Why Understanding Stimulant Addiction Treatment Matters Now
Stimulant addiction treatment offers proven paths to recovery. Key approaches include:
- Behavioral therapies like Contingency Management (CM) and Cognitive Behavioral Therapy (CBT), which are the most effective treatments.
- Withdrawal management (detox) to safely manage initial symptoms.
- Various levels of care, from outpatient counseling to 24/7 inpatient treatment.
- Recovery support services like peer groups and family therapy to strengthen your journey.
Stimulant use disorder (StUD) is a global issue, affecting 35 million people worldwide in 2021. The stakes are high: in 2022, 35,000 people died from stimulant overdoses in the U.S. alone, with over 71% of these deaths also involving an opioid.
Despite these numbers, recovery is possible. People overcome stimulant addiction every day through evidence-based treatment.
Stimulants like cocaine and methamphetamine flood the brain with dopamine, creating an intense high followed by a crash. The brain adapts, making it hard to feel pleasure without the drug, which drives cravings. Research shows that behavioral therapies are highly effective. Contingency Management, which rewards positive behaviors, has the strongest scientific support for treating StUD. When combined with CBT and community support, people can and do rebuild their lives.
At Addiction Helpline America, we guide individuals and families toward effective stimulant addiction treatment, connecting them with evidence-based programs that match their unique needs. Our team is available 24/7 to help you steer the path to recovery.
Basic stimulant addiction treatment glossary:
Understanding Stimulant Addiction: Signs, Types, and Brain Effects
It’s important to understand what stimulants are, how they affect the body, and how to spot a developing problem. The effects of stimulants go far beyond a temporary high, impacting brain chemistry, physical health, and daily life.
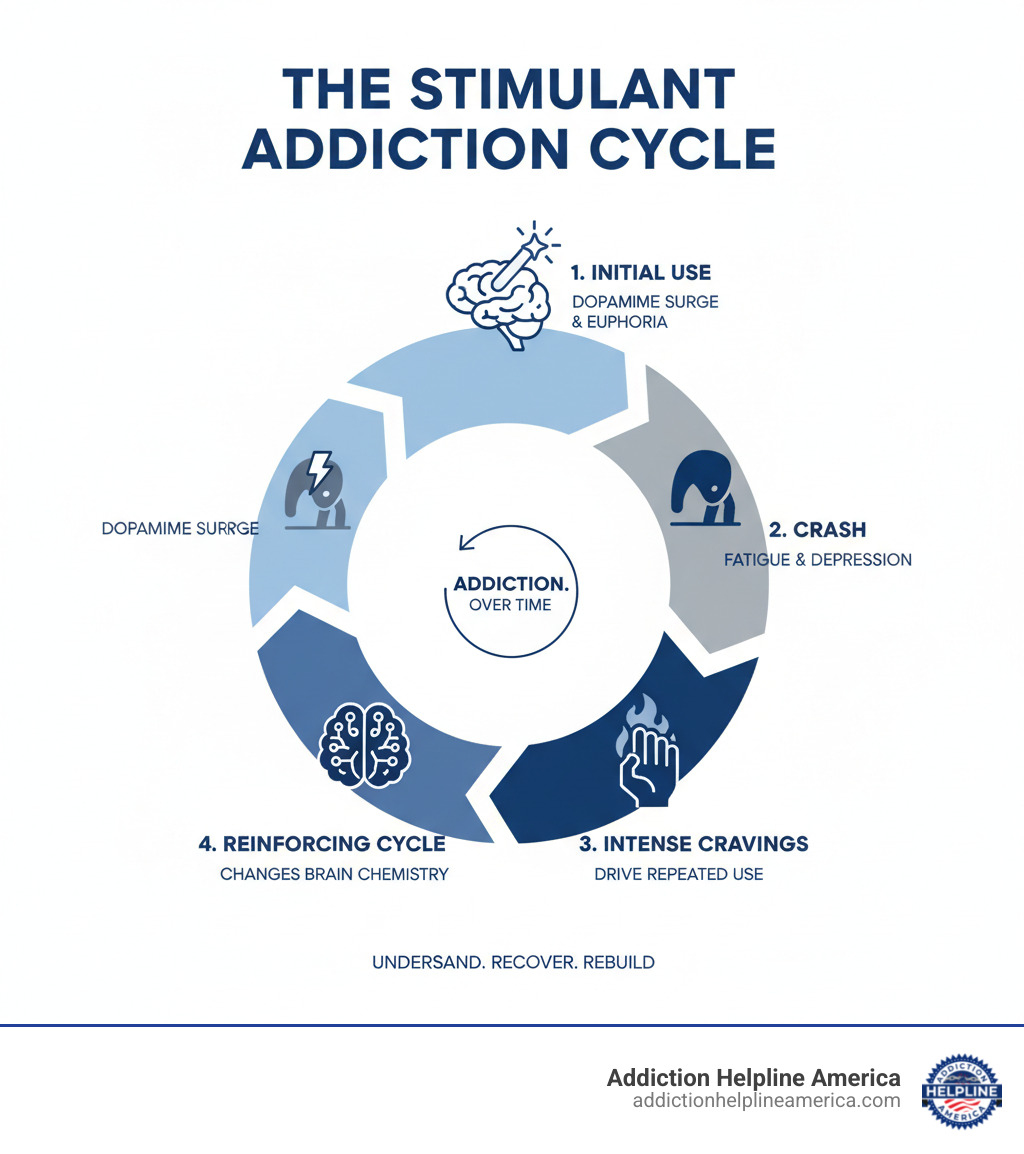
How Stimulants Affect the Brain’s Reward System
Stimulants accelerate the central nervous system (CNS), causing a rapid release of brain chemicals like dopamine. Dopamine is the brain’s “feel-good” messenger, crucial for pleasure and motivation. The intense dopamine rush from stimulants creates feelings of euphoria and high energy.
Over time, the brain adapts to these high dopamine levels, a process called neuroadaptation. It begins to rely on the drug for pleasure, diminishing the joy from everyday activities and leading to powerful cravings.
-
Short-term effects: Users experience increased heart rate, breathing, and blood pressure, followed by a hard “crash” marked by extreme fatigue, irritability, and intense cravings.
-
Long-term effects: Chronic use can cause serious health issues, including heart attacks and strokes. Mental effects can include paranoia, hallucinations, and mood swings. Brain structure can also change, impairing decision-making and emotional control.
Mixing stimulants with other substances (polysubstance use) is extremely dangerous. For instance, 71.2% of stimulant overdoses also involve an opioid. A stimulant can mask the sedative effects of an opioid, leading to a fatal overdose.
Common Stimulants of Misuse: From Cocaine to Prescription Pills
Stimulants come in both illegal and prescription forms. The most commonly misused include:
-
Cocaine: A powerful stimulant from the coca plant, sold as a white powder or as “crack” cocaine.
-
Amphetamines (including Methamphetamine): A group of highly addictive synthetic stimulants, including methamphetamine (“meth”).
-
Prescription Stimulants: Medications like Adderall, Ritalin, and Vyvanse, prescribed for ADHD but often misused for performance improvement or euphoria. In 2020, about 758,000 people had a prescription stimulant use disorder.
-
MDMA (Ecstasy/Molly): Known for its psychedelic properties, MDMA also acts as a stimulant, increasing energy and altering mood.
In the past year, 10.3 million people in the U.S. misused a central nervous system stimulant.
Recognizing the Signs and Symptoms of a Use Disorder
Spotting the signs of stimulant use disorder (StUD) is the first step toward getting help. These signs can be physical, behavioral, or psychological.
Physical Signs:
- Dilated pupils and rapid speech.
- Significant weight loss due to decreased appetite.
- Twitches, tremors, or dental problems (“meth mouth”).
- Sleep problems like insomnia followed by excessive sleep (hypersomnia).
Behavioral Signs:
- Neglecting responsibilities at work, school, or home.
- Secrecy or lying about drug use.
- Risky or impulsive behavior.
- Financial problems and social withdrawal.
Psychological Signs:
- Intense cravings.
- Severe mood swings, irritability, or agitation.
- Paranoia, hallucinations, or delusions.
- Anxiety and depression, especially during withdrawal.
A formal diagnosis of StUD is made if someone shows at least two of eleven specific signs over a 12-month period. These criteria revolve around impaired control, social impairment, risky use, and pharmacological indicators like tolerance and withdrawal. Recognizing these signs is a critical step toward seeking professional stimulant addiction treatment.
The Pillars of Stimulant Addiction Treatment
Knowing where to start with stimulant addiction treatment can feel overwhelming, but there is a proven path. The right combination of medical support, therapy, and care setting makes all the difference.
Starting with Safe Withdrawal Management (Detox)
When you stop using stimulants, your body goes through withdrawal, often called the “crash.” This first step in treatment, known as detox, addresses the physical dependence.
Symptoms include profound fatigue, severe depression (which can be dangerous), and intense cravings. You may also experience anxiety, paranoia, sleep disturbances, and a sharp increase in appetite. Because of these risks, medical supervision during detox is crucial. Professionals can monitor your health, keep you safe, and manage discomfort in a structured environment.
However, detox alone is not a complete treatment. It clears the drug from your system but doesn’t address the underlying psychological aspects of addiction. Without follow-up behavioral therapies, relapse is common. The real work of recovery begins after detox.
Core Behavioral Therapies: CBT and Contingency Management
Once you are medically stable, behavioral therapies provide the tools for long-term sobriety.
Cognitive Behavioral Therapy (CBT) helps you rewire your thinking. In CBT, you work with a therapist to identify personal triggers—people, places, or emotions—that lead to cravings. You then learn practical coping skills to manage these triggers in healthier ways. CBT teaches you to challenge the negative thought patterns that fuel addiction, creating lasting change by showing the connection between your thoughts, feelings, and behaviors.
Contingency Management (CM) is another powerful approach with strong scientific backing for treating stimulant use disorder. The concept is simple: it provides incentive-based rewards for positive behaviors. When you attend counseling or provide a drug-free urine sample, you might earn a gift card or voucher. Research shows that CM programs are highly effective because they retrain the brain’s reward pathways, redirecting them toward healthy actions.
Combining CBT and CM attacks addiction from two angles: CBT changes how you think, while CM reinforces positive actions. Together, they form a powerful foundation for recovery.
Choosing the Right Level of Care: Inpatient vs. Outpatient
Treatment intensity should match your unique needs. Factors like the severity of use, co-occurring mental health conditions, and your home environment determine the best level of care.
-
Inpatient/Residential Treatment: Provides 24/7 care in a live-in facility for 30-90 days. It’s best for severe addiction, dual diagnosis cases, or unsupportive home environments.
-
Partial Hospitalization (PHP): A “day treatment” option where you attend intensive therapy 5-7 days a week but return home at night. It’s a step down from inpatient care.
-
Intensive Outpatient (IOP): Offers more flexibility, with treatment 3-5 days a week for a few hours at a time. This allows you to maintain work or family commitments.
-
Standard Outpatient Treatment: The least intensive option, involving regular counseling sessions (e.g., once or twice a week) while you live at home.
The continuum of care model allows you to transition through these levels as you progress in recovery. At Addiction Helpline America, we connect people nationwide with facilities offering the right level of care, ensuring your treatment plan is custom to your specific needs.
The Future of Treatment: Research and Innovation
The landscape of stimulant addiction treatment is constantly evolving. While current behavioral therapies are powerful, scientists are working to develop new tools to make recovery even more effective.
Ongoing Research into New Approaches for Stimulant Use Disorder
Currently, there are no FDA-approved medications specifically for treating stimulant use disorder. Unlike opioid addiction, where medications are a key part of treatment, this pharmacological gap for stimulants makes ongoing research critical.
Scientists are investigating various compounds that could reduce cravings, block euphoric effects, or ease withdrawal. The goal is not to replace effective behavioral therapies like CBT and CM, but to complement them and provide additional support for recovery.
Challenges in Developing New Treatments
Developing medications for stimulant addiction is difficult for several reasons. The complexity of the dopamine system makes it hard to modify without causing side effects or new dependencies. High dropout rates in clinical trials, often exceeding 50%, make it challenging to gather conclusive data. Furthermore, widespread polysubstance use complicates research, as it’s hard to isolate the effects of an experimental medication when other drugs are present.
However, a recent shift by the FDA to recognize “use reduction” as a valid clinical outcome (in addition to complete abstinence) may open new pathways for medication approval.
Innovative Therapeutic Approaches for Stimulant Addiction Treatment
Despite the challenges, researchers are exploring several promising new approaches:
-
Medications targeting other neurotransmitter systems: The combination of naltrexone (an opioid antagonist) and bupropion (an antidepressant) has shown promise for methamphetamine use. Modulators of the GABA system are also being studied to reduce cravings.
-
Psilocybin-assisted psychotherapy: The psychedelic compound is being investigated in controlled therapeutic settings for its potential to treat various substance use disorders, including methamphetamine addiction.
-
Novel molecular targets: Researchers are looking at inhibitors that could disrupt drug-associated memories and prevent relapse.
-
Immunotherapies: Monoclonal antibodies and vaccines are being developed to train the immune system to neutralize stimulant molecules in the bloodstream before they can reach the brain, preventing the high.
These research avenues offer hope for future pharmacological tools to improve stimulant addiction treatment. While we await these innovations, Addiction Helpline America connects people with programs using today’s most effective evidence-based methods.
Building a Comprehensive and Lasting Recovery
Recovery from stimulant addiction is about rebuilding your entire life, not just stopping drug use. Successful stimulant addiction treatment programs provide comprehensive support that extends beyond therapy sessions.
The Power of Peer Support and Recovery Groups
Connecting with people who understand your struggle is incredibly powerful. Isolation can be overwhelming in recovery, but peer support changes everything.
Peer support groups like Narcotics Anonymous (NA) or SMART Recovery offer safe, non-judgmental communities where you can share your experiences. Hearing from others who have walked a similar path provides a unique form of hope and encouragement. These recovery communities help counter the loneliness that often fuels addiction.
Peer support specialists, who have their own lived recovery experience, offer mentorship and practical guidance. Research shows that engaging with peer support significantly increases the likelihood of long-term sobriety.
Integrating Holistic Therapies and Family Support
Effective treatment addresses the whole person—mind, body, and relationships.
Holistic therapies complement traditional treatment by promoting overall well-being. Mindfulness and meditation teach you to manage difficult emotions, while yoga and exercise reduce stress and provide a healthy, natural dopamine boost. Nutritional counseling is also vital, as it helps repair the physical damage caused by stimulant misuse and supports better brain function.
Family therapy is crucial because addiction affects the entire family system. It provides a space to rebuild trust, improve communication, and teach loved ones how to support recovery without enabling destructive behaviors. Your family members also need support to heal from the stress and trauma of a loved one’s addiction.
Addressing practical life challenges is also key. Stable housing and employment services provide a foundation of security and purpose. Rebuilding positive social connections that don’t revolve around drug use is essential for a fulfilling, sober life.
Finally, managing any co-occurring health issues, such as depression or anxiety, is critical. Treating both the addiction and mental health challenges simultaneously through an integrated approach dramatically improves the chances of lasting recovery. At Addiction Helpline America, we connect you with programs that understand this comprehensive model.
Frequently Asked Questions about Stimulant Addiction Treatment
When considering help for stimulant addiction, it’s natural to have questions. Here are honest answers to some common concerns.
How long does treatment for stimulant addiction take?
There is no one-size-fits-all timeline for stimulant addiction treatment. The journey is unique to each individual.
Most people begin with an initial program lasting 30 to 90 days, such as an inpatient stay or an intensive outpatient program. This phase builds a solid foundation of coping skills.
However, it’s crucial to understand that recovery is a lifelong process of management, similar to a chronic health condition like diabetes. After the initial program, many people transition through a continuum of care, stepping down to less intensive support over time. This ongoing approach is what makes treatment effective in the long term.
Is relapse a sign of failure?
Absolutely not. Relapse is not a sign of failure.
Stimulant addiction is a chronic disease, and setbacks can be part of the recovery process. A relapse doesn’t erase your progress; it indicates that your treatment plan may need adjustment. It can be a learning experience, revealing unknown triggers or areas where more support is needed.
The most important thing is to reach out for help immediately. Don’t let shame keep you from getting back on track. We’ve helped thousands of people steer these moments and are here 24/7 to help you too.
Can you treat stimulant addiction and a co-occurring disorder (like depression) at the same time?
Yes, and you absolutely should. Treating both simultaneously dramatically improves outcomes.
Co-occurring mental health conditions like depression, anxiety, and trauma are very common with stimulant addiction. The substance use and mental health symptoms are often intertwined. Trying to treat one without the other is like bailing out a boat while ignoring a hole in the bottom.
Dual diagnosis or integrated treatment addresses both the stimulant use disorder and the mental health condition at the same time. This holistic approach recognizes you as a whole person, leading to a much higher chance of achieving lasting, stable recovery.
Conclusion: Your Path to Recovery Starts Here
If you’ve made it this far, you’ve learned that stimulant addiction treatment works and recovery is real. We’ve seen how behavioral therapies help people reclaim their lives and how promising research is opening new doors.
The truth is simple: Behavioral therapies like Contingency Management and Cognitive Behavioral Therapy are proven approaches that give you practical tools to manage cravings and rebuild your life. While we await new medications, these evidence-based methods are already helping thousands.
Here’s what matters most: recovery from stimulant use disorder is not just possible—it happens every single day. People who once felt trapped by stimulants are now living full, meaningful lives. With the right support and personalized care, you or your loved one can be one of those success stories.
At Addiction Helpline America, we’ve spent years building relationships with trusted treatment providers across the entire country—from Pennsylvania to Wyoming, from Maine to California. We offer free, confidential guidance because we believe everyone deserves a clear path forward. Our team takes the time to understand your unique situation, then connects you with programs that truly match your needs. We’re not here to push you toward any particular option. We’re here to help you find the right one.
Your path to recovery doesn’t have to wait. We’re ready when you are.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.