Understanding Bipolar I Disorder: A Serious Condition That Demands Comprehensive Care
Bipolar 1 treatment is a lifelong commitment combining medication, therapy, and lifestyle management to stabilize mood and improve quality of life. A comprehensive approach includes:
- Medications: Mood stabilizers and second-generation antipsychotics.
- Psychotherapy: Cognitive behavioral therapy (CBT) and family-focused therapy.
- Lifestyle Management: Regular sleep, stress management, and avoiding alcohol and drugs.
Bipolar I disorder, which affects about 8 million adults in the U.S., is defined by extreme mood swings. A diagnosis requires at least one manic episode lasting a week or more (or requiring hospitalization), often alongside depressive episodes.
The consequences of untreated bipolar disorder are severe, reducing life expectancy by 12 to 14 years. The suicide rate is over 60 times higher than in the general population, with 15% to 20% of individuals with the disorder dying by suicide.
Unfortunately, diagnosis and treatment are often delayed by an average of 9 years, and over 50% of patients struggle with treatment adherence. The condition is also frequently complicated by co-occurring substance use disorders, affecting up to 60% of individuals.
At Addiction Helpline America, we guide individuals and families in finding effective bipolar 1 treatment programs that address these complex, often dual-diagnosis, challenges with specialized, compassionate care.
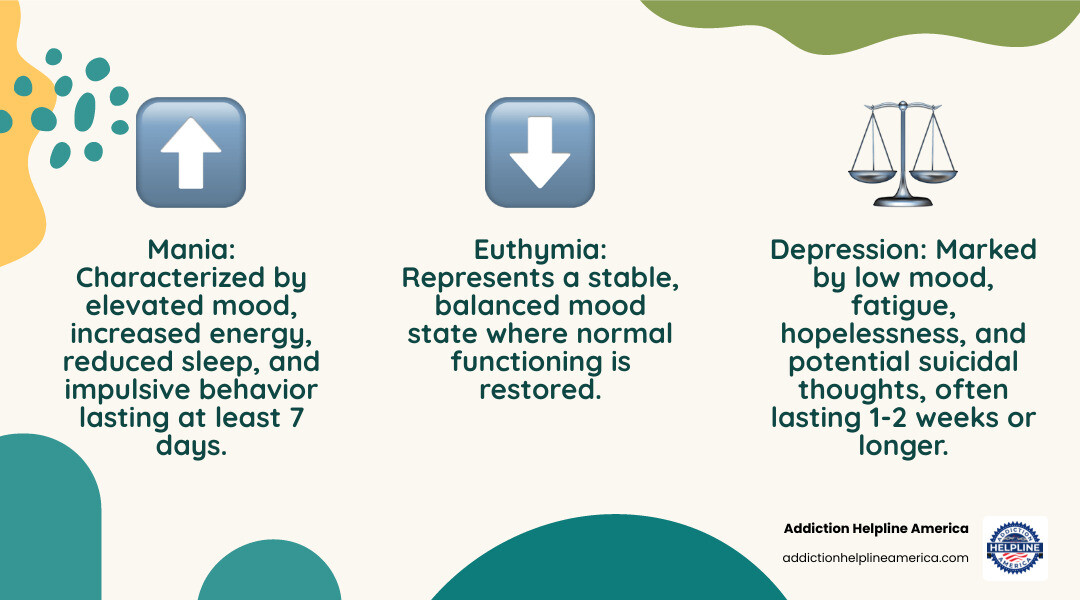
Bipolar 1 treatment terms made easy:
The Foundation of Care: Diagnosis and Treatment Goals

Accurate diagnosis is the first step toward effective bipolar 1 treatment and is strongly linked to better long-term outcomes.
The diagnostic process is thorough. It begins with a physical exam and lab tests to rule out medical causes like thyroid problems. A mental health professional then conducts a detailed assessment of your thoughts, feelings, and behaviors throughout your life. Input from family and friends is often invaluable, as they can describe behavioral changes during manic episodes that you may not recognize as problematic. Mood charting—tracking daily moods, sleep, and activities—also helps reveal patterns.
Clinicians use the DSM-5 criteria, which require at least one manic episode lasting at least seven days (or any duration if hospitalization is needed) for a Bipolar I diagnosis. This full manic episode distinguishes it from Bipolar II disorder.
Differentiating Bipolar I from other conditions like major depression, schizophrenia, or borderline personality disorder is crucial, as misdiagnosis can lead to ineffective or harmful treatments. This is especially challenging in children and adolescents, where symptoms can overlap with ADHD.
Once diagnosed, treatment focuses on several key goals:
- Symptom Management: The immediate priority is controlling acute manic or depressive episodes to restore stability.
- Relapse Prevention: As a chronic condition, the long-term goal is to prevent or reduce the frequency and severity of future mood episodes.
- Restoring Functioning: Treatment aims to help you rebuild and regain footing in work, school, and relationships.
- Improving Quality of Life: The ultimate goal is to lead a fulfilling, meaningful life despite the challenges of the illness.
Comprehensive care must also address co-occurring conditions. Up to 60% of people with bipolar disorder also battle substance use disorders, which must be treated concurrently. Anxiety, ADHD, and physical health issues like metabolic syndrome and cardiovascular disease are also common and require integrated management.
For those with co-occurring anxiety, specialized inpatient anxiety treatment can be beneficial. At Addiction Helpline America, we connect you with programs that address your complete health picture.
Pharmacological Approaches to Bipolar 1 Treatment
Medication is the foundation of managing bipolar I disorder, providing the stability necessary for therapy and lifestyle changes to be effective. Bipolar 1 treatment uses a phase-based approach, with acute treatment for current episodes and maintenance treatment to prevent future ones.
Here’s a comparison of common first-line mood stabilizers:
| Medication Type | Primary Use (Bipolar I) | Common Side Effects | Necessary Monitoring |
|---|---|---|---|
| Lithium | Acute Mania, Maintenance (mania & depression prevention) | Tremor, nausea, increased thirst, frequent urination, weight gain, cognitive slowing | Blood lithium levels (weekly initially, then every 3-6 months), kidney function, thyroid function, calcium levels, ECG |
| Valproate (Divalproex) | Acute Mania, Maintenance (mania & depression prevention) | Nausea, vomiting, tremor, sedation, hair loss, weight gain, liver issues, pancreatitis, teratogenicity (significant risk in pregnancy) | Liver function tests, complete blood count, valproate levels (if concerns), weight, for women of childbearing potential: strict pregnancy prevention program |
| Lamotrigine | Bipolar Depression (maintenance) | Skin rash (can be severe, Stevens-Johnson Syndrome), nausea, dizziness, headache | Monitor for rash (especially early in treatment), liver function, complete blood count (less frequent than lithium/valproate) |
First-Line Medications for Acute Mania and Maintenance
For acute mania, the goal is rapid stabilization using mood stabilizers and second-generation antipsychotics (SGAs).
- Lithium: Often considered the gold standard, it is effective for acute mania and long-term maintenance. It has been shown to reduce suicide risk but requires careful blood monitoring to avoid toxicity.
- Anticonvulsants: Valproate is highly effective for acute mania and mixed episodes but carries serious risks during pregnancy. Carbamazepine is another option, particularly for rapid cycling, but requires monitoring for drug interactions.
- Second-Generation Antipsychotics (SGAs): These have become central to treatment. Quetiapine is versatile for mania, depression, and maintenance. Olanzapine and risperidone are effective for acute mania, with risperidone available in a long-acting injectable form to aid adherence. Aripiprazole and cariprazine are also effective for manic episodes. For severe mania, combining a mood stabilizer with an SGA is often most effective. For more on current approaches, see A review on the diagnosis and treatment of Bipolar Disorder.
Navigating Bipolar Depression and Medication Precautions
Treating bipolar depression requires a different strategy, as people with Bipolar I spend most of their symptomatic time in a depressive state. First-line options include quetiapine, cariprazine, lurasidone (often with lithium or valproate), and the olanzapine-fluoxetine combination.
Crucially, antidepressants should never be used alone (as monotherapy) for bipolar I disorder. They can trigger mania or rapid cycling, worsening the condition. If used, they must be paired with a mood stabilizer or an antipsychotic. Lamotrigine is not used for acute mania but is highly valuable in maintenance treatment for preventing future depressive episodes.
Long-Term and Treatment-Resistant Bipolar 1 Treatment
Bipolar I is a lifelong condition requiring indefinite maintenance treatment to prevent relapse. For individuals with treatment-resistant bipolar disorder, several options exist.
- Medication Optimization: This may involve adjusting doses or combining multiple medications.
- Clozapine: An antipsychotic reserved for severe, treatment-resistant cases, requiring close monitoring.
- Electroconvulsive Therapy (ECT): A highly effective treatment for severe, treatment-resistant mania or depression, especially with psychosis or high suicide risk. It can also be used for maintenance.
- Transcranial Magnetic Stimulation (TMS): A non-invasive procedure approved for treatment-resistant depression and being studied for bipolar depression.
- Ketamine: Used in low doses, it shows promise for rapid, short-term relief from treatment-resistant bipolar depression and suicidal thoughts.
At Addiction Helpline America, we help you connect with programs experienced in managing complex medication needs for bipolar 1 treatment.
The Role of Psychotherapy and Lifestyle Management
While medication is essential for managing bipolar I disorder, it is most effective when combined with psychotherapy and lifestyle changes. This holistic approach addresses the whole person, not just the symptoms, leading to fewer relapses and a better quality of life.
Evidence-Based Psychotherapies
Therapy provides practical skills to manage the illness. Research shows that combining psychotherapy with medication leads to better outcomes than medication alone.
- Cognitive Behavioral Therapy (CBT): Helps you identify and change negative thought patterns and behaviors that can trigger mood episodes.
- Family-Focused Therapy (FFT): Involves family members in the treatment process, improving communication, problem-solving, and the support system.
- Interpersonal and Social Rhythm Therapy (IPSRT): Focuses on stabilizing daily routines (sleep, meals, activities), as disruptions can trigger mood episodes.
- Psychoeducation: Provides in-depth knowledge about bipolar disorder, its treatment, and relapse warning signs, empowering you to be an active participant in your care. The NIMH has documented how such interventions improve outcomes, as detailed in NIMH research on psychotherapy effectiveness.
Therapy helps develop coping skills, improves medication adherence, and allows for early intervention before a full mood episode develops, leading to better functioning and a greater sense of control.
Self-Management and Lifestyle Modifications
Daily choices are a critical part of effective bipolar 1 treatment. These strategies help stabilize mood between appointments.
- Sleep Hygiene: Prioritizing a consistent sleep schedule is critical, as lack of sleep is a primary trigger for mania. Aim for the same bedtime and wake time daily.
- Consistent Routines: Regular schedules for meals, work, and other activities help regulate your internal clock and promote stability.
- Stress Management: Techniques like meditation, deep breathing, yoga, and regular exercise are powerful tools for managing life’s inevitable stressors.
- Mood Diary: Tracking daily mood, sleep, and stressors helps you and your team identify patterns and triggers, allowing for proactive adjustments to your treatment plan.
- Avoiding Alcohol and Drugs: Substance use can destabilize mood, interfere with medications, and increase the frequency and severity of episodes. Given that up to 60% of people with bipolar disorder also have a substance use disorder, addressing this is non-negotiable. At Addiction Helpline America, we specialize in finding dual diagnosis treatment.
- Support System: Healthy relationships with friends, family, and support groups provide a crucial safety net.
Self-management is about progress, not perfection. Building habits that support stability most of the time is the goal.
Special Considerations in Bipolar 1 Treatment

Bipolar 1 treatment must be adapted for specific life stages and situations, such as pregnancy and adolescence, requiring personalized and expert care.
Treatment for Women of Childbearing Age
For women with bipolar I disorder, treatment decisions require a careful balance of maternal health and fetal safety. Untreated bipolar disorder during pregnancy poses significant risks to both mother and baby, so planning is key.
- Valproate: This medication carries a high risk of birth defects and developmental problems. According to MHRA guidance on valproate use by women and girls, it must not be used in women of childbearing potential unless no other treatment is effective and a strict pregnancy prevention program is followed.
- Lithium: While it carries some risks, it is generally considered a safer option than valproate during pregnancy. Women stable on lithium may continue it at the lowest effective dose with close monitoring.
Collaborative family planning with a psychiatrist and obstetrician before conception is essential to make thoughtful medication adjustments. The postpartum period is also a high-risk time for mood episodes due to hormonal shifts, sleep deprivation, and stress, requiring close monitoring and strong support.
Treating Children and Adolescents
Diagnosing and treating bipolar I disorder in youth is challenging. Symptoms can present differently than in adults and overlap with conditions like ADHD.
- Diagnosis: A Bipolar I diagnosis in a young person requires a distinct manic episode with euphoria (not just irritability) for at least seven days. Careful, long-term assessment by a specialist is needed to ensure an accurate diagnosis.
- Treatment: The approach is measured and cautious. Psychotherapy and psychosocial interventions (individual or family) are typically the first line of treatment. They provide young people and their families with essential coping skills.
- Medication: When necessary, medication is used with extra caution. Doses are started low, and side effects are monitored closely. Valproate should generally be avoided. Family and school support is foundational, with family-focused therapy and psychoeducation empowering everyone involved.
At Addiction Helpline America, we help families find specialized bipolar 1 treatment programs that understand the unique needs of young people.
Frequently Asked Questions about Bipolar 1 Treatment
We’ve heard the same questions about bipolar 1 treatment from many families. Here are some honest, straightforward answers.
How long does it take for bipolar 1 treatment to work?
Patience is key when starting medication. Mood stabilizers like lithium may take two weeks to begin reducing manic symptoms, with full stabilization taking several weeks to months. Antipsychotics can work faster for acute mania, sometimes within days. It’s common to try different medications or combinations to find the most effective regimen with the fewest side effects. Consistency is vital; continuing medication even when you feel better is crucial for long-term stability.
Can Bipolar I be managed without medication?
For the vast majority of people, the answer is no. Bipolar I is a biological brain condition, and medication is the necessary cornerstone of treatment to correct underlying chemical imbalances. Without it, the risk of severe mood episodes, hospitalization, and suicide increases dramatically. Abruptly stopping medication often leads to severe relapse. However, psychotherapy and lifestyle modifications are crucial supports that work alongside medication to build coping skills, manage stress, and improve overall well-being. They are essential components of a comprehensive plan, not replacements for medication.
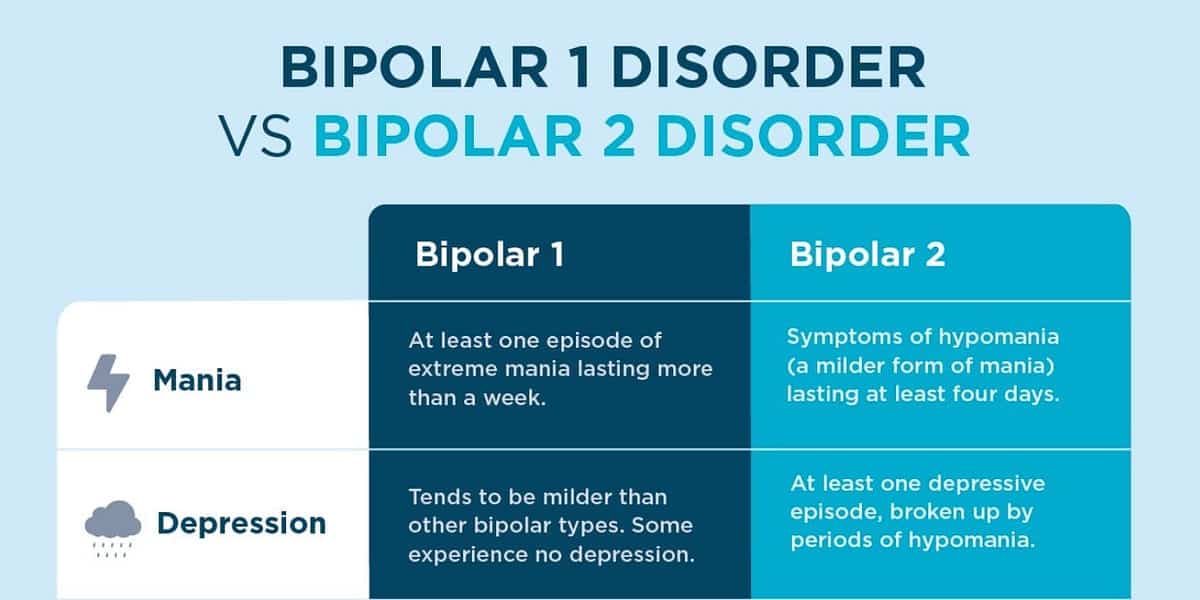
What is the difference between Bipolar I and Bipolar II treatment?
The primary difference lies in the severity of the liftd mood episodes. Bipolar I disorder is defined by at least one full-blown manic episode, which is severe, may involve psychosis, and often requires hospitalization. Consequently, treatment for Bipolar I prioritizes managing and preventing these dangerous manic episodes.
Bipolar II disorder involves less severe hypomanic episodes and is often characterized by more frequent and prolonged periods of depression. Therefore, its treatment may focus more on preventing depressive episodes. While both conditions use similar treatments (mood stabilizers, antipsychotics, therapy), the specific medication choices and strategies are custom to the primary challenge—severe mania in Bipolar I versus depression and hypomania in Bipolar II. For more on Bipolar II, see our Bipolar Disorder 2 Treatment Complete Guide.
Finding Hope and Getting Help
Learning about bipolar 1 treatment is a vital step toward managing this condition. While bipolar I disorder is a lifelong illness, we want you to know that there is hope. With the right treatment, countless individuals lead stable, fulfilling lives.
Effective care is built on these key principles:
- Early Diagnosis: Seeking a professional evaluation at the first sign of symptoms can prevent years of struggle.
- Medication: Mood stabilizers and antipsychotics are the cornerstone of treatment, providing essential brain chemistry balance.
- Psychotherapy: Therapies like CBT and FFT provide the skills needed to steer daily life, manage stress, and prevent relapse.
- Lifestyle Management: Consistent routines, especially for sleep, along with stress management and avoiding substances, are critical for stability.
- Support System: A strong network of family, friends, and professionals is an invaluable safety net.
Navigating bipolar I disorder is even more complex when addiction is involved, a reality for up to 60% of individuals with the condition. Addressing both simultaneously is essential for recovery.
This is where Addiction Helpline America can help. We specialize in connecting people to dual diagnosis treatment centers across the United States. Our team offers free, confidential guidance to help you find a program that fits your unique needs.
You don’t have to do this alone. Stability and well-being are achievable. Take the next step toward recovery today.
Find professional help for bipolar disorder today
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.












