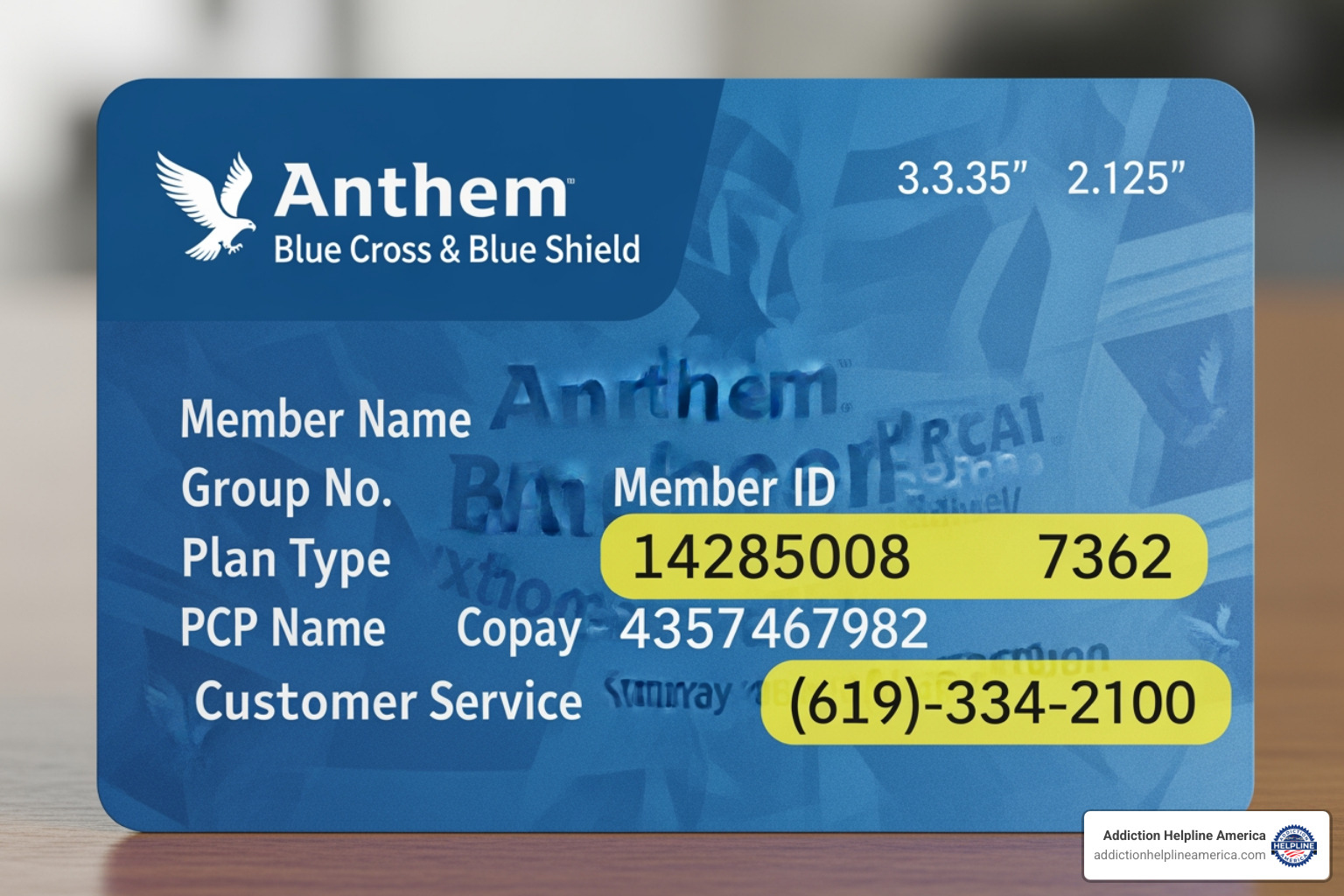
- Call Anthem Customer Service: The member services phone number is on the back of your insurance card. Have your Member ID and Group ID ready.
- Use the Anthem Member Portal: Log in to your account on the Anthem member portal to review your benefits, check claims, and find providers.
- Review Your Summary of Benefits and Coverage (SBC): This document, which you received when you enrolled, provides a clear summary of your plan’s coverage and costs.
Verifying coverage upfront helps you understand your financial responsibility and avoid surprises.
Step 2: Find an In-Network Rehab Center
Next, find a treatment facility that is in-network with Anthem. This is crucial for maximizing your coverage and minimizing your out-of-pocket costs.
Here’s how to find an in-network facility:
- Use Anthem’s “Find Care” Tool: This online directory, available on Anthem’s website, allows you to search for in-network facilities by location and service type (e.g., “substance abuse treatment”).
- Ask About the BlueCard Program: If you’re considering treatment in another state, the BlueCard program may allow you to use your benefits at Blue Cross Blue Shield providers nationwide at in-network rates.
- Contact Facilities Directly: Once you have a list of potential centers, call them and provide your insurance information. Most rehabs offer free insurance verification to confirm your benefits.
Choosing an in-network provider is the most effective way to make treatment financially manageable. For more help finding a facility, see our Find Addiction Rehab Centers Guide.
Step 3: Get Pre-Authorization
Pre-authorization (or prior authorization) is Anthem’s approval that a treatment is medically necessary. It is often required for intensive services like inpatient rehab, PHP, and IOP. Failing to get required pre-authorization can lead to a denial of coverage, leaving you responsible for the full cost.
What requires pre-authorization?
- Inpatient (residential) rehab
- Partial Hospitalization Programs (PHP)
- Intensive Outpatient Programs (IOP)
- Certain medications used in Medication-Assisted Treatment (MAT)
Your doctor or the rehab facility’s admissions team will typically handle the pre-authorization process. They submit clinical documentation to Anthem to demonstrate medical necessity. Your role is to ensure they have your correct insurance information and to confirm that authorization has been secured before you begin treatment.
Frequently Asked Questions about Anthem Rehab Coverage
Navigating insurance can be confusing. Here are answers to some of the most common questions about Anthem Insurance Coverage for Drug and Alcohol Rehab.
How long will Anthem cover my addiction treatment?
The length of your treatment coverage is determined by medical necessity, not a fixed number of days. Anthem will cover your care for as long as your providers can demonstrate a clinical need for it. Your treatment team will communicate with Anthem, providing updates to justify continued care based on your progress.
Factors that influence the duration of coverage include:
- The severity of your addiction
- Your progress in treatment
- The type of substance used
- The presence of co-occurring mental health conditions
While some plans may have initial limits, these can often be extended with proper medical justification. For more on this, see our Long Term Rehab Guide.
Does Anthem cover rehab in a different state?
Yes, Anthem often covers out-of-state rehab, but it depends on your plan type.
- PPO plans offer the most flexibility. Through the BlueCard program, you can often access Blue Cross Blue Shield providers nationwide at your lower, in-network rates.
- HMO plans are more restrictive and typically require you to stay within a local network. However, some HMOs offer a guest membership for extended treatment (e.g., 90+ days), allowing you to receive in-network benefits in another state.
Always call Anthem’s customer service to verify your out-of-state benefits before committing to a program.
What should I do if Anthem denies coverage for my treatment?
A denial is not the final word. You have the right to appeal the decision, and many appeals are successful.
- Understand the Denial: Carefully read Anthem’s denial letter to learn the specific reason for their decision.
- File an Internal Appeal: Submit a formal request for Anthem to reconsider your case. Work closely with your treatment provider to gather supporting documents, such as clinical notes and letters of medical necessity, to strengthen your appeal.
- Request an External Review: If your internal appeal is denied, you can request an external review. An independent third party will evaluate your case, and their decision is legally binding for Anthem.
Don’t give up after a denial. Your treatment provider can be a powerful ally in the appeals process. We at Addiction Helpline America can also help you steer these challenges to access the Anthem Insurance Coverage for Drug and Alcohol Rehab you are entitled to.
Conclusion: Take the First Step on Your Recovery Journey
Understanding your Anthem Insurance Coverage for Drug and Alcohol Rehab is a powerful first step toward healing. As we’ve covered, Anthem plans provide coverage for a full spectrum of addiction treatment, from detox to outpatient care, but your specific benefits and costs will depend on your plan.
The key is to verify your coverage, find an in-network provider, and secure pre-authorization when needed. While this process can feel complex, you don’t have to do it alone.
At Addiction Helpline America, we offer free, confidential guidance to help you make sense of your insurance and find a treatment program that fits your needs. Our team works with a nationwide network of quality centers and can quickly verify your Anthem benefits to match you with the right care.
Recovery is achievable. Help is available. Your journey can start today.
Get help finding a rehab that accepts your insurance
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.












