
Why Effective Depression Interventions Matter
Interventions for depression are evidence-based treatments that help individuals reclaim their lives. The World Health Organization calls depression a leading cause of disability globally, but the encouraging truth is that it’s treatable, and recovery is possible.
Quick Overview: Main Types of Depression Interventions
- Psychotherapy – Talk-based treatments like Cognitive Behavioral Therapy (CBT), Interpersonal Therapy (IPT), and Behavioral Activation
- Medication – Antidepressants including SSRIs, SNRIs, and other classes that help balance brain chemistry
- Lifestyle Changes – Exercise, nutrition, sleep improvement, and mindfulness practices
- Brain Stimulation – Electroconvulsive Therapy (ECT) and Transcranial Magnetic Stimulation (TMS) for severe or treatment-resistant cases
- Support Services – Guided self-help, support groups, and crisis intervention resources
Depression impairs quality of life, work, and relationships. Fortunately, multiple effective interventions for depression exist, and most people benefit from treatment. Appropriate interventions can help you recover, regardless of symptom severity.
This guide covers the full spectrum of treatments, from first-line approaches to advanced interventions. You’ll learn about psychotherapy, medication, lifestyle changes, and specialized treatments.
At Addiction Helpline America, we help individuals and families steer mental health challenges. Our team provides compassionate, evidence-based guidance 24/7 to connect you with the right interventions for depression for your situation.
Interventions for depression terms you need:
- bipolar depression treatment
- depression and anxiety therapist near me
- outpatient depression treatment centers near me
If You Need Immediate Help
If you’re having thoughts of suicide or self-harm, know that these feelings are temporary, even if they don’t feel that way. Suicidal thoughts are a symptom of depression, not a character flaw, and they require immediate attention.
You don’t have to face this alone. Crisis support is available 24/7.
Go to your nearest emergency room if you’re in immediate danger. Hospital staff are trained to help keep you safe. If you can’t get there yourself, call 911.
Call the National Suicide Prevention Lifeline at 1-800-273-8255 to speak with a trained crisis counselor who will listen without judgment and help you find ways to stay safe.
Contact Addiction Helpline America for immediate support at any time. Our team can connect you with resources and professionals who care about your wellbeing. We’re here to help you through this difficult moment.
Depression distorts your thinking, but recovery is possible. We’ve seen countless people recover and rebuild their lives with effective interventions for depression. You matter, and support is available to guide you through this.
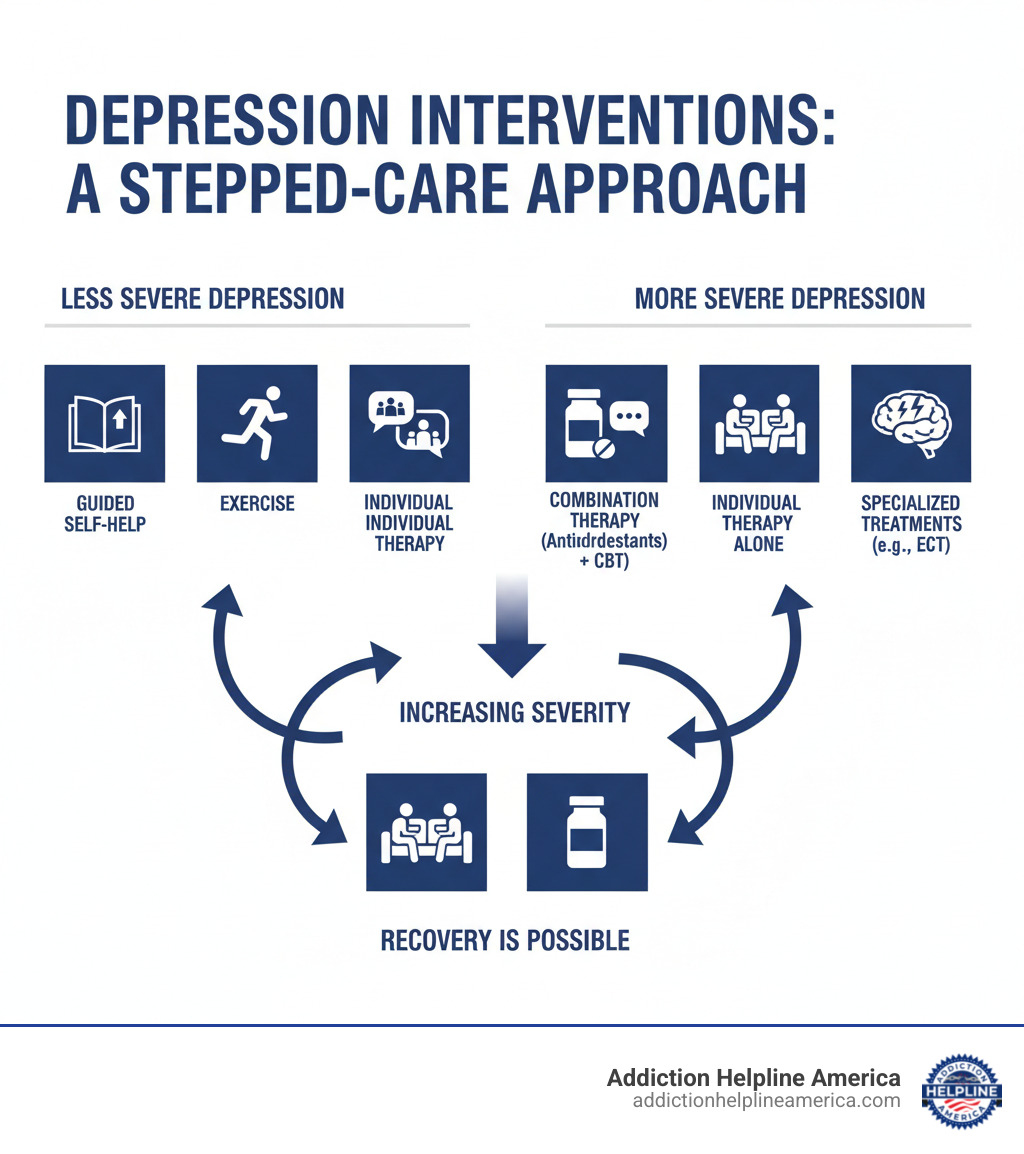
Understanding Depression Treatment Pathways
There’s no single “correct” way to treat depression. Effective interventions for depression must be personalized to your unique situation, symptom severity, and personal preferences.
Most providers follow a “stepped-care” model, starting with the least intensive treatment that matches your needs and “stepping up” to more comprehensive care if necessary. This practical approach ensures you get the right level of support.
Clinical guidelines help professionals recommend the most effective treatments for each situation. At Addiction Helpline America, we offer free, confidential guidance to help you understand these options.
First-Line Approaches for Mild Depression
For less severe depression, gentler approaches are often highly effective and can prevent symptoms from worsening.
- Wait and see approach: For very mild symptoms, a doctor may suggest monitoring with regular check-ins, paired with self-care strategies.
- Guided self-help: These structured programs use workbooks or online modules with professional support over 6-8 sessions to teach mood management strategies.
- Exercise: Research shows just one hour of physical activity per week can help. A daily walk, bike ride, or even dancing at home can make a difference. Movement matters more than intensity.
- Supportive counseling: Brief problem-solving therapies provide a safe space to develop better coping skills.
Recommended Approaches for Moderate to Severe Depression
When symptoms severely disrupt daily life, more intensive interventions for depression are needed to achieve remission and prevent relapse.
- Antidepressant medication: This is an important option that works by balancing brain chemistry that influences mood.
- Combination therapy: Pairing medication with psychotherapy is often the most effective approach, as it addresses both the biological and psychological aspects of depression.
- Psychotherapy: Treatment is more intensive, often involving weekly sessions of evidence-based therapies like Cognitive Behavioral Therapy (CBT) or Interpersonal Therapy (IPT).
- Referral to mental health professionals: For complex cases, a specialized team (psychologists, psychiatrists, etc.) can provide comprehensive assessment and treatment planning.
The Power of Talk: Psychotherapy for Depression
Psychotherapy, or “talk therapy,” is one of the most effective interventions for depression. Working with a mental health professional in a safe environment helps you explore thoughts, feelings, and behaviors. It’s highly effective for maintaining remission and preventing relapse.
Therapy teaches you to cope with difficulties, identify negative beliefs, explore relationship dynamics, and regain a sense of control. If you’re curious about what therapy might look like for you, you can learn more about therapy options at Addiction Helpline America.
Cognitive Behavioural Therapy (CBT)
CBT is a widely recognized therapy based on the connection between our thoughts, feelings, and behaviors. By changing unhelpful thought patterns, your emotional state can improve. A key part is recognizing “cognitive distortions”—unhelpful thought patterns that reinforce negative emotions.
In CBT, you’ll learn practical techniques like using a thought diary to spot patterns, identifying unhelpful thinking styles (like all-or-nothing thinking), and challenging negative thoughts to produce more balanced ones. It also addresses core beliefs that fuel negative thinking. A typical course of CBT lasts between 8 and 16 sessions. To learn more, you can explore recognizing cognitive distortions.
Interpersonal Therapy (IPT)
IPT is an evidence-based therapy focusing on the link between your mood and your relationships. It is particularly helpful if depression is linked to relationship issues or major life changes, such as grief, role disputes, or life transitions. By improving interpersonal skills and communication, IPT reduces depressive symptoms and builds stronger social support. It typically involves 8 to 16 sessions.
Other Effective Psychotherapy Interventions for Depression
Several other psychotherapies have proven highly effective.
- Behavioural Activation (BA): This therapy focuses on increasing engagement in rewarding activities to improve mood, based on the principle that action can precede motivation and create positive change. It usually involves 12 to 16 sessions.
- Acceptance and Commitment Therapy (ACT): ACT teaches you to accept difficult thoughts and feelings while committing to actions aligned with your personal values.
- Mindfulness-Based Cognitive Therapy (MBCT): MBCT combines cognitive therapy with mindfulness to help you observe thoughts without judgment, which is effective in preventing relapse.
- Psychodynamic Psychotherapy: This therapy digs into unconscious thoughts and past experiences to improve self-awareness and understand how they affect your current behavior. It often involves 8 to 16 sessions.
- Supportive Therapy: This intervention provides a supportive relationship where empathy and listening help you build coping skills.
- Group Therapy: This format offers the added benefit of peer support, reducing isolation and allowing members to learn from shared experiences.
A Closer Look at Medical Interventions for Depression
Medication (pharmacotherapy) is a crucial and effective intervention for depression, especially for moderate to severe cases. Antidepressants work by influencing neurotransmitters—chemical messengers that regulate mood.
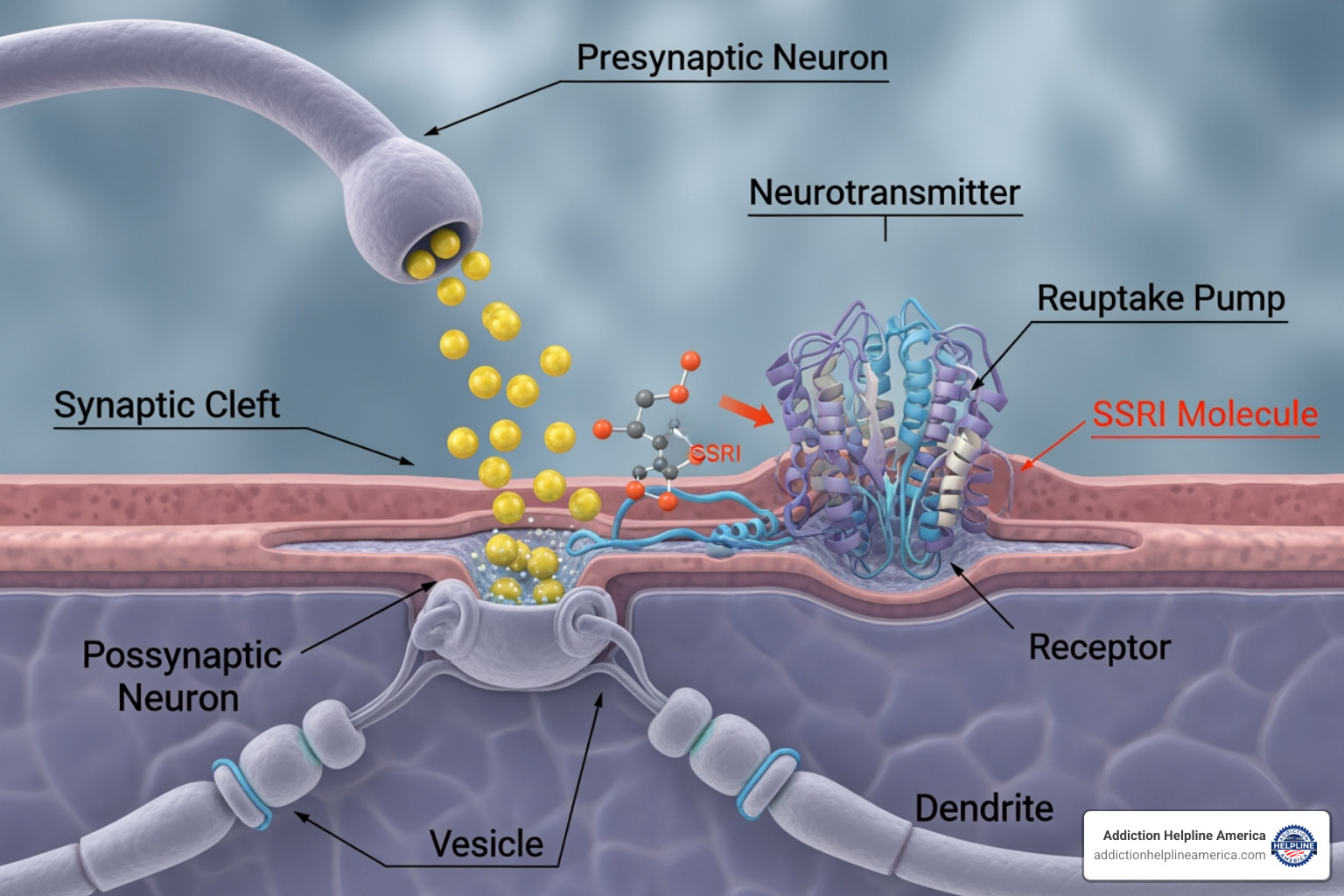
Modern “second-generation” antidepressants are generally better tolerated than older medications. Doctors choose a medication based on its potential side effects and your individual needs. For many, antidepressants provide the stability needed to fully engage in other treatments like psychotherapy.
How Antidepressants Work and Key Classes
Antidepressants adjust chemical signals in the brain, primarily involving serotonin, norepinephrine, and dopamine.
- Selective Serotonin Reuptake Inhibitors (SSRIs): Often the first choice, SSRIs are safer and have fewer side effects. They increase levels of serotonin, a mood-regulating chemical. Common examples include fluoxetine, sertraline, and citalopram.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): These increase both serotonin and norepinephrine. Examples include duloxetine (Cymbalta) and venlafaxine (Effexor XR).
- Atypical Antidepressants: This class works through various mechanisms. Bupropion (Wellbutrin) affects norepinephrine and dopamine, while mirtazapine (Remeron) can help with sleep. Others include trazodone and vortioxetine (Trintellix).
- Tricyclic Antidepressants (TCAs): While effective, this older class (e.g., imipramine, nortriptyline) has more significant side effects than newer drugs.
- Monoamine Oxidase Inhibitors (MAOIs): Typically used when other treatments fail, MAOIs (e.g., tranylcypromine) are powerful but require strict dietary restrictions to avoid dangerous interactions.
Potential Side Effects and Risks of Medication
Working closely with your doctor is essential to manage potential side effects. Common side effects of SSRIs/SNRIs include nausea, insomnia, and sexual dysfunction. TCAs more often cause dry mouth, constipation, and drowsiness.
While not addictive, stopping antidepressants suddenly can cause antidepressant discontinuation syndrome (withdrawal-like symptoms). Your doctor will guide a gradual tapering process.
Common Side Effects: SSRIs vs. TCAs
| Side Effect | SSRIs (Newer) | TCAs (Older) |
|---|---|---|
| Nausea | Common | Less common |
| Sexual Dysfunction | Common | Common |
| Weight Gain | Possible | More common |
| Drowsiness | Possible | Common |
| Dry Mouth | Possible | Very common |
| Blurred Vision | Less common | Common |
| Constipation | Less common | Common |
| Dizziness | Possible | Common |
| Heart Problems | Rare | More common (e.g., arrhythmias) |
| Overdose Risk | Lower, but still serious | Higher, potentially fatal |
The FDA requires a black box warning for increased suicide risk in young adults under 25; contact your doctor immediately if this occurs. Discuss risks with your doctor if you are pregnant, planning pregnancy, or breastfeeding. Always disclose all medications and supplements to avoid dangerous drug interactions, such as with St. John’s wort. Some medications like lithium require regular blood tests to monitor for toxicity.
When Standard Treatments Aren’t Enough
For treatment-resistant depression, more advanced interventions for depression are available.
- Brain Stimulation Therapies: These therapies stimulate the brain to improve mood.
- Electroconvulsive Therapy (ECT): This is the most effective treatment for severe, treatment-resistant, or psychotic depression. It involves a controlled electrical current that induces a brief seizure, altering brain chemistry.
- Transcranial Magnetic Stimulation (TMS): A non-invasive option that uses magnetic fields to stimulate mood-regulating nerve cells in the brain.
- Vagus Nerve Stimulation (VNS): Uses an implanted device to send electrical pulses to the brain via the vagus nerve, for long-term, treatment-resistant depression.
- Deep Brain Stimulation (DBS): A surgical procedure where electrodes are implanted in the brain, reserved for the most severe cases.
- Ketamine and Related Molecules: Ketamine and its derivative, esketamine, offer rapid relief for treatment-resistant depression by working on the glutamate system. These treatments require strict medical supervision.
- Augmentation Strategies: This involves adding another medication (like lithium or an atypical antipsychotic) to an antidepressant to boost its effectiveness.
If you’re exploring these advanced options, Contact Addiction Helpline America for advanced depression care to connect with specialists.
Building Resilience: Lifestyle and Self-Care Strategies
Daily lifestyle choices are powerful interventions for depression that complement professional treatment. These self-care strategies build a foundation for recovery and reinforce your self-worth.

The Role of Exercise and Nutrition
- Exercise: Even moderate physical activity, like a daily walk, is a potent mood-booster. It’s important to engage in activity even when you don’t feel like it, as action can shift your mood.
- Sleep: Depression disrupts sleep. Prioritize a consistent sleep schedule and a relaxing bedtime routine in a peaceful environment to get restorative rest.
- Nutrition: Eating nourishing foods like fruits, vegetables, and lean proteins provides your brain with essential fuel. While tempting, highly processed comfort foods don’t support long-term recovery.
- Avoid Alcohol and Drugs: Alcohol is a depressant that worsens symptoms and complicates treatment. Avoiding alcohol and recreational drugs is critical for recovery.
Mindfulness, Relaxation, and Positive Mindset
- Mindfulness: This practice involves paying attention to the present moment without judgment, which helps break cycles of negative thinking. The structured approach of Mindfulness-Based Cognitive Therapy (MBCT) is proven to reduce relapse.
- Relaxation Techniques: Deep breathing, meditation, and progressive muscle relaxation are powerful tools to manage stress and reduce ruminating thoughts.
- Mantras: Repeating short, positive statements like “This feeling will pass” can help shift automatic thought patterns over time.
- Uplifting Distractions: Engaging in hobbies, watching funny movies, or spending time in nature gives your brain a necessary break and reminds you that joy is possible.
Complementary and Alternative Approaches
Some people find complementary approaches helpful, but always consult your doctor first.
- Omega-3 Fatty Acids: Found in foods like salmon and walnuts, these may support mood and offer other health benefits.
- Supplements: Be cautious with supplements like St. John’s wort and SAMe. They are not FDA-regulated for depression in the U.S., and their quality varies. St. John’s wort can have dangerous interactions with prescription medications.
- Consult Your Doctor: Always talk to your doctor before starting any supplement, as “natural” does not always mean safe, especially when combined with other treatments.
Navigating Your Recovery and Future Directions
Recovery from depression is a non-linear journey requiring patience and persistence. You don’t have to do it alone. Professional guidance is crucial, as a depressed brain can’t be a neutral party in its own recovery.
For many, combination therapy (medication plus psychotherapy) is most effective, addressing both biological and psychological factors for better, more sustained outcomes. At Addiction Helpline America, we help you understand these options. Learn more about depression treatment options at Addiction Helpline America.
Challenges in Depression Treatment
- Treatment Resistance: Some people don’t respond to initial treatments. This means your depression requires a different approach, which may take time and persistence to find.
- Finding the Right Intervention: With so many options, personalized guidance from mental health professionals is invaluable for recommending the most appropriate starting point.
- Adherence to Treatment: Depression can sap motivation, making adherence difficult. Education, support systems, and a good relationship with your provider are crucial.
- Access to Services: Barriers like location and insurance can be frustrating. Addiction Helpline America helps break down these barriers by connecting people to care in states across the US.
The Future of Interventions
The field of depression treatment is constantly evolving.
- Emerging Therapies: Researchers are exploring new brain pathways, like the glutamate system, and neurotrophic factors, offering hope for those with treatment-resistant depression.
- Personalized Medicine: This exciting frontier aims to use genetic testing and brain imaging to identify biomarkers that match patients to the most effective interventions for depression, reducing the current trial-and-error process.
- Ongoing Research: Current research focuses on developing new medications with fewer side effects, refining psychotherapies, and improving brain stimulation methods. Research also focuses on simplifying therapies for delivery in primary care, increasing accessibility.
The future of depression treatment is bright. As research advances, more people will find relief faster and with fewer setbacks.
Conclusion
Depression is treatable, and you have options. This is the reality we see daily at Addiction Helpline America. While depression is a common psychiatric disorder that can disrupt your life, effective interventions for depression work.
Successful treatment often combines multiple approaches, such as therapy, medication, and lifestyle changes. This comprehensive strategy addresses depression from all angles and offers the best chance for lasting recovery.
Recovery isn’t linear and may require trying different medications or therapies. This is a normal part of the process, not a sign of failure. It means you’re doing the work, and that work is worth it.
You don’t have to figure this out alone. At Addiction Helpline America, we provide free, confidential, personalized guidance to connect you with the right treatment centers and mental health professionals across the country—from Alabama to Wyoming. We understand that finding help can feel overwhelming, and we’re here to make it easier.
Find personalized depression treatment support today. Take that first step. Your future self will thank you.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.












