
Navigating addiction treatment success rates often feels like trying to hit a moving target. That’s because success isn’t just one magic number. It’s a blend of different outcomes, from sustained sobriety and program completion to a genuinely improved quality of life. Understanding the context behind the statistics is everything.
What Do Treatment Success Rates Actually Mean?
When you start researching treatment facilities, you’ll be hit with all sorts of statistics. But on their own, these numbers rarely paint the full picture. The very definition of “success” can shift dramatically from one center to the next, which is why you have to look deeper to make a smart choice.
A high success rate sounds great, but what is it actually measuring? Is it based on someone finishing a 30-day program, or does it track their sobriety a full year after they’ve left? Getting answers to these questions is the only way to accurately interpret the figures you see.
Core Metrics for Defining Success
True success in recovery is a big-picture concept, going far beyond just staying away from substances. From my experience, the best treatment programs track a whole range of outcomes to get a holistic view of how well they’re really doing.
Some of the most common metrics include:
- Sobriety Duration: This tracks how long a person remains sober after completing treatment.
- Program Completion: This is the percentage of clients who see their recommended treatment plan through to the end.
- Quality of Life Improvements: This measures positive changes in key areas like employment, family relationships, and overall well-being.
- Reduced Legal Issues: A simple but powerful metric is a drop in arrests or other legal troubles after treatment.
“The most meaningful addiction treatment success rates are those that reflect long-term, positive life changes, not just short-term abstinence. They show that an individual has developed the skills to manage their recovery journey effectively.”
What the Data Reveals
Even with varying definitions, the data consistently points to one thing: completing a structured treatment program gives you a much better shot at long-term recovery. For example, some studies show that between 85% and 95% of people who finish a rehab program are still drug-free nine months later. On top of that, about 80% of patients report that their quality of life got better after treatment. You can learn more about these rehabilitation statistics and what they mean for the recovery journey.
To make sense of all this, it helps to have a clear breakdown of how success is measured.
Key Metrics for Measuring Treatment Success
The table below summarizes the most common metrics used to gauge the effectiveness of addiction treatment. Think of it as a quick reference guide to help you understand what the numbers really mean when you see them.
| Success Metric | What It Measures | Common Benchmark |
|---|---|---|
| Abstinence Rate | The percentage of alumni who are sober at a specific time (e.g., 90 days, 1 year). | Varies widely; often 30-60% at one year. |
| Program Completion | The ratio of clients who finish the entire program versus those who leave early. | Higher rates suggest better client engagement. |
| Quality of Life | Improvements in health, relationships, employment, and housing post-treatment. | Often measured via patient surveys and follow-ups. |
Ultimately, these metrics give you the tools to look past flashy marketing claims and focus on what truly matters: finding a program that facilitates lasting, positive change.
The Growing Need for Effective Addiction Treatment
Before we can even talk about individual success, we need to grasp the sheer scale of the challenge we’re facing. The demand for quality addiction treatment is surging, not just in isolated pockets but across entire communities, driven by powerful social and economic tides. This reality makes it absolutely essential to have a full toolbox of proven therapies at our disposal.
A huge part of this urgency comes from the ongoing opioid crisis, especially with the devastating rise of synthetic opioids like fentanyl. The fallout from this crisis has placed an incredible strain on our healthcare systems, families, and local economies, creating a desperate need for treatment that actually works and is easy to access.
The Treatment Market is Expanding to Keep Up
This isn’t just an anecdotal observation; you can see it in the numbers. The global market for addiction services is growing at a remarkable pace, with serious investment aimed at developing better therapies and breaking down barriers to care.
“This isn’t just about putting up more buildings. It’s about a fundamental shift in how we think about recovery. The real focus now is on evidence-backed solutions that can be adapted to a person’s unique situation, because that’s what it takes to fight addiction today.”
The numbers tell a clear story. The global drug addiction treatment market was valued at around USD 18.91 billion and is expected to climb to USD 31.20 billion by 2032. That’s a compound annual growth rate (CAGR) of 7.4%, which shows a sustained, worldwide commitment to tackling substance use. If you’re interested, you can learn more about these market projections and the factors behind them.
A Laser Focus on What Actually Works
Given the gravity of this public health issue, the old “one-size-fits-all” model just doesn’t cut it anymore. The entire field is moving toward therapeutic approaches that have been tested and proven to deliver real, measurable outcomes.
Some of the most important of these include:
- Medication-Assisted Treatment (MAT): This has become a cornerstone for treating opioid use disorder. It’s highly effective at managing cravings and easing the physical agony of withdrawal, giving people a stable foundation for recovery.
- Behavioral Therapies: Techniques like Cognitive Behavioral Therapy (CBT) are critical. They don’t just talk about the problem; they give people practical, real-world skills to manage triggers and stop a relapse before it starts.
- Integrated Care: We’ve finally learned that you can’t treat addiction in a vacuum. Addressing co-occurring mental health conditions like depression or anxiety at the same time is absolutely vital for someone’s long-term well-being.
When you understand the immense scope of this problem, it becomes crystal clear why solid, reliable addiction treatment success rates matter so much. They’re not just numbers on a page; they are the compass that points individuals, families, and providers toward the most promising paths to a lasting recovery.
Comparing Inpatient and Outpatient Program Success
One of the biggest decisions you’ll make on the road to recovery is choosing between an inpatient or outpatient program. There’s no single “better” option; the right choice comes down to your personal situation. The success of any treatment is deeply tied to how well the program fits your specific needs.
Inpatient programs, often called residential treatment, mean you live at the facility. This creates an immersive, structured environment with 24/7 medical and emotional support. By removing you from the daily triggers and stresses that can fuel addiction, these programs provide a critical buffer, especially for those with severe substance use disorders or an unstable home life.
Outpatient programs, on the other hand, offer flexibility. You continue living at home while attending scheduled therapy sessions a few times a week. This allows you to keep up with work, school, or family commitments, making it a great fit for people who have a strong support system and a less severe addiction. It’s all about finding a balance between getting help and managing daily life.
Situational Effectiveness: The Deciding Factor
To make the right choice, you have to be honest with yourself about your circumstances. If you’ve been struggling with addiction for a long time, have co-occurring mental health issues like anxiety or depression, or live in a chaotic environment, an inpatient program often provides the stability needed for a real chance at success. That constant structure is invaluable for minimizing relapse risk in the fragile, early days of recovery.
However, someone with a great family network, a steady job, and a more recent or less severe addiction can do incredibly well in an outpatient setting. This approach lets you practice the coping skills you learn in therapy in real time, which helps solidify your recovery in your own environment. For a deeper dive, check out our guide on inpatient vs. outpatient rehab, which details the specific scenarios where each type of care shines.
This infographic gives a quick visual breakdown of average success rates for different treatment approaches.
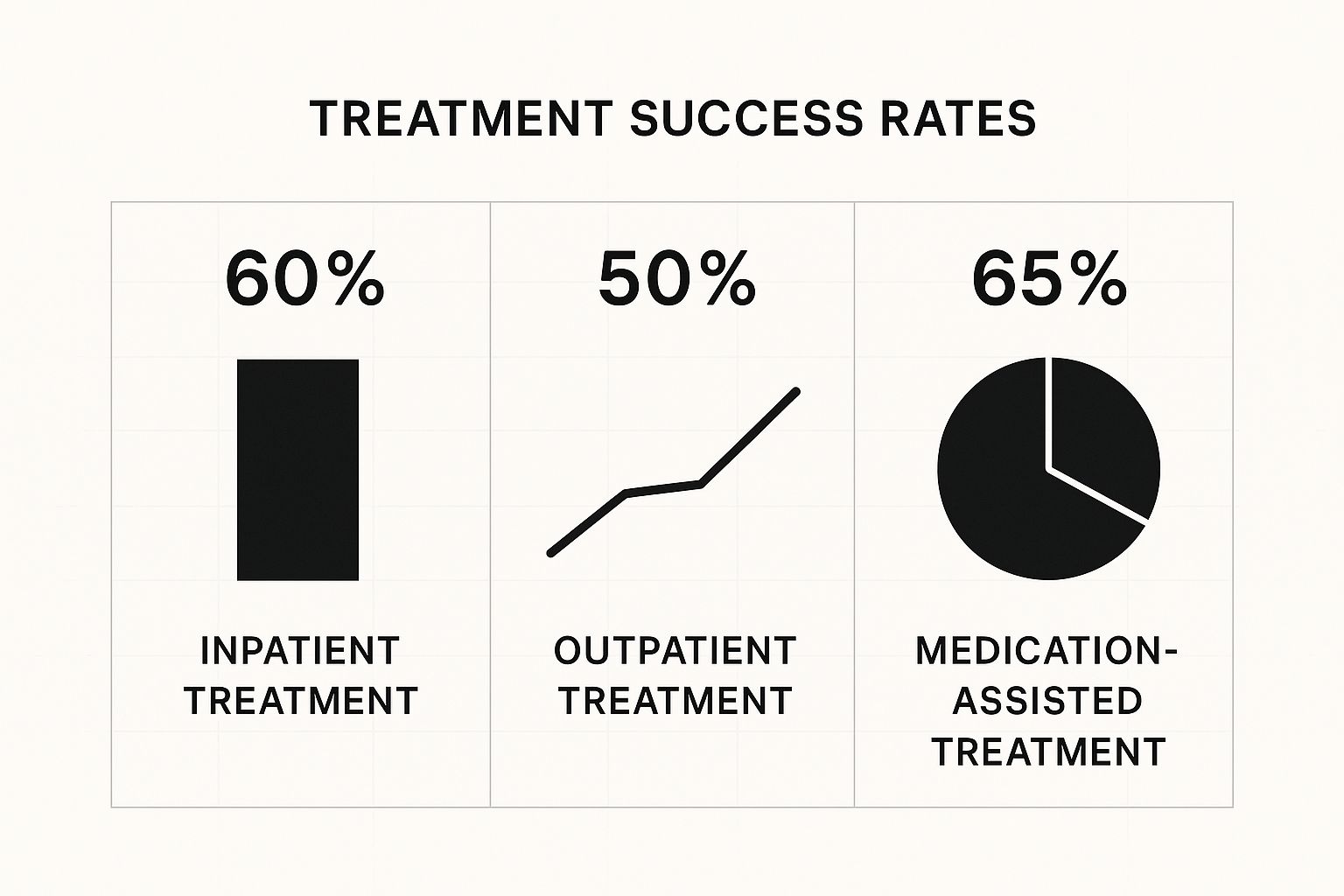
As you can see, both inpatient and outpatient care show positive outcomes. It’s also worth noting that Medication-Assisted Treatment (MAT), which can be part of either program, often has a slightly higher average success rate.
Situational Guide to Inpatient vs Outpatient Treatment
Making this choice can feel overwhelming. To simplify things, I’ve put together this table to help you see which environment might align better with different personal situations.
| Consideration | Best Suited for Inpatient | Best Suited for Outpatient |
|---|---|---|
| Severity of Addiction | Severe, long-term substance use; high risk of dangerous withdrawal | Mild to moderate substance use; motivated to change. |
| Home Environment | Unstable, triggering, or lacks a strong support system. | Stable, supportive, and safe. |
| Co-occurring Disorders | Significant mental health conditions (e.g., severe depression). | Mild mental health conditions; already seeing a therapist. |
| Previous Treatment Attempts | Multiple past relapses; previous outpatient attempts were unsuccessful. | First time seeking treatment or have a history of maintaining sobriety. |
| Daily Responsibilities | Able to take time away from work, school, or family duties. | Cannot leave job, school, or caregiving responsibilities. |
| Level of Medical Need | Requires 24/7 medical supervision and access to care. | Medically stable; does not require round-the-clock monitoring. |
This guide is a starting point. The best placement is always one that considers you as a whole person—your addiction history, mental health, home life, and responsibilities.
“The most successful treatment placement is one that acknowledges the whole person—their addiction severity, mental health status, home environment, and personal responsibilities. The goal is to create an environment where the individual feels supported enough to heal, not just forced into a generic program.”
Ultimately, the decision boils down to three things: safety, support, and structure. If your current environment puts your sobriety at risk, inpatient care offers a necessary sanctuary. If you have a solid support system but need professional guidance to navigate recovery, an outpatient program provides a practical path forward.
Effectiveness of Different Therapeutic Models

Beyond the setting inpatient or outpatient the specific therapeutic model used is one of the biggest factors driving addiction treatment success rates. It’s a mistake to think all therapies are the same or that one approach works for every person and every substance.
Real, lasting recovery often begins when we match the right therapy to an individual’s unique needs, their psychological makeup, and the specifics of their addiction. This requires looking deeper than just a program’s name and understanding how each therapy actually works. A person grappling with past trauma needs a fundamentally different approach than someone whose main struggle is navigating social triggers.
Cognitive and Dialectical Behavioral Therapies
Cognitive Behavioral Therapy (CBT) is a cornerstone of modern addiction treatment, and for good reason. It’s one of the most studied and validated approaches out there. The core idea of CBT isn’t just to talk through problems; it’s to give people practical skills to identify and rewire the destructive thinking that fuels substance use.
For instance, someone might learn to catch the thought, “It’s been a horrible day, I need a drink,” and actively replace it with a healthier action, like calling a sponsor or hitting the gym. This focus on real-world coping skills is why CBT is so powerful for preventing relapse long after a person leaves formal treatment.
Dialectical Behavior Therapy (DBT) is a more specialized offshoot of CBT. It was initially designed for borderline personality disorder but has proven incredibly effective for addiction, especially when other mental health issues are in the mix. DBT hones in on four critical skills: mindfulness, tolerating distress, regulating emotions, and building healthier relationships. It’s a game-changer for people who turn to substances to escape overwhelming emotional pain. You can find a more complete rundown of these and other methods by exploring different https://addictionhelplineamerica.com/types-of-addiction-therapy/.
Medication-Assisted Treatment (MAT)
Medication-Assisted Treatment (MAT) has become an essential tool in our fight against the opioid epidemic. It works by combining FDA-approved medications with counseling and behavioral therapies. Medications like methadone or buprenorphine (often known by the brand name Suboxone) help normalize brain chemistry, curb cravings, and block the euphoric effects of opioids.
“It’s crucial to understand that MAT is not “trading one drug for another.” It is a proven medical intervention that saves lives by dramatically reducing the risk of a fatal overdose. Studies show that MAT can cut this risk by about 50%, giving individuals the stability they need to do the deep psychological work of recovery.”
The power of MAT is especially evident with the rise of fentanyl. Emerging research shows methadone is particularly effective for fentanyl users. One study found that an impressive 53% of patients who were using fentanyl when they started treatment were still engaged in that treatment a full year later. In addiction recovery, staying in treatment is a massive indicator of long-term success.
Holistic and Complementary Approaches
Holistic therapies work on the entire person—mind, body, and spirit. While they aren’t typically standalone treatments for addiction, they serve as powerful complements to evidence-based models like CBT or MAT. Think of them as supportive practices that strengthen a person’s overall well-being and resolve.
A few common holistic approaches include:
- Yoga and Meditation: These practices are fantastic for reducing the stress and anxiety that so often trigger a relapse. They build mindfulness, helping a person stay grounded in the present moment instead of being overwhelmed by cravings.
- Art and Music Therapy: Sometimes, words aren’t enough. Creative therapies offer a way to express and process complex feelings tied to trauma and addiction without having to talk directly about them.
- Nutritional Counseling: Addiction takes a heavy toll on the body. Learning to eat well helps restore physical health, which in turn improves mood and energy, building a stronger foundation for the mental work of recovery.
By weaving these different approaches together, a treatment center can build a truly personalized recovery plan. This customized strategy is what ultimately leads to higher and more durable addiction treatment success rates.
Personal Factors That Shape Recovery Outcomes
While it’s essential to compare different treatment programs and therapies, addiction treatment success rates aren’t just about the facility. The best programs understand that recovery is a deeply personal journey, and individual circumstances play a massive role in whether someone stays sober for the long haul.
Success is ultimately shaped by what happens both inside and outside the walls of a treatment center. Things like how long a person stays in treatment, the strength of their aftercare plan, and whether they’re also dealing with mental health issues are incredibly influential. True recovery depends on the entire ecosystem of support built around a person.
The Critical Role of Treatment Duration
If there’s one thing the research consistently shows, it’s the direct link between the length of treatment and positive outcomes. A 30-day program can be a great way to get stabilized, but longer stays are almost always connected to higher rates of long-term sobriety.
In fact, the National Institute on Drug Abuse (NIDA) has found that treatment lasting less than 90 days has limited effectiveness. More time allows a person to really dig in and address deep-seated behaviors, practice new coping skills in a safe space, and solidify their commitment to recovery before facing the real world again.
“A longer treatment stay isn’t about prolonging the process; it’s about providing enough time for the brain and behavior to heal. It allows new, healthy habits to take root, making them more resilient against the pressures and triggers of everyday life.”
Integrating Mental Health and Aftercare
For many people, substance use is a way to self-medicate underlying issues like depression, anxiety, or PTSD. If these co-occurring conditions aren’t treated right alongside the addiction, the risk of relapse skyrockets. Integrated treatment that addresses both mental health and substance use at the same time simply gets better results.
What happens after the initial program is just as critical. A solid aftercare plan is the bridge from the structured, safe environment of rehab back to the real world. This isn’t just a suggestion; it’s a lifeline. A good plan often includes:
- Sober living arrangements: A substance-free home that offers structure and peer support.
- Ongoing therapy: Continuing with a therapist to reinforce coping strategies and navigate challenges.
- Support groups: Programs like AA, NA, or SMART Recovery provide invaluable peer connection and accountability.
- Alumni programs: Staying connected to the treatment center and others who have been through it creates a lasting community.
The Power of a Strong Support System
No one gets through recovery alone. A strong, positive support system is one of the most powerful tools a person can have. This network can be family, friends, or peers who genuinely understand the journey. Digging into the importance of support systems in recovery really highlights how these connections build resilience.
Even with the clear benefits, huge barriers to getting help still exist, and most people who need treatment never receive it. But the numbers don’t lie: people do recover from addiction with specialized care. A supportive network is often the very thing that gives someone the courage to finally seek and complete the treatment they desperately need.
How to Evaluate a Treatment Center’s Claims

Now that we’ve broken down what “success” really means in addiction recovery, you can start looking at treatment centers with a more critical eye. When you’re vetting a facility, it’s not enough to just accept a big, splashy number they advertise. You have to dig a little deeper and ask the right questions to understand the real story behind their addiction treatment success rates.
The first thing to do is get curious about their methods. What, exactly, are they calling “success”? Does it just mean someone finished the program, or are they talking about sobriety a full year after treatment? A quality, reputable center will have no problem explaining how they track outcomes and what their stats actually mean. If you get vague, roundabout answers, that’s a major warning sign.
Questions to Ask an Admissions Counselor
When you call a treatment center, remember you’re in the driver’s seat. Think of it as an interview—you’re the one deciding if they are the right fit, and they need to earn your trust. Showing up prepared with a list of questions is the best way to do this. For a more exhaustive checklist, check out our complete guide on how to choose the right rehab.
To get the conversation started, here are a few essential questions:
- Data Collection: “How do you keep in touch with alumni, and how long do you track their progress after they leave?”
- Definition of Success: “When you calculate your success rate, what specific outcomes are you measuring? Is it strictly about abstinence, or do you include other factors?”
- Third-Party Verification: “Do you have an independent, outside organization that verifies your outcome data?”
- Accreditation: “Are you accredited by a major body like The Joint Commission or CARF?”
“A facility’s willingness to openly discuss their data is often as important as the data itself. Transparency indicates confidence in their programs and a commitment to ethical practices, while secrecy or evasive answers suggest their marketing may not match reality.”
Identifying Red Flags and Empty Promises
Beyond asking direct questions, you also need to tune your radar for common red flags. Be incredibly wary of any center that makes an outright guarantee of success or promises a “cure” for addiction. That’s just not how it works. Addiction is a chronic disease, and the goal is long-term, effective management—not a quick, one-and-done fix.
Another huge red flag is a lack of proper licensing or accreditation. These certifications are your assurance that a facility meets critical standards for safety, quality of care, and staff qualifications. If a center can’t or won’t provide this information upfront, it’s a clear sign to walk away. This is one of the most important decisions you can make, and doing your homework is the best way to protect yourself from misleading claims and subpar care.
Your Questions Answered
Why do success rates vary so much between rehab centers?
You’ve probably noticed that addiction treatment success rates can look wildly different from one facility to the next. This isn’t just marketing spin; it’s because there’s no single, universally accepted way to measure success.
Some centers might define “success” as simply completing a 30-day program. Others track sobriety for a full year after treatment. The numbers are also heavily influenced by who they’re treating—a facility working with clients who have co-occurring mental health disorders might have different outcomes than one that doesn’t. Always ask a potential center how they measure their own success; transparency is a very good sign.
Does relapse mean treatment failed?
Not at all. In fact, most clinicians in the field view relapse as a common and sometimes expected, part of the recovery journey. It’s not a sign of failure, but rather an indication that the treatment plan needs adjustment.
The best programs anticipate this possibility. They equip people with strong relapse prevention strategies and have clear pathways to get them back on track quickly if a setback happens. Think of it less as a failure and more as a bump in the road.
How important is aftercare?
Aftercare is absolutely critical. Think of inpatient rehab as the intensive, foundational work, but recovery is a lifelong process. Ongoing support through aftercare like therapy, support groups, or sober living arrangements is what solidifies those new habits and truly boosts the chances of long-term sobriety.
The transition back to daily life can be jarring, and aftercare provides the safety net needed to navigate it successfully.
What about the financial aspect?
Understanding the investment is a huge part of the planning process. Costs can vary significantly based on the type of facility, the level of care, and the length of stay. For a complete breakdown, you can learn more about how much rehab costs in our detailed guide.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.












