Why Inpatient Rehab for Depression Offers Hope for Recovery
Inpatient rehab for depression is a residential program providing intensive, 24/7 care for severe depression. It’s designed for individuals with debilitating symptoms, suicidal thoughts, or for whom outpatient treatment has not been effective.
Key Features of Inpatient Rehab:
- 24/7 medical supervision and crisis support in a safe, structured environment
- Intensive therapy schedule including individual, group, and family sessions
- Medication management with real-time adjustments by psychiatrists
- Treatment for co-occurring disorders like addiction or anxiety
- Duration typically ranges from 30-90 days for comprehensive treatment
- Evidence-based therapies like CBT and DBT, plus holistic approaches
Depression rates have surged in recent years, affecting millions. It’s crucial to remember that depression is a treatable medical condition, not a character flaw or a lack of willpower.
Inpatient programs are the most intensive form of depression treatment. They remove you from daily triggers, allowing you to focus entirely on healing in a supportive environment. Unlike weekly therapy, this immersive approach is highly effective for those with severe symptoms who may be a danger to themselves.
Recovery is possible. This guide will walk you through what to expect from inpatient rehab for depression and how to find the right program.
At Addiction Helpline America, we connect individuals with life-changing inpatient rehab for depression programs nationwide. We provide confidential guidance to make the process of seeking help clearer and more manageable.
In patient rehab for depression terms you need:
Understanding Inpatient Rehab for Depression
When depression makes daily life feel impossible, inpatient rehab for depression offers a lifeline. In this intensive residential program, you live full-time at a specialized facility, receiving round-the-clock care. By removing you from daily triggers and responsibilities, it provides a structured, safe space focused entirely on healing.
This immersive approach means medical supervision is available 24/7, so a crisis at 2 a.m. is met with immediate help. Psychiatrists can adjust medications in real-time, rather than waiting weeks for an appointment. The facility handles the structure, allowing you to focus completely on getting better.
Untreated depression has devastating effects on relationships, work, and physical health. The consequences of untreated depression can include chronic pain, a weakened immune system, and increased risk of other serious medical conditions, highlighting the importance of proper treatment.
Who is inpatient rehab for depression best suited for?
This intensive level of care is designed for individuals facing severe, debilitating symptoms. The most urgent indicator is safety. Anyone experiencing suicidal thoughts, planning self-harm, or who has already made an attempt needs the protective environment of inpatient care. If you’re in crisis, call or text 988 to reach the Suicide & Crisis Lifeline 24/7.
Other key signs that inpatient care is necessary include:
- Inability to function: Being unable to get out of bed, maintain personal hygiene, or go to work or school.
- Failed outpatient treatment: When weekly therapy and medication have not improved severe symptoms.
- Co-occurring disorders: Struggling with substance use, anxiety, or PTSD alongside depression requires integrated treatment.
- Need for diagnostic clarity: A 24/7 setting allows a team of specialists to conduct a comprehensive evaluation for complex symptoms.
- Unsupportive home environment: A toxic or triggering home life can prevent recovery, making a therapeutic refuge necessary.
If you or a loved one experiences overwhelming hopelessness, persistent thoughts of death, or a complete withdrawal from daily life, it’s time to consider a higher level of care.
What are the benefits compared to outpatient treatment?
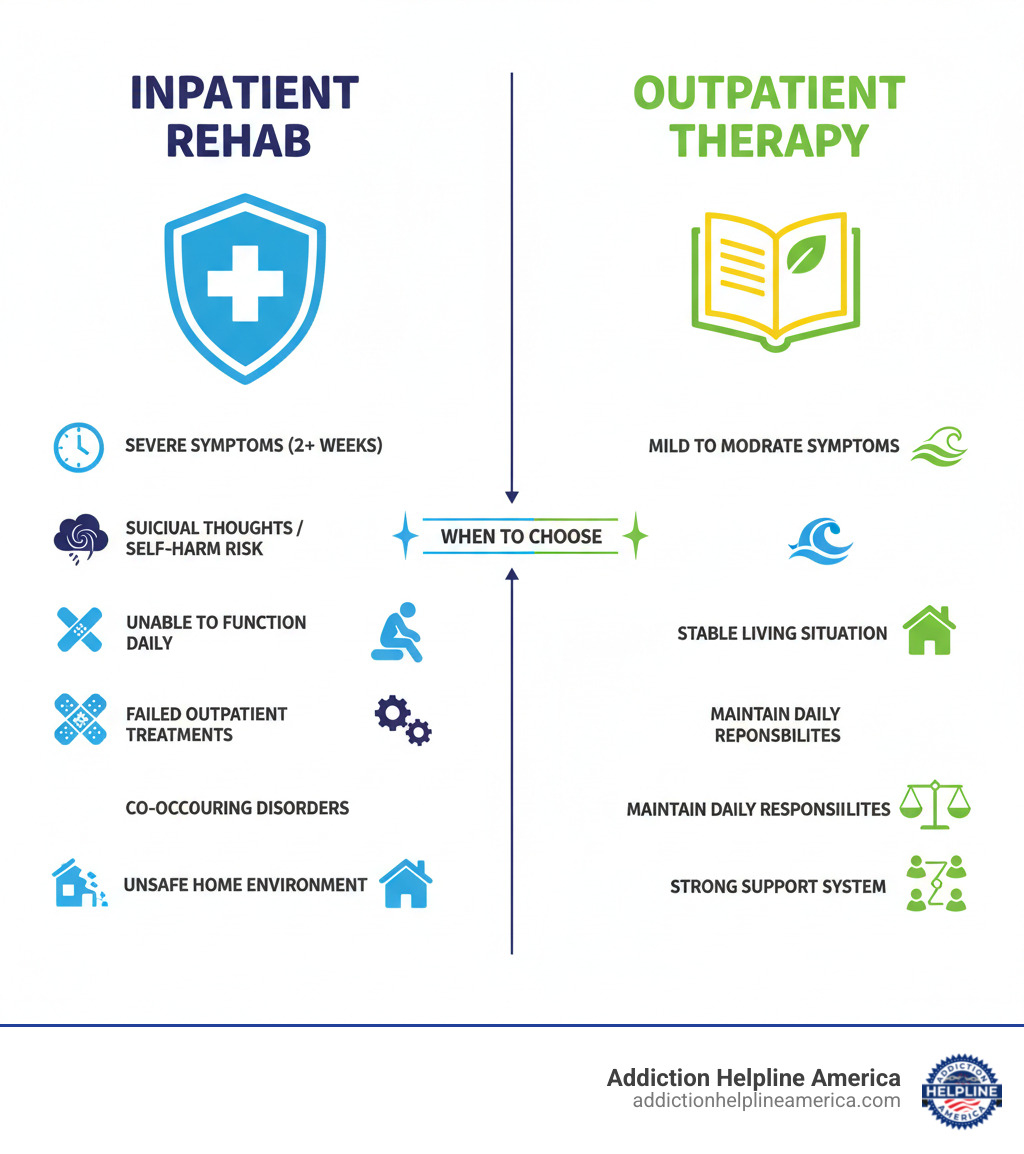
While both inpatient and outpatient care are valuable, inpatient rehab for depression offers unique benefits for those in crisis.
The primary advantage is intensity. Instead of one hour of therapy per week, you engage in multiple therapeutic activities every day. This concentrated approach accelerates healing. Immediate crisis support is another life-saving feature; trained staff are available 24/7 to provide help whenever you need it.
You’ll also find a powerful peer support community of people who understand your struggle, breaking the isolation of depression. Real-time medication management allows psychiatrists to quickly find the right medication and dosage for you, a process that can take months in an outpatient setting.
Perhaps most importantly, inpatient care allows you to focus solely on recovery without distractions. A multidisciplinary team of psychiatrists, therapists, and nurses collaborates on your care, addressing your mental and physical health simultaneously.
Here’s how the two approaches compare:
| Feature | Inpatient Depression Treatment | Outpatient Depression Treatment |
|---|---|---|
| Environment | 24/7 supervised, structured residential facility | Live at home, attend scheduled appointments |
| Intensity | High-intensity, daily therapies and support | Lower intensity, typically weekly or bi-weekly sessions |
| Supervision | Constant medical and therapeutic supervision | Limited supervision, self-management required |
| Crisis Support | Immediate, on-site crisis intervention | Access to emergency services, but not on-site |
| Focus | Holistic healing, stabilization, skill acquisition | Symptom management, skill-building, maintaining daily life |
| Suitability | Severe symptoms, suicidal risk, co-occurring disorders, failed outpatient | Mild to moderate symptoms, stable, functional |
| Distractions | Minimal, controlled environment | Exposure to daily stressors and triggers |
| Cost (Generally) | Higher, but often covered by insurance for medical necessity | Lower per session, but cumulative costs can add up |
Outpatient treatment is effective for mild to moderate depression. But for a crisis, in patient rehab for depression provides the immersive care needed to build a foundation for lasting recovery.
A Look Inside: The Daily Structure and Therapies
One of the most powerful aspects of inpatient rehab for depression is its structure. A predictable daily routine removes the burden of decision-making and creates the stability your brain needs to heal. The schedule is balanced to include therapy, education, physical activity, and rest, creating a rhythm that supports holistic wellness.
What does a typical day look like?
While schedules vary, most programs follow a similar rhythm. A typical day is structured to support healing and is not just sitting in therapy all day.
- Mornings often begin around 7:00 AM and focus on core therapeutic work. After breakfast, you’ll likely participate in group therapy, psychoeducational workshops, and individual therapy sessions.
- Afternoons mix specialized workshops with experiential therapies. This may include sessions on goal setting, physical exercise to boost mood, or other therapeutic modalities.
- Evenings are for connection and processing. After dinner, you might attend a support group meeting or participate in recreational activities before winding down for a restful night’s sleep.
Nutritious meals and free time for personal reflection are integrated throughout the day. This structure is designed to heal your mind, body, and spirit.
What types of therapies and treatments are offered in inpatient depression rehab?
Inpatient rehab for depression uses a toolkit of evidence-based therapies custom to your needs. This multifaceted approach addresses the whole person, not just the symptoms.
- Cognitive Behavioral Therapy (CBT) is a cornerstone, helping you identify and change the negative thought patterns and behaviors that fuel depression.
- Dialectical Behavior Therapy (DBT) is powerful for managing overwhelming emotions. It teaches skills in mindfulness, distress tolerance, emotional regulation, and interpersonal effectiveness.
- Individual psychotherapy offers a confidential, one-on-one space to explore personal issues and develop coping strategies.
- Group therapy provides a profound sense of connection, allowing you to share experiences with others who truly understand your struggle.
- Family therapy can help improve communication and build a stronger support system for your long-term recovery.
Many programs also integrate holistic approaches. Experts agree that lifestyle changes for depression are crucial. This includes mindfulness and meditation, yoga and physical activity, art and music therapy, and nutritional counseling to support your overall well-being.
To help you prepare, we’ve created a guide on What to Pack for Rehab to ensure you’re comfortable on your healing journey.
How long does inpatient rehab for depression typically last?
The duration of your stay in inpatient rehab for depression is individualized based on your needs, the severity of your symptoms, and your progress. There is no one-size-fits-all timeline.
- Short-term stabilization programs may last a few days and are designed for acute crises to ensure safety.
- Most comprehensive inpatient rehab programs last 30 to 90 days. This allows for thorough assessment, intensive treatment, and skill development.
- Some residential programs may extend beyond 90 days for complex or chronic cases.
Factors like the severity of symptoms and the presence of co-occurring conditions (like substance use or trauma) will influence the recommended length of stay. The goal is to ensure you are stable and equipped for a successful transition to a lower level of care, not to rush you through a program.
Essential Components of a Comprehensive Program
The best inpatient rehab for depression programs use an integrated care model that treats you as a whole person. They address the connections between your mental health, physical health, and daily habits to build a solid foundation for lasting wellness. A comprehensive program also prepares you for life after treatment, giving you the tools and support needed to maintain progress long-term.
What is the role of medication in treatment?
Medication is often a key component of treatment. After a thorough psychiatric evaluation, you may be prescribed antidepressants. The most common types are Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), which help restore the balance of mood-regulating chemicals in the brain.
The inpatient setting is ideal for real-time medication management. Your psychiatrist can monitor your response closely and make adjustments quickly, accelerating the process of finding what works best for you. For those with treatment-resistant depression, inpatient programs can offer advanced options like Electroconvulsive Therapy (ECT) or Transcranial Magnetic Stimulation (TMS).
As this depression medications overview explains, antidepressants are most effective when combined with therapy and lifestyle changes.
How are co-occurring disorders addressed?
Depression rarely exists in a vacuum. Many people entering inpatient rehab for depression also struggle with anxiety, substance use, trauma, or eating disorders. This is known as a dual diagnosis and requires specialized, integrated treatment.
A quality program treats all conditions simultaneously. Your therapy will address how these conditions interact and reinforce one another. For example, if you struggle with depression and addiction, the program will provide a safe medical detox (if needed) followed by therapy that explores the roots of both issues. Therapies like CBT and DBT are effective for both depression and anxiety disorders.
For those with trauma and PTSD, trauma-informed care creates a safe environment to process past experiences without being retraumatized. This comprehensive approach is essential for a complete and lasting recovery.
Our network includes specialized Depression Treatment Centers that excel in treating co-occurring disorders. We can help you find a program equipped to address your specific challenges.
What happens after completing a program (aftercare)?
Completing an inpatient rehab for depression program is a major achievement, but it’s the beginning of your long-term recovery journey, not the finish line. A solid aftercare plan is crucial to prevent relapse and maintain your progress.
Discharge planning begins well before you leave. Your team will create a personalized plan that may include:
- Relapse prevention strategies: Learning to recognize your personal warning signs and having a crisis plan in place.
- Step-down programs: A gradual transition through a Partial Hospitalization Program (PHP) or an Intensive Outpatient Program (IOP), which offer structured therapy while you live at home.
- Sober living homes: For those with co-occurring substance use disorders, these provide a supportive, drug-free environment.
- Ongoing therapy: Regular sessions with a therapist to maintain momentum and steer new challenges.
- Support groups: Connecting with peers through organizations like the Depression and Bipolar Support Alliance or NAMI. The Mental Health Toolkit is a great resource for finding groups.
This continuum of care gives you the best chance at lasting recovery. At Addiction Helpline America, we guide you through the entire journey, from inpatient care to aftercare. You can explore various types of treatment programs to understand what’s right for you.
Frequently Asked Questions about Inpatient Depression Treatment
Choosing inpatient rehab for depression is a major decision, and it’s normal to have questions. We’re here to provide the answers you need to move forward with confidence.
What is the success rate of inpatient rehab for depression?
While there’s no single “success rate” because recovery is personal, inpatient rehab for depression is highly effective for severe cases. Scientific research on inpatient program effectiveness shows that intensive programs lead to significant symptom reduction and improved daily functioning. A relapse doesn’t mean treatment failed; it means more support is needed. The skills you gain in rehab provide a strong foundation for lifelong resilience.
How much does inpatient rehab for depression cost?
The cost of inpatient rehab for depression varies by facility, location, and program length. While it can seem daunting, there are several ways to make it affordable.
The good news is that insurance often covers inpatient mental health treatment when it’s deemed medically necessary. Most private plans, as well as Medicare and Medicaid, provide substantial coverage. If you don’t have insurance, many facilities offer private pay rates, financing plans, or payment arrangements.
Navigating insurance can be confusing. At Addiction Helpline America, we can help you verify your benefits and understand your coverage, connecting you with facilities that accept your insurance to remove financial barriers.
How do I find the right inpatient facility?
Finding the right inpatient rehab for depression is crucial, and you don’t have to do it alone. Here are key factors to look for:
- Accreditation: Look for accreditation from The Joint Commission or CARF, which indicates high standards for quality and safety.
- Licensed Staff: The team should include experienced psychiatrists, licensed therapists, and registered nurses with expertise in depression.
- Evidence-Based Therapies: The facility must use proven methods like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT).
- Individualized Treatment: Avoid cookie-cutter approaches. A quality facility will create a personalized plan based on your unique needs and goals.
- Aftercare Planning: The program should have a strong focus on discharge planning and connecting you with step-down programs and ongoing support.
Reading Treatment Center Reviews can also provide valuable insights from former patients.
At Addiction Helpline America, we provide free, confidential guidance to help you find the right program from our network of trusted centers. We serve individuals and families in Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, Virginia, Washington, West Virginia, Wisconsin, Wyoming, and the District of Columbia. Our only goal is to find the best fit for you.
Conclusion
Taking the first step toward inpatient rehab for depression is a courageous decision. As this guide has shown, it offers the 24/7 medical supervision, intensive therapy, and supportive community needed to break free from the grip of severe depression. You’ve learned that treatment is custom to your needs, combining evidence-based therapies with expert medication management to build a foundation for lasting recovery.
Recovery from depression is not just possible—it’s a reality for people just like you. Depression is a treatable medical condition, and you deserve to feel better. Reaching out for help is a sign of strength, and you don’t have to walk this path alone.
Addiction Helpline America is here to help you find the right fit from our trusted network of treatment centers across all 50 states. Our service is free, confidential, and personalized. We don’t profit from referrals, so our only focus is connecting you with the care you need. Whether you have questions about insurance, treatment options, or just need to talk, we’re here.
Let us help you take that first step. Find the right treatment program for you and begin your journey toward healing today.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.