Understanding Your Options for a Drug for Anxiety and Depression
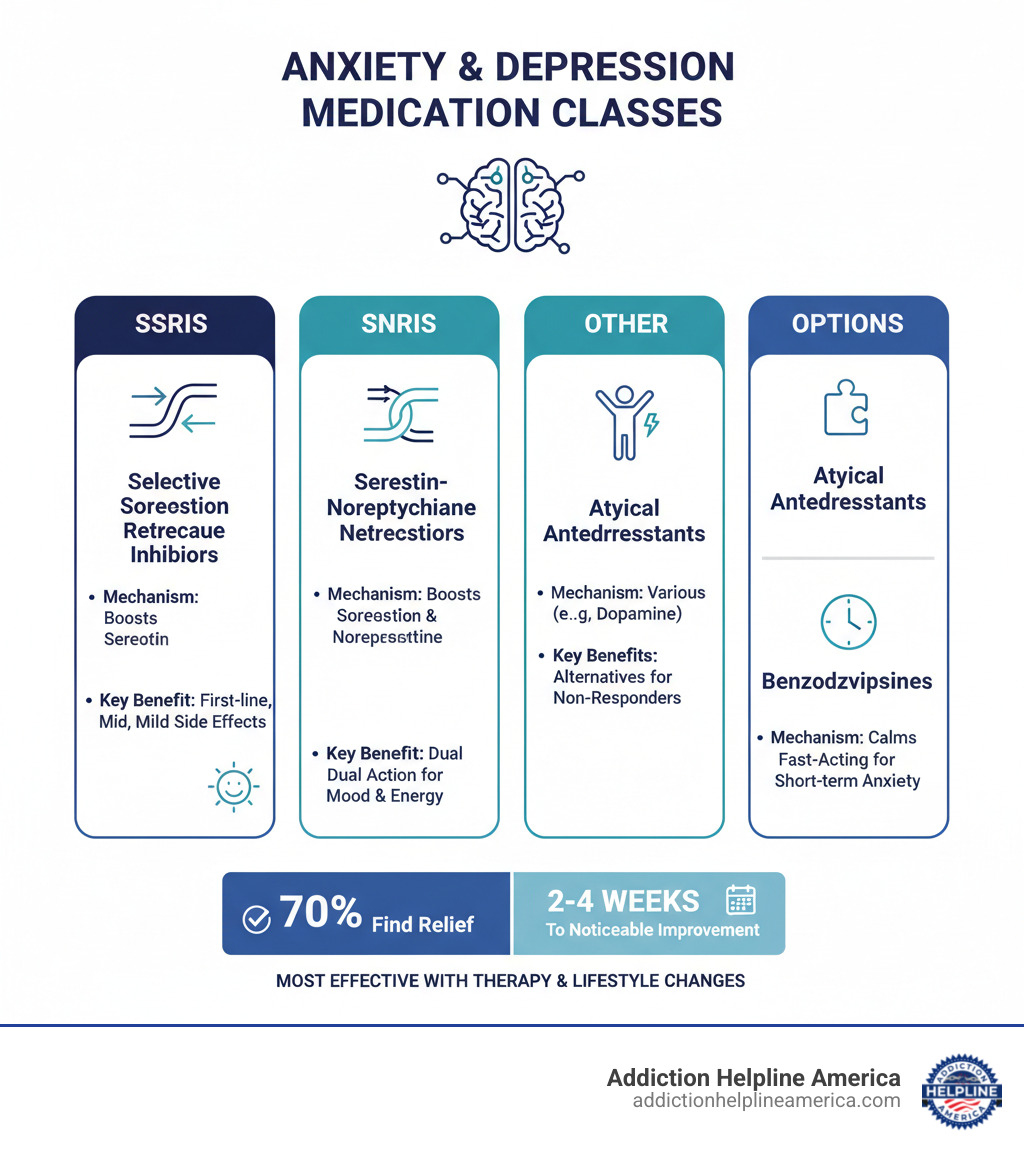
A drug for anxiety and depression can be a crucial tool for managing these often co-occurring conditions. The main medication options include:
Primary Drug Classes:
- SSRIs (Selective Serotonin Reuptake Inhibitors) – First-line treatment with milder side effects (e.g., Prozac, Zoloft, Lexapro)
- SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors) – Dual-action medications for depression and anxiety (e.g., Effexor, Cymbalta)
- Atypical Antidepressants – Alternative options like Wellbutrin for those who don’t respond to SSRIs
- Benzodiazepines – Fast-acting anti-anxiety medications for short-term use (e.g., Xanax, Ativan)
Key Facts:
- Up to 70% of people find symptom relief with antidepressants
- Around 45% of people with major depression also experience anxiety disorders
- Medications typically take 2-4 weeks to show noticeable improvement
- Most effective when combined with therapy and lifestyle changes
Depression and anxiety often intertwine, but multiple medications can help restore balance to your brain chemistry. These drugs work by adjusting levels of neurotransmitters—like serotonin, norepinephrine, and dopamine—that regulate your mood, energy, and emotions.
Choosing the right medication is about finding what works for you. Your doctor will consider your symptoms, medical history, and potential side effects to find the best fit.
Medication alone is rarely the complete answer. Research shows that combining it with psychotherapy and lifestyle changes produces the best outcomes by addressing both brain chemistry and behavioral patterns.
At Addiction Helpline America, we help people steer the complexities of treating anxiety and depression. We connect individuals with comprehensive treatment programs, knowing that education and support are key to finding the right drug for anxiety and depression.
Drug for anxiety and depression vocabulary:
- bipolar depression treatment
- outpatient depression treatment centers near me
- can i refuse mental health treatment
Understanding How Medications for Anxiety and Depression Work
When considering a drug for anxiety and depression, it helps to understand how your brain’s chemistry works. Your brain uses chemical messengers called neurotransmitters to regulate everything from mood to sleep. The key neurotransmitters involved are serotonin, norepinephrine, and dopamine. An imbalance can lead to persistent sadness, overwhelming anxiety, or a lack of energy.
Most of these medications work by blocking neurotransmitter reuptake. Normally, after a neurotransmitter delivers its message, it’s reabsorbed. Antidepressants block this process, leaving more neurotransmitters available to send positive signals and restore brain chemistry balance.
These medications don’t work overnight. The time to effectiveness varies, but initial improvements like better sleep or energy may appear in a week or two. The full mood improvement timeline is typically two to four weeks, with some people needing six to twelve weeks for complete symptom remission. Patience and close contact with your provider are essential during this period.
Factors in Selecting a Drug for Anxiety and Depression
Choosing the right drug for anxiety and depression is a personalized process. Your doctor will partner with you, considering multiple factors to find the best medication for you.
- Symptom profile: Your specific symptoms, such as insomnia versus fatigue, help determine whether a sedating or activating medication is more appropriate.
- Side effect tolerance: An honest discussion with your doctor about which side effects are dealbreakers (e.g., nausea, sexual dysfunction) helps narrow the options.
- Co-existing conditions: Other health issues, like chronic pain or a heart condition, influence medication choice. Some SNRIs, for example, can treat both depression and pain.
- Family history: If a close relative responded well to a specific antidepressant, it might also work for you due to shared genetics, though it’s not a guarantee.
- Drug interactions: Your doctor needs to know all medications and supplements you take to avoid dangerous combinations, such as those leading to Serotonin Syndrome.
- Cost and insurance coverage: Many effective antidepressants are available as affordable generics. Your doctor can help find an option that fits your budget.
This selection process is ongoing. If the first medication doesn’t work, adjustments can be made. For more information on how treatment plans are personalized, check out this resource on Customized Treatment Plans.
Finding the right medication is a journey you don’t have to steer alone.
The Main Classes of a Drug for Anxiety and Depression
Understanding the different classes of medications for anxiety and depression can help you steer your treatment. Each class works differently to rebalance brain chemistry.
Doctors often start with SSRIs (Selective Serotonin Reuptake Inhibitors) because they are effective and have milder side effects. However, finding the right fit can take time. Antidepressants relieve symptoms in up to 70% of people, but it may require trying more than one medication. Close communication with your doctor is key to finding what works for your unique situation.
SSRIs (Selective Serotonin Reuptake Inhibitors)
SSRIs are a first-line drug for anxiety and depression because they are effective and well-tolerated. They work by increasing levels of serotonin, a neurotransmitter that regulates mood, sleep, and appetite, by blocking its reabsorption in the brain.
Common SSRIs include Fluoxetine (Prozac), Sertraline (Zoloft), Escitalopram (Lexapro), Citalopram (Celexa), and Paroxetine (Paxil).
Side effects are often mild and may include nausea, headaches, sleep disturbances, or changes in sex drive. Many of these fade as your body adjusts. For more details on a common SSRI, see this Information on Fluoxetine (Prozac).
SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors)
If SSRIs aren’t effective, SNRIs may be the next step. They have a dual-action mechanism, increasing both serotonin and norepinephrine. This can be especially helpful for symptoms like low energy and poor concentration.
Common SNRIs include Venlafaxine (Effexor), Duloxetine (Cymbalta), and Desvenlafaxine (Pristiq). A key benefit of some SNRIs, like Duloxetine, is their ability to also treat chronic pain conditions. Side effects are similar to SSRIs, but SNRIs can also increase blood pressure, which your doctor will monitor.
Other Antidepressant and Anti-Anxiety Classes
Beyond SSRIs and SNRIs, other medication classes offer valuable alternatives.
- Atypical antidepressants: These work in unique ways. Bupropion (Wellbutrin) affects dopamine and norepinephrine, making it a good option for those with fatigue or concerns about sexual side effects. It can also help with smoking cessation.
- Tricyclic Antidepressants (TCAs): This is an older class of medication. While effective, they have more side effects (like dry mouth, blurred vision, and drowsiness) and are usually not a first-line choice. They are sometimes used for chronic pain.
- MAOIs (Monoamine Oxidase Inhibitors): These were some of the first antidepressants. They are highly effective but require strict dietary restrictions to avoid dangerous blood pressure spikes. Due to these risks and numerous drug interactions, they are reserved for treatment-resistant cases.
- Benzodiazepines: Medications like Alprazolam (Xanax) and Lorazepam (Ativan) provide rapid relief for acute anxiety and panic attacks. However, they are prescribed for short-term use due to the risk of tolerance, physical dependence, and withdrawal. Long-term use can lead to cognitive impairment. If you’re concerned about dependence, Benzo Withdrawal Help is available.
Here’s a quick comparison of the main antidepressant classes:
| Class | Mechanism of Action | Common Side Effects | Key Considerations |
|---|---|---|---|
| SSRIs | Block serotonin reuptake | Nausea, insomnia, sexual dysfunction, weight changes | First-line treatment; generally well-tolerated; takes 2-4 weeks to work |
| SNRIs | Block serotonin and norepinephrine reuptake | Similar to SSRIs, plus potential blood pressure increase | Good for low energy and concentration issues; some help with chronic pain |
| TCAs | Block multiple neurotransmitter reuptake | Dry mouth, constipation, blurred vision, drowsiness | Older medication class; more side effects but effective; sometimes used for pain |
| MAOIs | Inhibit monoamine oxidase enzyme | Similar to TCAs, plus risk of hypertensive crisis | Requires strict dietary restrictions; used when other options fail; dangerous drug interactions |
Finding the right drug for anxiety and depression often involves some adjustment, but with patience and good communication, you can find what helps you feel like yourself again.
Managing Risks, Side Effects, and Interactions
Starting a drug for anxiety and depression requires understanding the risks and side effects to stay safe and empowered.
Maximizing effectiveness relies on three key principles: patience, as medications take weeks to work; open communication with your provider about any issues; and patient adherence, meaning you take the medication exactly as prescribed. Never adjust your dose or stop taking your medication without talking to your doctor first.
Common Side Effects and How to Manage Them
Many side effects are temporary and fade as your body adjusts. Here are some common ones and how to manage them:
- Nausea: A common initial side effect. Taking medication with food often helps, and it usually fades within a few weeks.
- Weight gain: Some antidepressants can affect appetite or metabolism. Discuss diet, exercise, or medication alternatives like Bupropion with your doctor.
- Drowsiness or insomnia: If a medication makes you tired, take it at bedtime. If it keeps you awake, take it in the morning. Avoid driving until you know how it affects you.
- Sexual dysfunction: A common side effect of SSRIs and SNRIs. Don’t hesitate to discuss this with your doctor; adjusting the dose or switching to a drug like Bupropion can help.
- Dry mouth: Stay hydrated, chew sugar-free gum, or use sugar-free candy for relief.
- Dizziness: Stand up slowly from a sitting or lying position to prevent dizzy spells.
If side effects are persistent or severe, your healthcare provider can help find solutions.
Understanding the Black Box Warning: Suicide Risk
The FDA requires a “black box warning” on antidepressants, its strongest advisory. It highlights an increased risk of suicidal thoughts or behavior in children, teens, and young adults (under 25), especially during the first few weeks of treatment or after a dose change.
This doesn’t mean the drugs cause suicide, but they can temporarily increase agitation before mood improves. Close monitoring is critical during this period. Watch for worsening depression, unusual behavior changes, or any thoughts of self-harm.
If you or someone you know experiences these symptoms, seek emergency help immediately. Call 911, go to the nearest emergency room, or call the National Suicide Prevention Lifeline at 988. For more information, see the Empirical justification for the antidepressant black box warning. Untreated depression also carries a significant suicide risk, which antidepressants ultimately help reduce for most people.
Interactions with Other Substances
What else you put in your body matters when taking a drug for anxiety and depression.
- Alcohol interactions: It’s generally not recommended. Alcohol is a depressant that can worsen symptoms and amplify side effects like drowsiness.
- Recreational drugs: This is a dangerous combination that can cause severe, unpredictable interactions and reduce your medication’s effectiveness. If you struggle with substance use, understanding the Causes of Drug Addiction can be a step toward recovery.
- Other medications: Always give your doctor a complete list of all prescriptions, over-the-counter drugs, and supplements you take. Even common items like St. John’s Wort can cause problems.
- Serotonin Syndrome: This is a potentially life-threatening condition from combining multiple drugs that raise serotonin levels. Symptoms include agitation, rapid heart rate, high blood pressure, and muscle rigidity. Seek emergency medical attention if you suspect it.
A Holistic Approach: Combining Medication with Therapy and Lifestyle Changes
A drug for anxiety and depression is just one piece of the recovery puzzle. Medication is most effective when combined with psychotherapy and lifestyle changes. This synergistic approach provides tools for long-term well-being.
The Crucial Role of Psychotherapy
Psychotherapy, or talk therapy, is a crucial component of treatment. It teaches practical skills for building resilience. Cognitive Behavioral Therapy (CBT) is highly effective for anxiety and depression, helping you identify and change negative thought patterns.
Research confirms that combining medication with psychotherapy yields better results than either treatment alone. While medication adjusts brain chemistry, therapy provides coping skills for lasting change. It’s a safe space to process emotions, understand the drivers of your symptoms, and build strategies to prevent relapse. For more information on different therapy approaches, NAMI on Psychotherapy offers excellent resources.
Lifestyle Changes to Support Your Mental Health
Daily choices can either amplify or undermine your progress. Small, sustainable lifestyle changes can make a big difference.
- Exercise: Regular physical activity, even a daily walk, releases mood-boosting endorphins, reduces stress, and improves sleep.
- Balanced diet: A diet rich in fruits, vegetables, and lean proteins, and low in processed foods, provides the brain with essential nutrients for optimal function.
- Sleep: Prioritize good sleep hygiene—like consistent sleep-wake times and a relaxing bedtime routine—as poor sleep worsens anxiety and depression.
- Stress management: Practices like deep breathing, meditation, and mindfulness can calm the nervous system and break the cycle of anxious or depressive thoughts.
- Connection: Building strong relationships with family, friends, or support groups provides crucial emotional support and combats the isolation that fuels mental health struggles. The Importance of Support Systems in recovery cannot be overstated.
When you combine the right medication with therapy and positive lifestyle habits, you’re not just managing symptoms—you’re building a healthier, more resilient life.
Your Treatment Journey: Common Questions Answered
It’s natural to have questions when starting treatment for anxiety and depression. Here are answers to some of the most common concerns.
How long will I need to take a drug for anxiety and depression?
The answer varies, but there are general guidelines. Once you feel better, most doctors recommend continuing the drug for anxiety and depression for at least six to twelve months. This maintenance phase is crucial to prevent relapse.
For those with recurrent episodes, longer-term treatment might be necessary to maintain stability, similar to managing other chronic conditions like high blood pressure. You and your doctor will decide on the right duration for your situation.
Are antidepressants addictive and how do I stop taking them?
Antidepressants are not addictive in the way substances like opioids are; they don’t cause cravings or a high. However, your body can develop a physical dependence, meaning you may experience withdrawal symptoms (discontinuation syndrome) if you stop abruptly. Symptoms can include dizziness, nausea, irritability, and “brain zaps.”
Never stop taking your medication cold turkey. Always work with your doctor to create a tapering plan. They will help you gradually reduce the dose over weeks or months to allow your brain to adjust and minimize withdrawal symptoms. For a comprehensive guide, Harvard Health provides excellent information on going off antidepressants.
What are the considerations for children, teens, and during pregnancy?
Treating anxiety and depression in these groups requires extra care and thoughtful decision-making.
- For children and teens, psychotherapy is the first-line treatment. Medication may be considered for severe cases, but it requires close monitoring due to the black box warning about increased suicide risk in people under 25.
- During pregnancy and while breastfeeding, the decision is a careful balance of risks and benefits. Untreated maternal depression can pose risks to both mother and baby. While some medications carry potential risks, many women use them safely during pregnancy. Your doctor will help you weigh the options.
- For breastfeeding mothers, most antidepressants pass into breast milk in very small amounts. However, this decision should also be made with your doctor, considering your baby’s health and age.
Reaching out for professional guidance is a sign of strength. At Addiction Helpline America, we can connect you with the resources and support you need for these important decisions.
Conclusion: Finding the Right Path to Recovery
Navigating your options for a drug for anxiety and depression can feel complex, but remember: you are not alone, and recovery is possible. We’ve seen that the most effective treatment combines medication (like SSRIs or SNRIs) with psychotherapy and healthy lifestyle changes.
There is no one-size-fits-all solution. Finding the right path is a personal journey that requires patience and open communication with your healthcare provider. The most important step is reaching out for that professional guidance.
At Addiction Helpline America, we understand this journey. We provide free, confidential, and personalized guidance to connect you with the right treatment program from our extensive network. We don’t believe in one-size-fits-all solutions because we know your story is unique.
If you or a loved one is struggling with anxiety and depression, don’t wait. Recovery is possible, and you deserve support. Reach out today and Find personalized help for mental health. Let us help you find the path to a brighter, more balanced tomorrow.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.