
Understanding What Happens When You Stop Using Drugs
Drug withdrawal is the collection of physical and psychological symptoms that occur when a person dependent on a substance stops or reduces their use. Symptoms can range from uncomfortable (muscle aches, anxiety) to life-threatening (seizures from alcohol or benzodiazepine withdrawal).
Quick Facts About Drug Withdrawal:
- Cause: The body adapts to a drug’s presence and must readjust when it’s removed.
- Common Symptoms: Anxiety, depression, nausea, sweating, tremors, insomnia, and intense cravings.
- Timeline: Varies by substance, from days to months.
- Risk: Alcohol and benzodiazepine withdrawal can be fatal without medical supervision.
- Treatment: Medical detox, medication, and ongoing support are most effective.
The severity of withdrawal depends on the drug used, duration of use, dosage, and your overall health.
Physical dependence is when your body adapts to a drug and needs it to function normally, causing withdrawal symptoms without it. This differs from psychological dependence, which is a mental craving for the drug’s effects.
Regular drug use disrupts your brain’s chemical balance, a process called homeostasis disruption. When the drug is removed, this imbalance causes withdrawal symptoms until the brain can readjust.
At Addiction Helpline America, we provide 24/7 guidance on safe detox options and connect people with medical care. We understand withdrawal is a frightening barrier to recovery, and we’re committed to helping you steer this phase with compassionate support.
Key drug withdrawal vocabulary:
Understanding the Symptoms and Timeline of Drug Withdrawal
Stopping a substance your body depends on leads to drug withdrawal. The symptoms vary based on the substance, duration and amount of use, your age, and overall health.
Withdrawal symptoms are often the opposite of the drug’s effects. This happens because your brain works to balance out the drug; when it’s gone, your brain’s chemistry is thrown off until it can readjust.
Cravings are intense, overwhelming urges to use again and are a difficult part of withdrawal. Managing cravings is crucial for long-term recovery, as they can be triggered by people, places, or emotions long after physical symptoms fade.
Several factors influence withdrawal severity. Older adults may have a harder time due to slower metabolism. Longer use creates deeper dependence. Your physical and mental health also play a major role; co-occurring disorders like anxiety or depression can intensify withdrawal symptoms, making integrated treatment essential.
The type of substance, dosage, and how you stop all matter. Quitting “cold turkey” is typically more severe than a medically supervised taper.
For a complete picture, visit our page on Drug Withdrawal Symptoms.
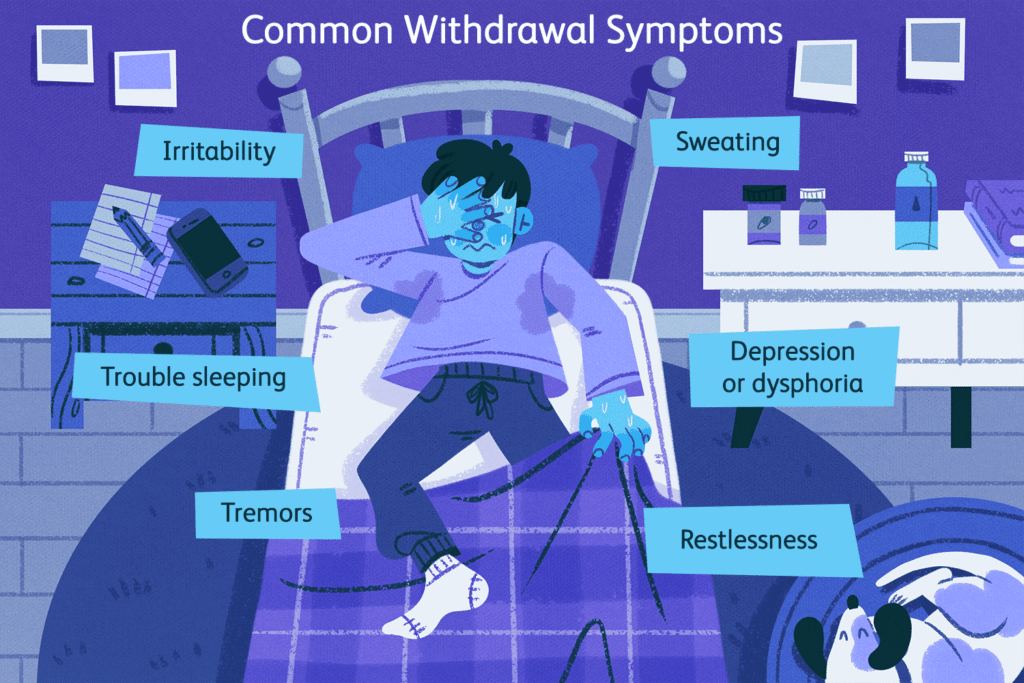
Common Symptoms of Drug Withdrawal
Drug withdrawal affects both mind and body.
Psychological symptoms can be overwhelming and may include:
- Anxiety and agitation
- Depression and hopelessness
- Irritability and mood swings
- Insomnia
- Difficulty concentrating
- In severe cases (especially with alcohol or benzodiazepines), psychosis (hallucinations or delusions).
Physical symptoms are equally challenging:
- Muscle and joint aches
- Nausea, vomiting, and diarrhea
- Sweating and headaches
- Tremors (shaking)
- Increased heart rate and blood pressure
- In severe cases (especially with alcohol and benzodiazepines), seizures, which require immediate medical attention.
These symptoms reflect real disruption in your brain’s chemistry, as documented in scientific research on withdrawal syndromes.
Withdrawal Timelines for Common Substances
The timeline for drug withdrawal varies dramatically by substance.
| Substance | Onset of Withdrawal Symptoms | Peak Severity | Duration (Acute Phase) | Notable Symptoms/Risks |
|---|---|---|---|---|
| Alcohol | 6-12 hours after last drink | 24-72 hours | 5-7 days | Tremors, anxiety, seizures, hallucinations; risk of Delirium Tremens (DTs)—potentially fatal without medical care |
| Opioids (short-acting) – heroin, oxycodone, hydrocodone | 8-24 hours after last use | 36-72 hours | 4-10 days | Severe flu-like symptoms, muscle aches, anxiety, insomnia, diarrhea; not typically life-threatening but extremely uncomfortable |
| Opioids (long-acting) – methadone, buprenorphine | 2-4 days after last use | 3-8 days | 10-20 days | Similar to short-acting but milder and more prolonged |
| Benzodiazepines – Xanax, Valium, Ativan | 1-4 days after last use | Varies widely | Weeks to months | Anxiety, insomnia, seizures; potentially fatal; often requires very slow taper |
| Stimulants – cocaine, methamphetamine | Within hours to 24 hours | 2-4 days | 1-2 weeks (acute) | Severe depression, fatigue, intense cravings, increased appetite, disturbed sleep |
Delirium Tremens (DTs) is a dangerous complication of alcohol withdrawal, typically starting 48-72 hours after the last drink. It causes confusion, hallucinations, and seizures and can be fatal without treatment. This is why medical supervision for alcohol withdrawal is essential.
Protracted withdrawal, or Post-Acute Withdrawal Syndrome (PAWS), involves symptoms that can last for months or years, especially with benzodiazepines. These are mostly psychological (anxiety, depression, insomnia) and occur as the brain slowly heals.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Opiate and Opioid Withdrawal Symptoms
Withdrawal from opiates (heroin, morphine) and opioids (oxycodone, fentanyl) is notoriously miserable, often described as a severe flu. The timeline depends on the drug’s duration of action.
- Short-acting opioids (e.g., heroin): Symptoms start in 8-24 hours, peak in 36-72 hours, and last 4-10 days.
- Long-acting opioids (e.g., methadone): Symptoms start in 2-4 days and can last 10-20 days.
Symptoms include agitation, muscle aches, runny nose, sweating, yawning, abdominal cramping, diarrhea, goosebumps, nausea, and vomiting. While not typically fatal, opiate and opioid withdrawal is difficult to endure alone. Medical guidance makes the process safer and more bearable. Learn more about opiate and opioid withdrawal.
The Risks and Potential Complications of Withdrawal
Drug withdrawal isn’t just uncomfortable—it can be dangerous, and for certain substances, even deadly. Understanding these risks is crucial for your safety.
While most people associate drug use with overdose, withdrawal itself can be lethal. This is particularly true for alcohol and benzodiazepines (e.g., Xanax, Valium).
- Alcohol withdrawal can lead to delirium tremens (DTs), a condition affecting fewer than 5% of people in withdrawal but fatal in about 15% of those cases if untreated. DTs can cause severe confusion, hallucinations, seizures, and cardiac arrest.
- Benzodiazepine withdrawal carries similar dangers. Abruptly stopping can trigger life-threatening seizures. Protracted symptoms can also persist for months or years, making medical support essential.
Other serious complications from drug withdrawal include seizures from various depressants, severe dehydration from vomiting and diarrhea, and aspiration pneumonia (a lung infection caused by inhaling vomit). Chronic alcohol users also risk Wernicke-Korsakoff syndrome, a brain disorder from thiamine deficiency that withdrawal can worsen.
One of the biggest dangers occurs right after detox: overdose. Withdrawal lowers your tolerance. If you relapse and use your previous dose, it can be fatal. This is why most opiate overdose deaths happen to people who recently detoxed. Ongoing treatment after detox is lifesaving.
When to Contact a Medical Professional
Always consult a medical professional before stopping a substance. However, some symptoms of drug withdrawal require immediate emergency help. Call 911 if you or a loved one experiences:
- Severe hallucinations (seeing or hearing things that aren’t there)
- Seizures of any kind
- Delirium (severe confusion or disorientation)
- Uncontrollable vomiting, diarrhea, or tremors
If you are having suicidal thoughts, call or text 988 or chat at 988lifeline.org for free, confidential, 24/7 support. Medical supervision during withdrawal can save your life. We can connect you with Emergency Detox Services to ensure your safety.
Managing Prescription Medicine Drug Withdrawal
Drug withdrawal also occurs with prescribed medications like painkillers, benzodiazepines, and antidepressants. While the physical dependence is the same as with illicit drugs, there are added complexities, such as managing the underlying condition the medication was treating.
Tapering schedules are essential for these medications. A slow, medically supervised reduction in dose gives your body time to adjust and minimizes withdrawal severity. Abruptly stopping antidepressants can cause Antidepressant Discontinuation Syndrome (flu-like symptoms, dizziness, sensory disturbances), while stopping benzodiazepines can cause seizures.
Doctor consultation is non-negotiable when stopping prescription medications. Never quit cold turkey. Your doctor can create a safe tapering plan and provide support. This is especially critical for painkillers, where dependence can develop even when taken as prescribed. Your doctor understands this is a physiological response and will help you find the safest path forward.
For more information, visit our page on Drug For Anxiety and Depression.
Navigating Treatment for Drug Withdrawal
Understanding the treatment process for drug withdrawal can make the experience safer and more manageable. Here’s what to expect.

The first step is a diagnosis. A medical professional will conduct a physical exam and use blood or urine tests to identify substances and check your overall health. They may use standardized tools like the Clinical Opiate Withdrawal Scale (COWS) for opioids or the CIWA-Ar for alcohol to measure withdrawal severity and determine the right level of care.
Based on this assessment, your team will create a personalized treatment plan involving medical detox. This process safely manages your withdrawal symptoms under medical supervision, providing a safety net as your body readjusts. Medical detox keeps you safe from complications, makes you more comfortable, and builds a foundation for long-term recovery.
Medications Used in Detox
Medications can ease discomfort and prevent serious complications during drug withdrawal. The specific medication depends on the substance.
- For opioid withdrawal: Methadone and buprenorphine relieve withdrawal symptoms and cravings. You can learn why methadone is used for drug withdrawal on our site. Clonidine helps with physical symptoms. Naltrexone can be used after detox to help prevent relapse.
- For alcohol withdrawal: Benzodiazepines (e.g., diazepam) are the standard treatment to prevent seizures and reduce anxiety. Gabapentin may also be used in some cases.
- For stimulant withdrawal: Treatment is primarily supportive care to manage psychological symptoms like depression and cravings. Benzodiazepines may be used for severe agitation.
Supportive medications like anti-nausea drugs or sleep aids may also be prescribed to manage specific symptoms.
Treatment Settings for Detox
Choosing the right detox setting is a critical decision based on the substance, severity of dependence, and your overall health.
- Home-based withdrawal: This is only an option for mild withdrawal (not from alcohol or benzodiazepines) and requires close medical supervision and a strong home support system.
- Inpatient detox facilities: These provide 24/7 medical supervision in a safe, structured environment. This is the recommended choice for moderate to severe withdrawal or for those with co-occurring health conditions.
- Hospital settings: Necessary for severe, life-threatening withdrawal, such as DTs or uncontrolled seizures, offering the highest level of medical care.
- Outpatient detox programs: A middle ground for those with mild to moderate dependence and a stable home life. You live at home and attend regular medical appointments.
Choosing a setting can be overwhelming. Addiction Helpline America can help you assess your needs and connect you with appropriate detox centers in your area, from Alabama to Wyoming.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
How to Support a Loved One Through Withdrawal
Watching someone you care about go through drug withdrawal is difficult. Your support can make a huge difference in their recovery. Here’s how you can help.

Pre-withdrawal planning:
Preparation is key. Before withdrawal begins, take these steps:
- Consult a healthcare professional. This is non-negotiable. A doctor can explain what to expect and determine if home withdrawal is safe. Never attempt home withdrawal for alcohol or benzodiazepines without medical supervision.
- Create a safe environment. Remove all substances, paraphernalia, and triggers. Make the space calm and comfortable.
- Discuss medications. Ask the doctor about medications that can ease withdrawal symptoms.
- Set realistic expectations. Your loved one may be irritable, anxious, or hostile. Understand that this is a symptom of withdrawal and try not to take it personally.
- Plan for emergencies. Know when to call 911 and have the doctor’s number handy.
During withdrawal support:
Your loved one will need patient care. Provide fluids and nutrition by encouraging them to drink water, electrolyte drinks, or broth. Offer small, easy-to-digest meals like toast, crackers, or bananas. Good hydration and nutrition can ease symptoms and reduce relapse risk.
Emotional support is vital. Be present, listen without judgment, and offer simple reassurances like, “I’m here for you.” Gently remind them of their reasons for quitting when they feel like giving up. Help them stay occupied with low-energy activities like movies or audiobooks. Guide them through simple relaxation techniques like deep breathing.
Post-withdrawal care:
When acute drug withdrawal ends, the journey is just beginning. It’s important to understand the difference between a lapse (a single use) and a relapse (a return to regular use). A lapse is not a failure, but it is dangerous due to lowered tolerance, which increases overdose risk. Seek medical help if a lapse occurs.
Caregiver self-care is essential. You cannot support someone else if you are depleted. Eat well, get enough sleep, and maintain your own social connections. Consider joining a support group like Al-Anon or Nar-Anon. Taking breaks and seeking your own support is not selfish—it’s necessary.
Finding Long-Term Support
Detox is the first step; long-term recovery requires ongoing support to prevent relapse. Addiction is a chronic condition that needs long-term management.
- Counseling: Individual and group therapy help address the root causes of addiction and build healthy coping skills.
- Inpatient/Outpatient Treatment: Inpatient programs offer 24/7 support, while outpatient programs provide structured treatment with more flexibility.
- Support Groups: Groups like Narcotics Anonymous (NA) and SMART Recovery provide crucial peer support and accountability.
- Peer Support: Specialists with lived recovery experience offer unique mentorship and guidance.
The Substance Abuse and Mental Health Services Administration (SAMHSA) offers more resources at www.samhsa.gov/find-support.
Addiction Helpline America offers free, confidential guidance to find the right program. We can connect you with Family Support and other Support and Resources. For a full overview, see our Addiction Recovery Complete Guide.
Recovery is possible. With the right support, people build meaningful lives in sobriety every day.
Frequently Asked Questions about Withdrawal
If you’re facing drug withdrawal, you likely have many questions. Here are answers to some of the most common ones we hear at Addiction Helpline America.
How long does drug detox typically last?
The timeline for drug withdrawal varies depending on the substance, duration of use, dosage, and individual factors. General timeframes for the acute phase are:
- Short-acting opioids (e.g., heroin): Symptoms start in 8-24 hours and last 4-10 days.
- Long-acting opioids (e.g., methadone): Symptoms start in 2-4 days and last 10-20 days.
- Alcohol: Symptoms start within hours, peak at 24-72 hours, and resolve within a week. Severe complications like DTs can last longer.
- Benzodiazepines: Acute withdrawal can last from a few weeks to months, with some protracted symptoms persisting even longer.
- Stimulants (e.g., cocaine): The acute “crash” lasts a few days, but psychological symptoms like depression and cravings can linger for weeks.
Most medical detox programs aim to stabilize patients within 5-10 days, but feeling “normal” takes more time and requires ongoing treatment.
Is it safe to detox at home?
This depends entirely on the substance and the severity of dependence.
Detoxing from alcohol or benzodiazepines at home without medical supervision is extremely dangerous and can be fatal. The risk of seizures and delirium tremens is too high to attempt it alone. Please seek professional medical help.
For other substances, home detox may be an option, but only after a medical consultation. A doctor can assess your health, recommend the safest approach, and determine if you are a candidate. Even then, it should only be attempted with a strong, sober support system at home to monitor you and seek help if complications arise. In most cases, professional detox is the safest and most effective option.
What is the difference between physical dependence and addiction?
This is a crucial distinction.
Physical dependence is a physiological state where your body has adapted to a drug and needs it to function normally. If you stop, you experience withdrawal symptoms. You can be physically dependent on a medication even when taking it exactly as prescribed by a doctor.
Addiction, clinically known as Substance Use Disorder, is a chronic brain disease characterized by compulsive drug seeking and use despite harmful consequences. It involves loss of control and continuing to use even when it damages your health, relationships, and life. Addiction involves long-term changes to the brain’s reward, motivation, and memory circuits.
You can have physical dependence without addiction (e.g., a patient on prescribed painkillers). You can also have an addiction with less severe physical dependence (e.g., cocaine). Understanding this difference is key: detox manages physical dependence, but overcoming addiction requires long-term treatment like therapy and support groups to address the underlying brain disease.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Your Path to a Healthy, Drug-Free Life
If you’re reading this, you’ve already taken the courageous first step: seeking information. Drug withdrawal is the gateway to a life free from substance dependence. It’s a temporary, though challenging, process that you don’t have to face alone.
Professional help makes the process safer and more manageable. Medical detox provides supervision and support to guide you through withdrawal, preparing you for the next phase of recovery. Lasting recovery comes from addressing the root causes of use through counseling, support groups, and treatment programs.
At Addiction Helpline America, we are here to guide you. We offer free, confidential support to connect you with a trusted treatment program that fits your unique needs. We serve every state, from California to New York, and treat every call with the compassion you deserve.
Your story doesn’t end with addiction. It begins again with hope. When you’re ready to take the next step, we’re here to help you find your path forward.
Explore addiction treatment programs
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















