When someone is struggling with addiction, the idea of "treatment" can sound clinical and intimidating. But at its core, drug abuse treatment is really a structured, supportive process designed to help people break free from compulsive substance use and, piece by piece, rebuild their lives.
This isn't about punishment. It's about healing—a journey that combines medical care with therapeutic guidance to help someone get sober, stay sober, and learn to thrive again.
Navigating Your First Steps to Recovery
Taking that first step toward overcoming addiction is often the hardest part, but breaking down the path ahead can make the whole process feel much more manageable. A good treatment program doesn't just treat the addiction; it demystifies recovery, turning what feels like an impossible mountain into a series of small, achievable steps.
Think of it as being handed a map and a compass after being lost in the woods. Treatment provides the direction, the tools, and an experienced guide to help you find your way back to a healthy and fulfilling life. It’s a supportive environment that proves help is always available and that recovery is absolutely possible.
What Is Treatment Really Trying to Accomplish?
At its heart, drug abuse treatment is built on a few clear, fundamental goals. These objectives become the bedrock of any personalized recovery plan, guiding the process from the very first conversation all the way to long-term sobriety.
The best programs focus on treating the whole person, not just the substance use. That means addressing the physical, psychological, and even the social aspects of addiction to create a strong foundation for healing.
The main aims usually boil down to three things:
- Achieving Sobriety: The immediate goal is to help you safely stop using. For many, this starts with a medically supervised detoxification process to manage withdrawal.
- Preventing Relapse: This is where the real work begins. You learn how to spot your triggers, handle cravings, and build a toolbox of healthy coping skills for long-term success.
- Rebuilding a Healthy Life: Treatment empowers you to mend relationships, take charge of your health, and find stability in your work, home, and community.
The journey begins with the understanding that you are not alone. Millions face this challenge, yet a significant gap in care remains. It is a worldwide issue that requires more accessible solutions.
Understanding the Treatment Gap
The need for effective and accessible drug treatment has never been clearer. The World Drug Report 2025 paints a stark picture: in 2023, an estimated 316 million people around the world used drugs.
Of those, about 64 million were found to have drug use disorders. But here’s the most alarming statistic: only about 8.1% of them actually received treatment. That’s a massive gap in care.
This number shows just how critical it is to have compassionate, easy-to-access treatment programs. By making these first steps less intimidating, we can encourage more people to seek the life-changing help they need and deserve.
Navigating the journey from active addiction to recovery involves several distinct phases. The table below outlines the typical stages you can expect in a structured treatment program.
Key Stages of the Drug Treatment Journey
| Stage | Primary Goal | Common Activities |
|---|---|---|
| 1. Initial Contact & Assessment | To understand the individual's needs and determine the right level of care. | Phone call or meeting with an admissions counselor, clinical evaluation, and medical screening. |
| 2. Detoxification (Detox) | To safely manage withdrawal symptoms as substances leave the body. | Medically supervised withdrawal, symptom management, and emotional support. |
| 3. Rehabilitation (Rehab) | To address the root causes of addiction and build coping skills. | Individual therapy (like CBT), group counseling, family therapy, and educational workshops. |
| 4. Aftercare & Ongoing Support | To maintain sobriety and prevent relapse after formal treatment ends. | Support groups (like AA/NA), sober living arrangements, ongoing therapy, and alumni programs. |
Each stage builds on the last, creating a comprehensive support system that guides you from crisis to a sustainable, sober life.
Choosing the Right Treatment Program for You
Once you’ve made the courageous decision to get help, the next step is figuring out which kind of abuse drug treatment program is the right fit. This isn't a one-size-fits-all situation. The best path for you hinges on your personal circumstances, how severe the addiction is, and what your daily responsibilities look like.
Think of it like this: are you looking for a completely immersive experience, or do you need something that works around your existing life? The two main avenues, inpatient and outpatient care, cater to these very different needs.
Comparing Inpatient vs Outpatient Treatment Programs
To make the best choice, it helps to see the core differences side-by-side. Both inpatient and outpatient programs have the same goal—lasting recovery—but they take very different routes to get there.
| Feature | Inpatient (Residential) Treatment | Outpatient Treatment |
|---|---|---|
| Living Situation | You live at the facility 24/7 for the duration of the program. | You live at home and travel to the facility for scheduled sessions. |
| Environment | A highly structured, immersive, and trigger-free setting. | You remain in your regular environment, facing real-world triggers. |
| Intensity & Structure | Very high. Your entire day is scheduled with therapy and activities. | More flexible. Sessions are scheduled for a few hours, a few times a week. |
| Level of Support | 24/7 access to medical and clinical staff. | Support is available during program hours. After-hours support is typically via a crisis line. |
| Best For | Severe addictions, co-occurring mental health disorders, or unstable home environments. | Milder addictions, strong support systems at home, or as a step-down from inpatient care. |
| Daily Life | All work, school, and family obligations are put on hold. | You can often continue working, attending school, and managing family life. |
Ultimately, the choice comes down to what level of structure and support you need to feel safe and focused as you begin your recovery journey.
Inpatient Residential Treatment: A Deep Dive
Inpatient treatment, also known as residential treatment, is the most intensive level of care available. It means you live at the facility around the clock, typically for 30, 60, or 90 days. This approach is often the best choice for people with severe substance use disorders or for those who have tried to quit before and relapsed.
The biggest advantage is being completely removed from your usual environment. You get a clean break from the people, places, and daily stressors that might trigger drug use. This allows you to focus 100% on getting better.
Days are tightly structured, filled with a blend of individual therapy, group sessions, medical check-ins, and classes that teach you about the nature of addiction. You’re surrounded by a built-in support system of professionals and peers who know exactly what you’re going through. It’s a powerful thing to know you’re not alone.
The core idea behind inpatient care is to create a safe, controlled sanctuary where healing is the only priority. It provides the space needed to break the physical and psychological cycles of addiction before re-engaging with the outside world.
The Flexibility of Outpatient Treatment
Outpatient treatment offers a completely different kind of structure—one built on flexibility. It’s a great option for people with less severe addictions or for those who have a strong, supportive network at home. Many people also transition to an outpatient program after completing an inpatient stay.
Instead of living at a center, you attend therapy sessions several times a week while continuing to live at home. This allows you to immediately apply the coping skills you’re learning to real-world situations. You can keep your job, take care of your family, and stay connected to your community, which can be a huge motivator.
Of course, that flexibility means you’ll also have to navigate daily triggers on your own. Success in an outpatient program requires a high degree of personal commitment and a stable living situation that supports your recovery goals.
Finding the Right Level of Care
The good news is that treatment isn't just a choice between these two extremes. There are programs that bridge the gap, offering a blend of structure and independence.
- Partial Hospitalization Programs (PHP): This is the most intensive type of outpatient care. You’ll attend treatment for several hours a day, five to seven days a week, giving you a level of support that’s very close to an inpatient program while letting you sleep in your own bed at night.
- Intensive Outpatient Programs (IOP): IOPs are a slight step down from PHPs. Sessions are usually held three to five days a week for about three hours at a time. This model provides solid, consistent support but offers more room to accommodate a work or school schedule.
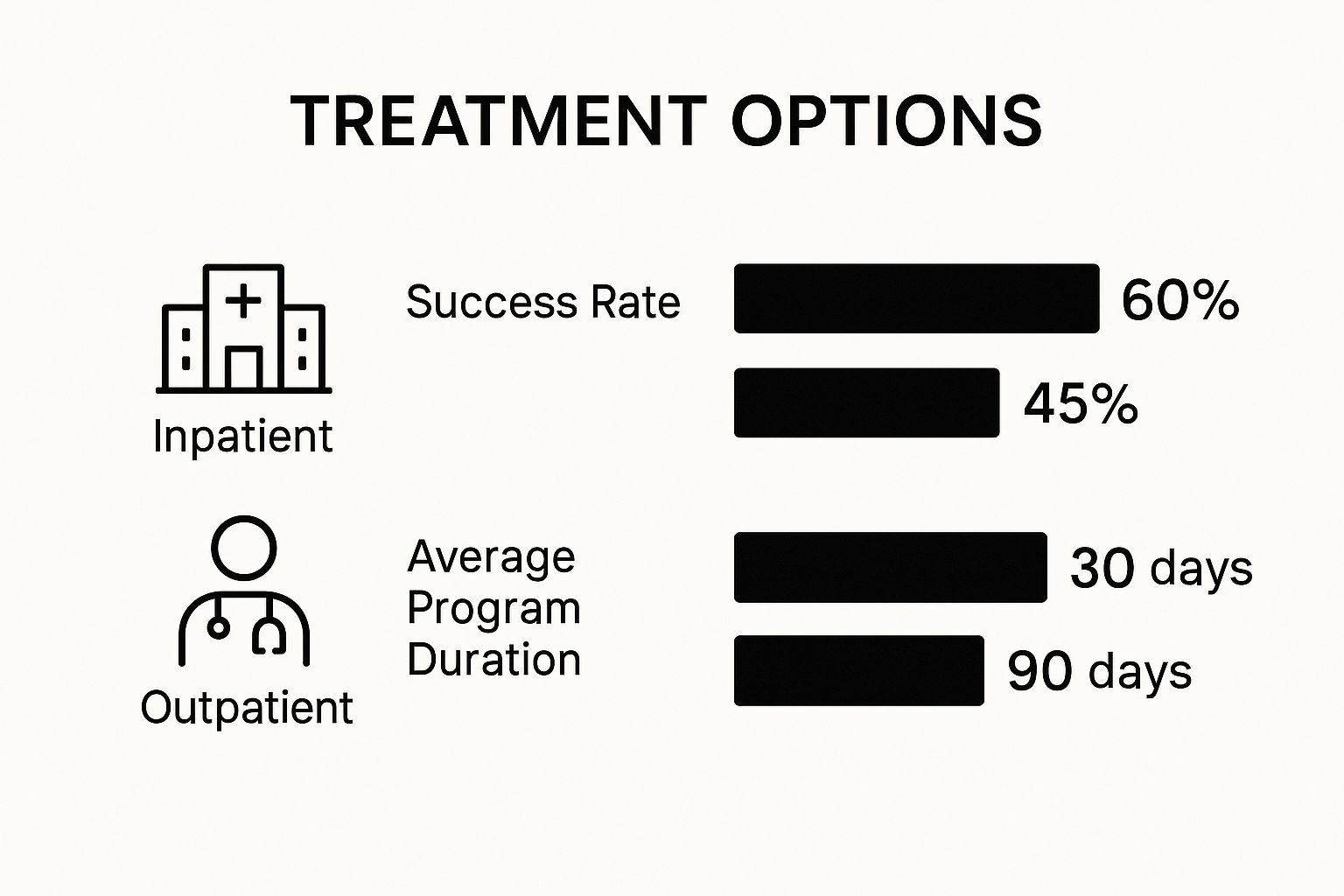
The image below gives a snapshot of how these two main approaches compare in terms of success rates and typical program lengths.
While inpatient programs often boast higher success rates right out of the gate due to their focused nature, outpatient care provides a crucial, longer-term support structure. The key is to weigh these factors honestly against your own needs to find the best fit for your recovery journey.
Exploring Core Therapies in Addiction Recovery
At the heart of any solid addiction treatment program, you'll find a collection of proven, evidence-based therapies. These aren't just chats; they're structured, powerful tools designed to help you get to the bottom of your addiction and build the skills you need for a life of sobriety.
Think of it like a workshop for your mind. You learn to dismantle old, destructive patterns and construct new, healthier ways of thinking and reacting. These therapies are all about tackling the psychological side of addiction—untangling the thoughts and feelings that have been fueling substance use for so long. It's how you regain control and learn to handle life's curveballs without turning back to old habits.
Cognitive Behavioral Therapy: The Blueprint for Change
One of the most trusted and effective methods in addiction treatment is Cognitive Behavioral Therapy (CBT). The idea behind CBT is brilliantly simple yet incredibly powerful: our thoughts, feelings, and behaviors are all linked. If you can change your negative thinking, you can change your actions.
Imagine your brain has these well-worn paths that lead straight to using whenever you feel stressed or down. CBT helps you spot those trails and then consciously blaze new, healthier ones. You learn to press pause, identify the trigger, and deliberately choose a different route.
For example, a therapist helps you catch that automatic thought, "I can't get through this without a drink." CBT then gives you the tools to challenge it and replace it with something more constructive, like, "This is tough, but I have other ways to cope. I can call my sponsor or just get outside for a walk." It’s a very practical, hands-on way to rewire your brain’s automatic responses.
Dialectical Behavior Therapy: Mastering Your Emotions
Where CBT hones in on your thoughts, Dialectical Behavior Therapy (DBT) specializes in helping you manage intense, overwhelming emotions. DBT is a lifesaver for people whose powerful feelings often lead to impulsive actions, including drug or alcohol use.
DBT is built on teaching four key skill sets:
- Mindfulness: Learning how to stay grounded in the present moment without judging yourself.
- Distress Tolerance: Building skills to survive a crisis without making things worse.
- Emotion Regulation: Understanding your emotional triggers and learning how to be less vulnerable to them.
- Interpersonal Effectiveness: Figuring out how to ask for what you need and build better relationships.
This skill-based approach gives you a real-world toolkit for navigating emotional storms, which in turn quiets the urge to use substances as an escape.
By getting to the root of the mental and emotional health challenges driving the behavior, evidence-based therapies like CBT and DBT build a strong foundation for a recovery that can actually last. They go after the cause, not just the symptom.
The need for this kind of help is massive. Substance use disorders are serious mental health conditions affecting millions. In fact, an estimated 48.5 million people in the United States aged 12 or older had a substance use disorder in the past year alone. This number really underscores the urgent need for treatment that works. You can learn more about the scope of SUDs on TherapyRoute.com.
The Power of Connection: Group and Family Therapy
Recovery is almost never a solo mission. That's precisely why group and family therapies are such vital parts of any comprehensive treatment plan.
Group therapy offers a safe environment where you can connect with people who just get it. There's an incredible power in sharing your story with others who have walked a similar path, as it helps break down the shame and isolation that addiction thrives on. In a group, you get to practice new communication skills, get honest feedback, and build a support system that often lasts long after the program ends.
Family counseling, on the other hand, focuses on healing the relationships strained by addiction. It’s a space for educating loved ones about the disease of addiction, improving how everyone communicates, and setting healthy boundaries for the future. When you involve family in the healing process, you help create a supportive home environment—a critical piece for long-term success. Together, these therapies drive home one essential truth: you are not alone in this fight.
Understanding Medication-Assisted Treatment
https://www.youtube.com/embed/MslfDFVf1NE
Medication-Assisted Treatment (MAT) is a cornerstone of modern addiction care, backed by solid science, especially for those fighting alcohol and opioid use disorders. There's a persistent myth that MAT is just swapping one drug for another. That couldn't be more wrong.
Let's think about it like this: no one considers insulin a "crutch" for a person with diabetes. It's a medical necessity that corrects a physical imbalance. MAT works the same way, using specific, FDA-approved medications to re-stabilize the brain chemistry that addiction has thrown out of whack.
This medical support is a key piece of a comprehensive abuse drug treatment plan. It helps by dialing down the intense cravings and blocking the rewarding effects of drugs or alcohol. This gives a person the breathing room and mental clarity they need to really dig in and do the hard work in therapy. It's about building a stable foundation for recovery.
How Do These Medications Actually Work?
MAT medications are always prescribed and managed by a doctor to ensure they're safe and working as they should. They're designed to help the recovery process, not to create a new high. The right medication is chosen based on the substance a person was using and their overall health.
The main goals are simple: get the brain back to a normal state and quiet the overwhelming physical cravings that so often trigger a relapse.
Here are a few of the most common medications used in MAT:
- Buprenorphine (Suboxone): A go-to for opioid addiction, buprenorphine binds to the same receptors as other opioids but with a much weaker effect. This satisfies the brain's craving and stops withdrawal symptoms without producing a high.
- Naltrexone (Vivitrol): This one works for both opioid and alcohol use disorders, but in a totally different way. It acts like a shield, completely blocking the euphoric feelings from these substances. If someone uses while on Naltrexone, they won't feel the desired effect, which helps break the mental connection between the substance and the reward.
- Methadone: Methadone has been a gold standard in treating opioid addiction for decades. When taken as prescribed in a clinical setting, it effectively reduces cravings and withdrawal, allowing people to regain stability in their lives.
Medication-Assisted Treatment isn't a silver bullet; it's an integrated strategy. When you combine it with counseling and therapy, MAT is proven to improve patient survival, keep people in treatment longer, and significantly cut down on illicit drug use.
Who Is a Good Candidate for MAT?
Figuring out if MAT is the right call is a conversation between you and your doctor. It's an incredibly powerful tool, but it has to be part of a bigger plan that includes therapy, support groups, and other behavioral changes.
It all starts with a complete medical and psychological evaluation. For a deeper dive into how it all works, you can explore what is medication assisted treatment in our detailed guide.
This approach is often a game-changer for people who:
- Are battling an opioid or alcohol addiction.
- Have tried quitting on their own or with other methods but relapsed.
- Are facing severe withdrawal symptoms or overpowering cravings.
- Are ready and willing to participate in therapy alongside taking medication.
By tackling the physical side of addiction head-on, MAT gives you a real chance to focus on the psychological and behavioral work required for a lasting recovery. It helps level the playing field, making sobriety feel less like an impossible climb and more like an achievable goal.
How to Manage Detox and Withdrawal Safely
Detox is where the physical journey of recovery truly begins. It’s the process of letting your body clear itself of a substance, essentially hitting a reset button to create a clean slate. Once the physical fog starts to lift, the real, deeper work of psychological healing can finally get underway.
But that reset process isn't always simple. When your body becomes physically dependent on a substance, its entire chemistry adapts to function with that substance in the mix. If you suddenly stop—what most people call quitting "cold turkey"—it's like pulling the rug out from under your system. That abrupt shift is what triggers withdrawal, a storm of physical and mental symptoms that can be anything from uncomfortable to downright dangerous.
The Dangers of Quitting Cold Turkey
Trying to detox on your own at home is a gamble you don't want to take. The intensity of withdrawal symptoms varies wildly depending on the drug, how long you've been using it, and your overall health. For substances like alcohol, benzodiazepines, and opioids, going it alone can lead to life-threatening complications.
Here are just a few of the risks you could face:
- Severe Dehydration: Constant vomiting and diarrhea can quickly drain your body of essential fluids.
- Seizures: This is a very real and life-threatening risk, especially when withdrawing from alcohol or benzodiazepines.
- Cardiac Complications: The immense stress on your system can trigger heart palpitations, dangerously high blood pressure, and even heart failure.
- Psychosis: Some withdrawals can cause hallucinations, severe paranoia, and delirium, putting both you and those around you at risk.
Medically supervised detox isn't about just being more comfortable—it's about staying alive. It puts you in a controlled, professional setting where medical experts can manage symptoms and handle any emergency immediately, making the whole process as safe as it can possibly be.
What Happens During a Medical Detox
A professional medical detox program is a carefully structured process designed to get you through withdrawal safely and set you up for the next phase of your treatment. Think of it as a bridge from physical dependency to a stable, clear-headed state.
The process usually unfolds in three key stages. For a deeper dive, you can explore our complete guide to the stages of detox.
1. Comprehensive Evaluation
As soon as you arrive, a clinical team will sit down with you for a thorough assessment. This isn’t just a quick chat; it involves a physical exam, blood tests, and a screening for any co-occurring mental health issues like anxiety or depression. All this information is used to build a detox plan that’s customized just for you.
2. Stabilization and Symptom Management
This is the core of the detox process. Medical staff will monitor your vital signs around the clock to keep you stable and as comfortable as possible. They can provide medications to ease the worst of the withdrawal symptoms, helping to curb cravings, prevent seizures, or manage nausea and anxiety.
3. Preparation for Continued Treatment
It’s critical to understand that detox is just the first step—it isn’t a cure for addiction. The ultimate goal of a detox program is to get you physically and mentally prepared for a full rehabilitation program. Before you leave, the staff will help you figure out what comes next, connecting you with the therapy and support you need to tackle the root causes of addiction and build a real foundation for sobriety.
Planning for a Life of Sobriety After Treatment
Finishing a drug treatment program is a massive accomplishment, and you should be incredibly proud. It's a huge step. But here’s the thing—the real work begins the moment you walk out those doors. Recovery isn’t a one-and-done event; it's a lifelong journey, and having a solid aftercare plan is the next critical piece of the puzzle.
Think of it like this: rehab is where you learn to fly, but your aftercare plan is your flight navigation system for the rest of your life. A good program won't just send you on your way; they'll help you build this "recovery roadmap" before you leave, so you're ready for whatever life throws at you.
Building Your Recovery Roadmap
A strong aftercare plan isn't some generic checklist. It’s your personalized strategy for staying sober, designed to help you handle the ups and downs of everyday life without falling back into old patterns. This plan is your first and best line of defense against relapse.
The most effective roadmaps are built on a few core elements that give you structure, support, and accountability. They work together like a safety net, making sure you always have somewhere to turn when things get tough.
Key parts of a strong aftercare strategy include:
- Ongoing Therapy: Continuing with a counselor, either one-on-one or in a group, helps you keep digging into the root causes of addiction and sharpen your new coping skills.
- Support Groups: Programs like Narcotics Anonymous (NA) or Alcoholics Anonymous (AA) are invaluable. They connect you with a community of people who just get it.
- A Reliable Support System: This means actively leaning on sober friends and family members who are genuinely invested in your recovery.
Identifying Triggers and Mastering Coping Skills
A huge part of staying sober is getting really honest about your personal triggers. What people, places, feelings, or situations make you want to use? An aftercare plan forces you to pinpoint these landmines so you can develop healthy ways to navigate around them.
Instead of automatically reaching for a substance when stress hits, you'll have a new toolbox of coping skills. Maybe you’ll go for a run, practice a quick mindfulness exercise, call your sponsor, or just get your thoughts down in a journal. It’s all about replacing those old, destructive habits with conscious, positive actions.
An aftercare plan is your personal blueprint for navigating sobriety. It anticipates challenges and provides a clear, actionable path forward, empowering you to protect the progress you've worked so hard to achieve.
Creating this plan turns recovery from a vague hope into a concrete, daily practice. It’s a commitment to self-awareness and intentional living.
This focus on long-term support is gaining traction worldwide. The European Drug Report 2025, for instance, highlights a major push to expand evidence-based treatments and harm reduction services across the continent. This signals a growing recognition that effective abuse drug treatment has to include robust, ongoing support. You can read more about European drug treatment trends on euda.europa.eu.
Creating a Supportive Environment
Your surroundings play a massive role in your long-term success. A key part of your aftercare plan is to deliberately build a life that supports your sobriety, which often means making some difficult but necessary changes.
This could mean finding new, sober hobbies to fill the time once spent on activities centered around using. It might involve setting firm boundaries with friends or even family who don't respect your new path. For some, sober living homes provide an excellent transitional step, offering a structured environment with built-in accountability and peer support. Our guide on how to quit drinking has some great strategies for creating a supportive, alcohol-free lifestyle.
By taking these intentional steps, you’re creating a world for yourself where making the healthy choice becomes the easy choice. You're laying the foundation for a future defined not by addiction, but by freedom and purpose.
Answering Your Questions About Drug Rehab
It’s completely normal to have a lot of questions when you’re looking into addiction recovery. The whole process can seem confusing and overwhelming. Getting some clear, honest answers can make all the difference, helping you feel more prepared whether you’re seeking help for yourself or for someone you love.
Let's walk through some of the most common questions we hear. Our goal is to clear up the confusion so that taking the next step feels a little bit easier.
How Long Does Drug Rehab Last?
This is one of the first questions people ask, but there's no one-size-fits-all answer. The length of treatment really depends on the individual's specific needs. Think of it like physical therapy after an injury—some people need a few weeks, while others might need months to fully heal.
Inpatient or residential programs often run for 30, 60, or 90 days. These structured environments are great for getting stable and focusing completely on recovery. For more severe or long-standing addiction, a longer stay might be recommended.
Outpatient programs, on the other hand, are more flexible and can last for several months or even a year. The evidence is pretty clear on this: the longer a person stays engaged in treatment, the better their chances are for long-term success. It simply takes time to unlearn old behaviors and build new, healthy habits.
Will My Health Insurance Cover Treatment?
For most people, the answer is yes. Thanks to laws like the Affordable Care Act (ACA), most major insurance plans are required to cover treatment for substance use disorders just like they would for any other medical condition.
However, the amount of coverage varies wildly from plan to plan. Your out-of-pocket costs, like deductibles and copays, will depend on the specifics of your policy. The best first step is to verify your benefits. You can call your insurance company directly, or let the admissions team at a treatment center handle it for you—they do this every day and can quickly figure out what's covered.
It's important to know the difference between addiction and dependence. Physical dependence means your body has adapted to a substance and needs it to avoid withdrawal. Addiction is a disease of the brain, characterized by compulsive drug-seeking and use, despite knowing the devastating consequences. It's a much deeper psychological and behavioral issue.
Can Someone Be Forced into Treatment?
This is a tough one, both legally and emotionally. In some cases, yes, a person can be legally required to go to rehab. Many states have laws (often called civil commitment or involuntary commitment laws) that allow a court to order treatment if a person's substance use makes them a danger to themselves or others.
The criminal justice system can also mandate treatment as part of a sentence or as an alternative to jail time. While this can be a life-saving intervention, motivation is a huge factor in recovery. Someone who chooses to be there is often more open to change. If you're struggling to convince a loved one, learning how to approach the conversation is key. You can find some guidance in our article on providing recovery support for a drug addict.
The path to recovery can feel uncertain, but you don't have to navigate it by yourself. If you or someone you care about needs help, the team at Addiction Helpline America is available 24/7 to offer free, confidential support. Call us anytime to talk with a specialist who can listen, explain your options, and help you find the way forward.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.