
Medication Assisted Treatment (MAT) is a powerful, evidence-based approach to treating substance use disorders. It’s not just about medication—it’s a comprehensive strategy that combines FDA-approved medications with professional counseling and behavioral therapies.
Think of it as a way to quiet the storm. MAT helps stabilize brain chemistry, ease the intense physical cravings, and block the rewarding effects of alcohol or opioids. This gives individuals the breathing room they need to fully engage in their recovery and start rebuilding their lives.
Understanding Medication Assisted Treatment

To really get what MAT is, it helps to view addiction as the chronic disease it is. You wouldn’t ask someone with diabetes to just “will away” their need for insulin, or someone with heart disease to just “think” their blood pressure down. It’s the same principle here. Addiction physically changes the brain’s circuits for reward, stress, and self-control, and MAT is designed to address these biological changes head-on.
The goal is simple: restore normal brain function and give you relief from the relentless cycle of withdrawal and cravings. By creating this stable foundation, MAT empowers you to tackle the psychological and social sides of addiction in therapy, where the real, lasting change happens.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
The Three Pillars of Medication Assisted Treatment
A truly effective MAT program isn’t just a prescription; it’s a “whole-patient” approach built on three integrated pillars. Each one plays a critical role, and it’s how they work together that makes this treatment so successful for long-term recovery.
Here’s a breakdown of how these components team up:
The Three Pillars of Medication Assisted Treatment
| Component | Role in Recovery | Practical Example |
|---|---|---|
| FDA-Approved Medications | Stabilizes brain chemistry, blocks euphoric effects of drugs, and relieves cravings and withdrawal. | A patient receiving a daily dose of methadone or a monthly injection of Vivitrol to manage opioid dependence. |
| Counseling & Therapy | Addresses underlying emotional issues, teaches coping skills, and helps rebuild relationships. | Attending weekly cognitive-behavioral therapy (CBT) sessions to identify triggers and develop healthy responses. |
| Support Systems | Provides accountability, community, and encouragement from peers and professionals. | Participating in group therapy sessions or being actively involved in a 12-step program alongside medical treatment. |
Now, let’s clear up one of the biggest myths out there. A common misconception is that MAT just swaps one drug for another. That couldn’t be further from the truth. These are therapeutic medications, prescribed and carefully monitored by doctors in a controlled, clinical setting.
“The goal is not to produce a “high” but to normalize bodily functions, reduce harm, and create the opportunity for long-term healing. It is a medically supervised treatment, not a crutch.”
This approach finally treats addiction as the complex medical condition it is—one that demands a multi-layered plan. By calming the physical chaos that addiction creates, MAT opens the door for people to do the hard but essential work of rebuilding their lives. It provides the stability you need to make lasting behavioral changes and achieve genuine, long-term wellness.
How MAT Restores Balance to the Brain and Body
To really get what medication-assisted treatment does, picture your brain as a complex electrical panel. When someone is struggling with chronic substance use, particularly with opioids, it’s like a power surge has been sent through the system, hitting the “reward” and “pleasure” circuits over and over again. After a while, the whole panel overloads, fries some wires, and rewires itself to need that intense signal just to function.
This isn’t a failure of willpower; it’s a physical change in the brain’s wiring. The body’s natural production of feel-good chemicals, like endorphins, slows to a crawl because it’s being flooded by much stronger, artificial chemicals from the substance. Take the substance away, and the system crashes hard. This crash triggers excruciating withdrawal symptoms and powerful, deep-seated cravings. The brain is literally screaming for the one thing it thinks it needs to survive.
Hitting the Neurological Reset Button
Medication-assisted treatment works like a skilled technician coming in to carefully repair that damaged electrical panel. The medications used in MAT are designed to interact with the very same receptors that addictive drugs target, but they do it in a far more controlled and safe way. This is the crucial difference that makes MAT a medical treatment, not just a substitute.
Here’s another way to think about it: instead of the chaotic, destructive flood from substance use, MAT provides a steady, low-level electrical current. It’s just enough to keep the system from shorting out (which stops withdrawal) but not nearly strong enough to produce the euphoric “high” that fuels addiction. It’s all about creating neurological stability.
This is exactly why MAT is so effective. By calming the physical chaos, the medication gives a person the mental and emotional breathing room to start the real work of recovery. When they’re not constantly battling cravings and withdrawal, they can finally engage in therapy, heal relationships, and build a new life.
Two Different Tools for the Same Job
Not all MAT medications work the same way, which is great because it allows treatment to be tailored to a person’s unique situation. The two most common medications for opioid use disorder, buprenorphine and naltrexone, are perfect examples of these different—but equally effective—approaches.
- Buprenorphine: This medication is what’s known as a partial agonist. It latches onto opioid receptors and activates them, but only partially. This “partial” action is just enough to fool the brain into thinking its needs are being met, which stops withdrawal and quiets cravings. But here’s the key: it has a “ceiling effect.” After a certain dose, taking more doesn’t increase the effect, which dramatically lowers its potential for misuse and overdose.
- Naltrexone: This medication is an antagonist. Instead of turning the receptors on, it completely blocks them. Think of it as putting a protective lock over the buttons on the electrical panel. If someone uses opioids while on naltrexone, the drug can’t connect to the brain’s receptors, so the euphoric effect is blocked. This helps to finally break the cycle of use and reward.
The choice between these medications is a clinical one, based on a person’s medical history, the specifics of their substance use, and their recovery goals. It’s a decision made with a qualified healthcare provider after a thorough assessment.
“The core principle of what is medication assisted treatment is that it addresses the physical disorder first. By stabilizing the brain’s chemistry, MAT builds a solid foundation for the psychological and emotional work of lasting recovery.”
Ultimately, MAT gives the brain and body the time and space they need to heal. It lifts the immense weight of physical dependency, freeing a person from the relentless cycle of craving and relapse. This stability reinforces the truth that addiction is a treatable medical condition—and that with the right support, recovery isn’t just possible, it’s sustainable.
A Closer Look at Common MAT Medications
To really grasp what medication-assisted treatment is, you have to understand the tools in the toolbox. There’s no one-size-fits-all pill. Instead, doctors can choose from several FDA-approved medications to design a treatment plan that fits a person’s unique situation, biology, and recovery goals. Each one works differently to help restore balance and stability.
These medications are generally grouped by how they interact with the brain’s receptors. This diagram gives a great visual overview.
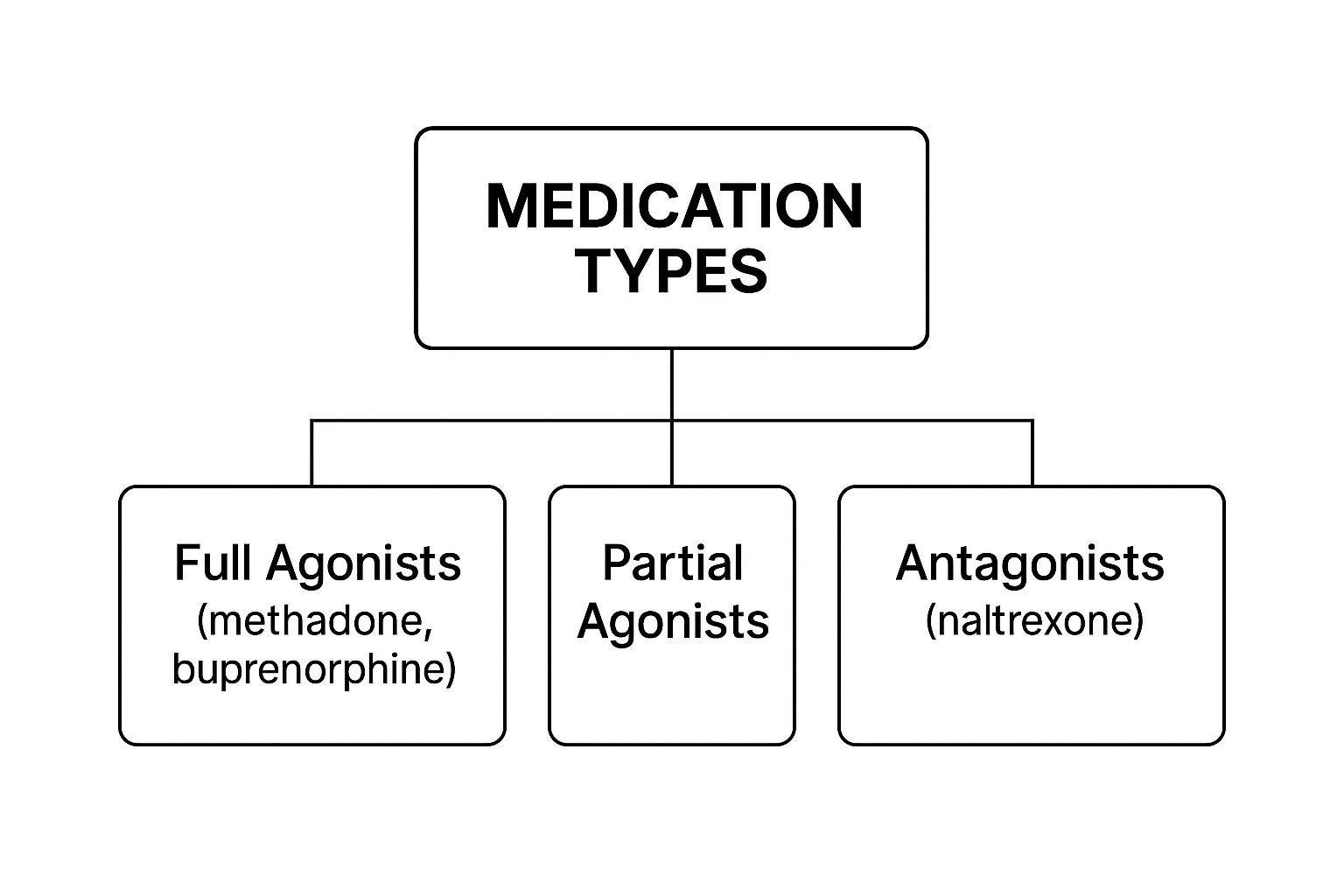
As you can see, the drugs are classified as full agonists, partial agonists, or antagonists. That fancy language just describes how they work in the brain. Let’s break down what that means for the most common options.
Methadone: The Time-Tested Full Agonist
Methadone is one of the oldest and most well-known medications for opioid use disorder (OUD). It’s a full opioid agonist, which means it binds to the same opioid receptors in the brain that other opioids do.
But here’s the key difference: methadone is slow-acting and long-lasting. This allows it to stop withdrawal symptoms and powerful cravings in their tracks without producing the intense, euphoric high that drives addiction. It provides relief and stability.
Because of its specific nature, methadone treatment is highly regulated. It can only be dispensed through federally certified opioid treatment programs (OTPs), which often means patients visit a clinic daily for their dose. This built-in structure provides a high level of accountability and support, which can be exactly what someone needs at the start of their recovery. To learn more, check out our guide on why methadone is used for drug addicts.
Buprenorphine: The Flexible Partial Agonist
Buprenorphine offers a different, more flexible path. It’s a partial opioid agonist, so it also activates opioid receptors, but not to the same extent as a full agonist like methadone.
This creates a “ceiling effect.” After a certain dose, taking more of the drug doesn’t increase its effects. This is a game-changer because it dramatically lowers the risk of misuse and overdose, making it a much safer option for many.
You’ll often see buprenorphine combined with naloxone (an antagonist) in products like Suboxone. The naloxone is a safeguard; it only becomes active if someone tries to crush and inject the medication, which helps deter misuse.
“One of the biggest wins for buprenorphine is how accessible it is. Unlike methadone, certified doctors can prescribe it from a regular office setting. This allows patients to have take-home prescriptions, giving them more freedom and autonomy in their recovery.”
The impact of these medications is enormous. The global market for treatments like Suboxone and methadone is valued at around $5 billion, a figure that speaks volumes about the widespread need for effective OUD solutions.
Naltrexone: The Protective Antagonist
Naltrexone works in a completely different way from the others. It’s an opioid antagonist, which means it works like a shield. It completely blocks opioid receptors.
If a person on naltrexone uses opioids, they won’t feel anything. The drug simply can’t attach to the receptors to produce a high. This effectively breaks the psychological link between using the substance and feeling a reward.
Naltrexone is non-addictive and has no potential for misuse. It comes as a daily pill or as a once-a-month, long-acting injection (Vivitrol), making it a great option for people who are highly motivated and have already completed detox.
Medications for Alcohol Use Disorder
MAT isn’t just for opioids. It’s also an incredibly effective strategy for treating alcohol use disorder (AUD). Three main medications are used here:
- Naltrexone: Just like with opioids, it helps reduce the rewarding, pleasurable effects of alcohol. This can significantly cut down on heavy drinking days and curb cravings.
- Acamprosate: Chronic drinking throws the brain’s delicate chemical balance out of whack. Acamprosate helps restore that balance, easing long-term withdrawal symptoms like anxiety, restlessness, and insomnia that often lead people back to drinking.
- Disulfiram: This medication creates a powerful deterrent. If someone taking disulfiram drinks alcohol, they will have a severe physical reaction, including nausea, flushing, and heart palpitations. It works by creating a strong, negative association with drinking.
Each of these provides a different kind of support, allowing a healthcare provider to tailor the treatment to a person’s specific health profile, drinking habits, and recovery goals.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
The Life-Changing Benefits of an Integrated MAT Approach

Medication-assisted treatment is far more than just a clinical strategy; it’s a lifeline that creates real, tangible change. The benefits ripple out, touching every part of a person’s life. By providing a stable foundation, an integrated MAT approach gives individuals the chance to rebuild their health, mend relationships, and reclaim their futures. Time and again, the data confirms that MAT is one of the most effective tools we have for overcoming substance use disorders.
MAT works by quieting the relentless noise of physical withdrawal and cravings. This gives a person the mental and emotional breathing room needed to do the deeper work of recovery. Think of it like trying to have a serious conversation during a rock concert. It’s nearly impossible. MAT turns down the volume, creating the calm needed for clarity and healing to begin.
Measurable Improvements in Safety and Health
The first and most critical benefit of MAT is its proven ability to save lives. The statistics are undeniable. For people with opioid use disorder, participating in MAT dramatically lowers the risk of a fatal overdose. It’s that simple.
This is because the medications are prescribed by a doctor and carefully controlled, which removes the need to turn to dangerous street drugs of unknown potency. Beyond preventing overdoses, MAT also leads to a sharp decline in behaviors that transmit infectious diseases like HIV and hepatitis C.
But the positive health impacts don’t stop there. MAT helps people achieve:
- A dramatic decrease in illicit drug use, as the medications effectively manage the cravings that fuel addiction.
- A significant reduction in criminal activity, since the compulsion to obtain drugs is no longer the driving force.
- Improved birth outcomes for pregnant individuals with opioid use disorder, making it a safe and recommended path for the health of both parent and child.
Building a Foundation for Lasting Recovery
While the medical benefits are profound, the personal impact is just as powerful. Physical stability is the key that unlocks a person’s ability to truly engage with the other essential parts of their recovery journey.
Imagine trying to build a house during an earthquake. It’s a futile effort. Active addiction is a constant earthquake for the mind and body. MAT calms the shaking ground, giving you the stability to lay a new foundation, one piece at a time.
“This stability is what makes genuine progress possible. It allows a person to shift their focus from just surviving to actively building a meaningful life, free from substance dependence.”
This is where the “assisted” part of medication-assisted treatment really shines. The medication provides the support needed to fully benefit from crucial psychological and social therapies. You can learn more about the vital role of therapy in addiction recovery in our detailed guide.
Improving Social Functioning and Quality of Life
One of the most incredible outcomes of a successful MAT program is watching someone’s entire quality of life improve. A key sign of success is treatment retention; studies consistently show that people in MAT programs stick with their treatment plan far longer than those in non-medicated programs.
This consistency gives people the space to mend broken relationships, reconnect with their communities, and start chasing goals that once felt impossible. One of the biggest benefits is the ability to find and keep a job. When a person is no longer consumed by addiction, they can become a reliable employee, which brings financial stability and a renewed sense of purpose.
Medication-assisted treatment is now a globally recognized standard for care, and its market is growing as more people see its value. The global MAT market was recently valued at over USD 10 billion. This growth is driven by a sobering reality: an estimated 286 million people used drugs worldwide in a recent year, a staggering 26% increase over the previous decade. These numbers highlight the urgent need for accessible, evidence-based care like MAT.
Debunking Common Myths About MAT
Even though it’s a life-saving, evidence-based approach, medication-assisted treatment is still surrounded by a cloud of stigma and misinformation. These damaging myths often create very real barriers, preventing people who desperately need help from ever seeking it. It’s critical that we address these falsehoods head-on to foster an environment where recovery can actually thrive.
Let’s confront some of the most persistent and harmful myths with clear, factual explanations. Getting to the truth behind MAT can empower patients, their families, and entire communities to make decisions based on medical science—not on fear or judgment.
Myth 1: It Is Just Trading One Addiction for Another
This is probably the most common and destructive myth out there. It comes from a basic misunderstanding of the massive difference between physical dependence and addiction.
Addiction is a behavioral and psychological disorder defined by compulsive, out-of-control drug use despite severe negative consequences. Physical dependence, on the other hand, is a predictable physiological response to a medication. Your body simply adapts to its presence and expects it to be there.
Think of it like this: someone with high blood pressure is physically dependent on their medication to keep their levels stable. No one would ever say they are “addicted” to their blood pressure pills. In the same way, a person in a MAT program takes a prescribed medication under strict medical supervision to stabilize their brain chemistry so they can function normally again.
“The entire point of MAT is to stop the compulsive, destructive behavior of addiction—not to substitute it with a new one. It uses medication to treat a chronic brain disease, giving a person the chance to get back in the driver’s seat of their own life.”
Myth 2: It Is a Crutch for People Who Lack Willpower
This myth is deeply harmful because it frames addiction as a moral failing instead of the chronic medical condition that it is. Substance use physically alters the brain’s structure and function, especially in the areas that control reward, stress, and self-control. Overcoming these profound biological changes isn’t just a matter of “being strong.”
Asking someone with a severe opioid use disorder to just quit without medical support is like asking someone with a broken leg to run a marathon. It’s an impossible task. MAT provides the necessary medical support—like a cast for that broken bone—so the real healing can finally begin. It works by correcting the neurochemical imbalances that fuel overwhelming cravings and withdrawal.
By stabilizing the brain, MAT gives individuals the mental and physical capacity to fully engage in counseling and therapy. It’s the tool that makes the hard work of recovery possible, not a shortcut to avoid it.
Myth 3: It Is Only a Short-Term Fix
Another common falsehood is that MAT is just a temporary patch that doesn’t lead to true, long-term recovery. In reality, the exact opposite is true. MAT is recognized as a long-term treatment strategy for a chronic disease.
How long someone stays in treatment is a deeply personal decision made between them and their doctor. For some, it might be for a year or two. For others, it could be indefinite, much like managing other chronic conditions like diabetes or heart disease. There is absolutely no set timeline.
The evidence couldn’t be clearer: staying in MAT programs for an adequate amount of time leads to far better outcomes, including:
- Reduced risk of overdose
- Lower rates of illicit drug use
- Increased treatment retention
- Improved ability to gain and maintain employment
Rushing to stop medication-assisted treatment can be incredibly dangerous and significantly increases the risk of relapse. The decision to taper off is a major medical one that should only be made when a person is stable and ready, all with the careful guidance of a healthcare professional. This is about sustainable wellness, not a quick fix.
How to Find and Begin Medication-Assisted Treatment

Taking that first step toward recovery can feel like staring up at a mountain. It’s a huge decision, but finding the right support is much more straightforward than you might think. Getting started with medication-assisted treatment just means having a clear, actionable roadmap—and it all begins with connecting to a qualified provider who can guide you with medical expertise and genuine compassion.
Help is out there. You have several different avenues for finding MAT providers, so you can choose the one that feels right for you.
- Certified Physicians: Many primary care doctors are now certified to prescribe MAT medications like buprenorphine right from their own offices.
- Dedicated Clinics: Specialized clinics called Opioid Treatment Programs (OTPs) provide structured care and often dispense medications like methadone.
- Telehealth Services: Reputable online platforms now connect patients with MAT providers virtually, offering a convenient and private way to get the care you need.
What to Expect at Your First Appointment
Your first appointment is simply a comprehensive assessment—it’s not a test or an interrogation. The provider’s only goal is to understand your unique situation so they can build the safest, most effective treatment plan for you. You can expect a thorough, judgment-free conversation about your medical history and your experience with substance use. This is all about your health and well-being.
This initial meeting is also your time to ask questions and bring up any concerns you have. A good provider will walk you through exactly how the recommended medication works, what its benefits are, and any potential side effects.
It’s also common for people to be dealing with co-occurring conditions like anxiety or PTSD. A great program will be equipped to address these needs simultaneously. In some cases, inpatient care is the best option for focused support, a topic we cover more in our guide to PTSD inpatient treatment programs.
Choosing an Integrated Program
The most successful MAT programs give you more than just a prescription. Real, lasting recovery happens when medication is paired with counseling and strong support services. When you’re looking for a provider, always ask about their approach to integrated care.
“A program that includes therapy and support services treats the whole person, not just the physical symptoms of addiction. This combination is the key to building a strong foundation for long-term wellness.”
The demand for these effective, integrated programs is skyrocketing. The global medication-assisted therapy market is projected to grow from over USD 10 billion to more than USD 21 billion by 2032. This massive growth shows that the world is recognizing the true value of MAT and the urgent need for proven solutions that blend medication with therapy.
Figuring out insurance and costs can feel like another hurdle, but there are plenty of options. Most insurance plans, including Medicaid, cover MAT. The team at Addiction Helpline America is here to help you understand your benefits and connect you with affordable, high-quality providers.
Taking that first step is the most important one you’ll make. We’re here to help you start your journey with confidence.
Call Now – Your Journey to Recovery Begins Today!

Take the first step towards a healthier life! Call now to connect with our compassionate team and start your recovery journey today. Your path to healing awaits!
Our recovery specialists are available 24/7 to provide support, and all calls are confidential and free. Reach out anytime – we’re here to help!
Frequently Asked Questions About MAT
When you’re considering something as important as medication-assisted treatment, it’s completely normal to have a lot of questions. Getting clear, straightforward answers is the best way to feel confident about your next steps. Let’s walk through some of the most common questions people have about MAT.
How Long Does Medication-Assisted Treatment Last?
This is one of the first things people ask, and the honest answer is: there is no set timeline. MAT isn’t a quick fix; it’s a long-term strategy for managing a chronic health condition. Think of it like managing diabetes or high blood pressure—some people may use medication for a few years to find stability, while others might continue it indefinitely to stay healthy.
The decision to eventually reduce or stop the medication is a major medical choice. It’s something that must be done carefully, in partnership with your doctor, and based entirely on your personal stability and progress. Stopping suddenly is incredibly risky and is strongly discouraged because it can lead to severe withdrawal and a high chance of relapse.
Is MAT Only for Opioid Addiction?
While MAT is most famous for treating opioid use disorder (OUD), it is also a highly effective, FDA-approved treatment for alcohol use disorder (AUD). Medications like naltrexone, acamprosate, and disulfiram are powerful tools for helping people cut back or stop drinking.
For instance, naltrexone works by blocking the pleasurable feelings alcohol can cause, which helps dial down cravings. Disulfiram works differently, creating a very unpleasant physical reaction if someone drinks, making it a strong deterrent. Just like with opioids, these medications work best when they’re part of a full treatment plan that includes therapy and solid support.
Can I Go to Therapy During MAT?
Yes, absolutely—in fact, it’s essential. The whole point of MAT is to combine medication with therapy. It’s the one-two punch that makes recovery stick.
“The medication helps stabilize your brain and body, which clears the way for you to do the real, meaningful work in therapy.”
Think of the medication as the foundation. It provides the physical and mental stability you need to dig into the behavioral and emotional roots of addiction in counseling. This is where you develop the new coping skills needed for a lasting recovery.
While some support groups have been slow to embrace MAT, the medical community’s understanding has grown, and most now recognize its value. It’s also crucial for family members to get educated. Learning how to support a loved one is a huge part of the process, and our guide on how to help a drug addict and support their recovery is a great place to start.
If you or someone you care about is struggling, remember that effective help is available. The team at Addiction Helpline America is here to connect you with trusted, compassionate professionals who can guide you on the path to recovery. Take the first step toward a healthier life by visiting Addiction Helpline America today.
Our helpline is 100%
free & confidential
If you or someone you care about is struggling with drug or alcohol addiction, we can help you explore your recovery options. Don’t face this challenge alone—seek support from us.
Programs
Resources
Will my insurance
cover addiction
treatment?
We're ready to help
Find the best
drug or alcohol treatment
center
Are you or a loved one struggling with addiction? Call today to speak to a treatment expert.















